The term Wolf′s isotopic response refers to the appearance of a new skin disease at the site of an already healed, unrelated disease. In most cases, the initial disease is herpes zoster. Different diseases may subsequently develop on the same site. The most common isotopic responses are granulomatous and lichenoid reactions, infiltrations of hematologic diseases, skin tumors, and infections. The pathogenesis of these skin reactions is unknown. It has been suggested that viral infection may alter local skin immunity; this would favor hyperreactivity, leading to inflammatory processes, or local immunosuppression, leading to tumor infiltrations or infections.
Materials and methodsWe performed a retrospective study of 9 patients diagnosed with Wolf's isotopic response in the dermatology department of Hospital Donostia in San Sebastian, Spain. Five patients had B-cell chronic lymphocytic leukemia, 2 had a non-Hodgkin lymphoma, and 1 had ovarian carcinoma.
ResultsThe initial disease was herpes zoster in 7 cases, and chickenpox and herpes simplex in the other 2 cases. The second disease was granulomatous dermatitis in 4 cases, lichenoid dermatitis in 2 cases, infiltration by B-cell chronic lymphatic leukemia in 2 cases, and infiltration by systemic non-Hodgkin lymphoma in 1 case. In the last case, the skin lesions were the first sign of the lymphoma.
ConclusionsWe highlight the need to biopsy these second lesions in order to rule out tumor infiltrations, which were more frequent than expected in our series.
El fenómeno isotópico de Wolf se define como la aparición de una enfermedad cutánea nueva en la misma localización donde previamente ha acontecido otra, ya curada, y con la que no guarda ninguna relación.
En la mayoría de los casos, la primera dermatosis es un herpes zóster (HZ). Posteriormente, en esta localización pueden desarrollarse diversos procesos dermatológicos, fundamentalmente reacciones granulomatosas y liquenoides, infiltraciones específicas de enfermedades hematológicas, tumores cutáneos o infecciones.
La patogenia de estas reacciones cutáneas es desconocida. Se ha sugerido que la infección viral pudiera alterar la inmunidad cutánea local, favoreciendo una hiperreactividad que determinaría el desarrollo de procesos inflamatorios, o una inmunosupresión local, que condicionaría la aparición de infiltraciones tumorales o infecciones.
Material y métodosEstudio retrospectivo de 9 pacientes diagnosticados de fenómeno isotópico de Wolf en el Servicio de Dermatología del Hospital Donostia. Cinco pacientes tenían una leucemia linfática crónica-B (LLC-B), 2 un linfoma no Hodgkin y una un carcinoma de ovario.
ResultadosLa dermatosis primaria en 7 casos fue un HZ, en los otros 2 una varicela y un herpes simple. Respecto a las dermatosis secundarias se diagnosticaron 4 casos de dermatitis granulomatosa, 2 de dermatitis liquenoide, 2 de infiltración específica por LLC-B y uno de infiltración por un linfoma no Hodgkin sistémico. En este último caso las lesiones cutáneas fueron el primer signo del linfoma.
ConclusionesDestacamos la necesidad de biopsiar este tipo de lesiones para descartar infiltraciones específicas tumorales, ya que en nuestra casuística fueron más frecuentes de lo esperado.
Wolf's isotopic response is defined as the appearance of a new skin disease at site of a previous, already healed, unrelated disease.
In 1876, Koebner1 described the isomorphic response in reference to the appearance of lesions of a previously existing skin disease on skin that had been subjected to injury. Then, in 1995,1 Wolf coined the term isotopic response.
In most cases, the initial dermatosis is herpes zoster, but the condition has also been described following herpes simplex, varicella, and thrombophlebitis.2 After the initial skin disease has healed, a wide variety of skin diseases may present on the same site; these are mainly granulomatous and lichenoid reactions, infiltrations by hematologic malignancies, skin tumors, and infections.3
The objective of our study was to collect cases of the isotopic response diagnosed in our department and to evaluate their particular clinical characteristics.
Materials and MethodsWe performed a retrospective study of all cases of Wolf's isotopic response diagnosed in the dermatology service of Hospital Donostia, San Sebastian, Spain in the 20 years, from 1990 to 2010. A total of 9 cases were collected and are shown in Table 1, which specifies the age, sex, relevant patient history, initial dermatosis and site, second dermatosis, time elapsed between the 2 dermatoses, and the treatment carried out in each case.
Characteristics of the Cases of Wolf's Isotopic Response.
| Case no.° | Sex/Age | History | Initial Dermatosis | Location | Time | Second Dermatosis | Treatment of Initial Dermatosis | Treatment of Second Dermatosis |
| 1 | F/63 | Ovarian cancer | Herpes zoster | L2 | 1 mo | Granulomatous dermatitis | Oral valaciclovir | Topical corticosteroids |
| 2 | M/71 | B-CLL | Herpes zoster | T10 | 1 mo | Granulomatous dermatitis | IV aciclovir | Topical corticosteroids |
| 3 | F/79 | B-CLL | Herpes simplex | Lip | 15 d | Granulomatous dermatitis | Oral valaciclovir | Topical corticosteroids |
| 4 | F/64 | Chronic rash | Herpes zoster | C4 | 2 mo | Granuloma annulare | Oral valaciclovir | Topical corticosteroids |
| 5 | F/53 | NHL | Herpes zoster | T8 | 2 mo | Lichenoid dermatitis | IV aciclovir | None |
| 6 | M/54 | B-CLL | Herpes zoster | L2 | 15 d | Lichenoid dermatitis | IV aciclovir | None |
| 7 | F/68 | No | Herpes zoster | 1st branch right trigeminal nerve | 7 mo | Systemic lymphoma | Oral valaciclovir | R-CHOP |
| 8 | M/71 | B-CLL | Herpes zoster | T2 | 3 mo | Leukemia cutis | IV aciclovir | Polychemotherapy |
| 9 | M/32 | B-CLL | Varicella | Crown | 1 mo | Leukemia cutis | IV aciclovir | R-CHOP |
Abbreviations: B-CLL indicates B-cell chronic lymphocytic leukemia; CHOP, cyclophosphamide, hydroxydaunorubicin, oncovin, and prednisone; F, female; IV, intravenous; M, male; NHL, non-Hodgkin lymphoma; and R-CHOP, CHOP plus rituximab.
The diagnosis of varicella, herpes zoster, or herpes simplex was clinical in most cases, although some cases were confirmed using the Tzanck test or direct immunofluorescence. A histologic study of the second dermatosis was performed in all cases.
Results (Table 1)A summary of the results is shown in Table 1. The patients were aged between 32 and 79 years and distribution by sex was similar: 4 men and 5 women. The initial dermatosis was a herpes infection in all cases: 7 herpes zoster, 1 varicella, and 1 herpes simplex. In our series, 6 out of the 9 cases (66%) had a prior hematologic malignancy.
The initial dermatosis was treated with systemic antiviral drugs in all cases, as most of the patients had associated immunosuppression.
The second dermatoses appeared after intervals of between 15 days and 7 months after the herpes or varicella had resolved. The second dermatoses were 4 cases of granulomatous dermatitis, 2 cases of lichenoid dermatitis, 2 cases of infiltration by B-cell chronic lymphocytic leukemia, and 1 case of infiltration by systemic non-Hodgkin lymphoma.
Below, we will discuss some of the 9 cases of isotopic response included in our series.
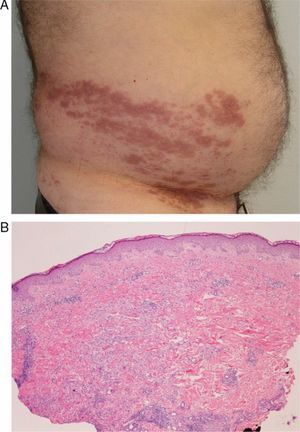
Case 2A 72-year-old man with a history of B-cell chronic lymphocytic leukemia who presented herpes zoster on the right flank, on the T10 dermatome (Fig. 1A). A month later he visited our department due to skin lesions at the same site. Histopathology revealed a lymphohistiocytic perivascular and interstitial infiltrate with the morphology of interstitial granulomatous dermatitis (Fig. 1B).
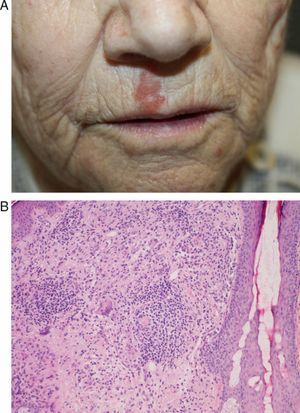
Case 3A 79-year-old woman with a history of chronic lymphocytic leukemia visited our department with a lesion on the right side of the upper lip. The lesion had appeared 15 days after the spontaneous resolution of a herpes simplex lesion on the same site. At the time of the visit, the patient presented a slightly infiltrated erythematous plaque measuring 2×1cm on the right side of the upper lip (Fig. 2A). A Tzanck test and direct immunofluorescence for herpes simplex virus type 1 and 2 were negative. Histopathology revealed a lymphohistiocytic infiltrate in the superficial dermis, with multinucleated giant cells forming loose, poorly-defined granulomas (Fig. 2B). The lesion gradually resolved following treatment with topical corticosteroids.
Case 3: A, Slightly infiltrated erythematous plaque with a corrugated surface, located on the right side of the upper lip. B, Granulomatous infiltrate in the superficial dermis, consisting of histiocytic growth and multinucleated-giant-cell forming loose, poorly-defined granulomas (hematoxylin-eosin, original magnification x10).
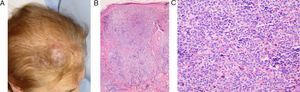
A 68-year-old woman with no relevant history had previously had herpes zoster in the area of the first branch of the right trigeminal nerve. Seven months later, she visited our department due to the appearance of new lesions in the same area. The patient presented a violaceous plaque in the same area in the right frontal region (Fig. 3A). Histopathology revealed a dense lymphoid infiltrate in the dermis; the infiltrate consisted of small and medium-sized lymphocytes that were positive for CD45 staining and were arranged in follicular groups. Immunohistochemistry was positive for CD20 and Bcl-6 and focally positive for CD10 and Bcl-2; these results were compatible with follicular lymphoma (Figure 3B and 3C).
Case 7: A, Erythematous-violaceous tumorous lesion in the right frontal area, in the region of the first branch of the trigeminal nerve. B, Lymphoid tumorous infiltration occupying the superficial and deep dermis and forming large groups with a follicular appearance (hematoxylin-eosin, original magnification x10). C, Small-to-medium-sized atypical lymphocytes arranged in follicular groups (hematoxylin-eosin, original magnification x20).
A bone-marrow biopsy revealed infiltration by the lymphoma. The patient was treated with CHOP and rituximab. In this case, the cutaneous infiltration was the first sign of the lymphoma and made it possible to diagnose the disease.
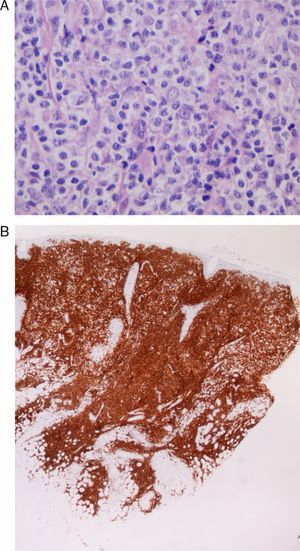
Case 9A 33-year-old man diagnosed with B-cell chronic lymphocytic leukemia, who had undergone multiple cycles of chemotherapy that included rituximab, fludarabine, and cyclophosphamide and had achieved complete remission 3 years after diagnosis. Two years later, he was admitted with varicella, which resolved after treatment with intravenous aciclovir. After 1 month, he visited our department with skin lesions in the form of erythematous-violaceous plaques on the site of the varicella scars on the face and scalp (Fig. 4). A skin biopsy revealed a lymphoid tumoral infiltration with diffuse growth, consisting of medium-to-large cells with prominent nuclei and nucleoli (Fig. 5A), and a high proliferation rate in the dermis. The infiltrate corresponded to the patient's lymphatic disease which was positive for CD5 (characteristic marker for B-cell chronic lymphocytic leukemia [Fig. 5 B]), CD79, and Bcl-2 and negative for CD30. A diagnosis of transforming B-cell chronic lymphocytic leukemia was made. The staging study confirmed involvement of the bone marrow and the consequent progression of the disease; treatment was therefore begun with CHOP and rituximab, with partial response, followed by different courses of treatment with alemtuzumab, lenalidomide, bendamustine, mitoxantrone, and rituximab. Because of the progression of the disease, the patient underwent an allogenic bone-marrow transplant from an unrelated donor.
Case 9: A, Medium-to-large-sized lymphoid cells with prominent nuclei and nucleoli, presenting mitotic activity (hematoxylin-eosin, original magnification x20). B, Diffuse CD5-positive tumorous infiltrate in the dermis, which corresponds to the skin infiltration by the patient's B-cell chronic lymphocytic leukemia (CD5 marker, original magnification x4).
In most cases of isotopic response, the initial dermatosis is herpes zoster,1 although it may be herpes simplex, varicella, or thrombophlebitis.3 In 2002, Cerroni et al.4 reported a case of infiltration by chronic lymphocytic leukemia on the scar of a benign cutaneous lymphadenosis due to Borrelia burgdorferi. As in the literature, in our series, all patients presented herpes zoster as the initial dermatosis, except for 2 patients, who presented herpes simplex and varicella.
The nature of the second dermatosis, however, may vary widely (Table 2). The most frequent second dermatoses are granulomatous reactions,5–8 particularly granuloma annulare,6 and lichenoid diseases. Cases of lichen planus on herpes zoster scars may require considering a differential diagnosis with zosteriform lichen planus,9–12 but the definitive diagnosis is based on the clinical history, which shows prior herpes zoster.
Second Dermatoses in Wolf's Isotopic Response.
| Inflammatory Disease | Tumoral Disease | Infectious Disease | Others |
| Granulomatous reactions (granuloma annulare) | Specific infiltrations (leukemias and lymphomas) | Viral infections (molluscum, common warts) | Acneiform eruptions |
| Lichenoid reactions (lichen planus) | Pseudolymphoma | Tinea | Keloid |
| Sclerotic and atrophic lichen | Basal cell carcinoma and squamous cell carcinoma | Furunculosis | Comedones |
| Morphea | Skin metastases of solid-organ tumors | Cutaneous Rosai-Dorfman disease | |
| Psoriasis | Kaposi sarcoma | Xanthoma | |
| Contact dermatitis | Angiosarcoma | Nodular solar degeneration | |
| Eosinophilic dermatosis | Reactive perforating collagenosis | ||
| Graft-versus-host disease | Unilateral nevoid telangiectasia | ||
| Centrifugal annular erythema |
Other second dermatoses described in the literature include comedones13 and acneiform eruptions, tinea, furunculosis, contact dermatitis, nodular solar degeneration, morphea, graft-versus-host disease,14 eosinophilic dermatosis, reactive perforating collagenosis, lymphomas and leukemias, Kaposi sarcoma,15 angiosarcoma,16 basal cell carcinomas and squamous cell carcinomas, and skin metastases. Viral infections such as molluscum contagiosum or common warts may also appear on the site of the previous herpes infection. Cases have also been described of centrifugal annular erythema,17 unilateral nevoid telagiectasia,18 and psoriasis plaques19 on the site of herpes zoster scars in patients with no personal or family history of the second disease.
In 1998, Requena et al.2 published a review of 20 cases; 14 of these developed a granulomatous dermatosis and 4 developed granuloma annulare. The other cases were pseudolymphoma, lichen sclerosus, lichen planus, keloid, and cutaneous Rosai-Dorfman disease.
In our series, 4 of the 9 patients (cases 1-4) developed a granulomatous dermatitis; this was the most frequent reaction, as reported in the literature. Lichenoid dermatitis was observed in 2 cases (cases 5 and 6).
Cases 8 and 9 were infiltrations by B-cell chronic lymphocytic leukemia, which the patients had presented previously. Of note is case 7, as the patient had an undiagnosed systemic B-cell lymphoma; the disease was diagnosed after the skin biopsy. In 1996, Cerroni et al.20 published 42 cases of infiltrations by B-cell chronic lymphocytic leukemia on herpes zoster and herpes simplex scars. In 2000, Paydaş et al21 described a case of T-cell lymphoma with skin infiltration in the scar of a previous herpes zoster infection.
In our study, 7 of the 9 patients presented an underlying malignancy, which was hematologic in most cases; this probably led to a state of immunosuppression, thereby predisposing the patient to develop herpes zoster. However, in the larger published series,1,2 this condition does not appear to be representative. In the review by Requena et al., 5 of the 20 patients had known immunosuppression. The immunosuppression associated with this type of malignancy would explain the higher incidence of herpes infections in these patients. We believe that the fact that our department is in a tertiary hospital, in close contact with the hematology department, led to the high incidence of hematologic malignancies in our series.
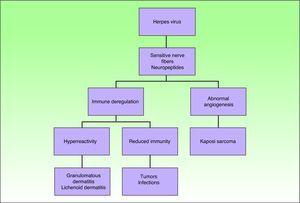
The pathogenesis of Wolf's Isotopic Response is unknown. It has been suggested that the nerve damage caused by herpes zoster, which can destroy nerve fibers in the dermis, may alter immunity; this would lead to hyperreactivity that would favor inflammatory processes such as granulomatous and/or lichenoid dermatitis, or local immunosuppression that would lead to tumor infiltrations, such as leukemia cutis, or infectious diseases.1 It has also been suggested that the nerve damage may cause abnormal angiogenesis, which would lead to vascular tumors (Fig. 6). Cell damage caused by the herpes virus does not tend to be observed in histology studies of the second disease. However, cases have been described in which viral DNA has been detected using PCR techniques,22,23 and in which glycoproteins24 of the herpes zoster viral envelope have been detected using in situ hybridization. No signs of active herpes infection were found in the biopsies of any of our cases.
Researchers have recently speculated on the role of tumor necrosis factor (TNF)-α in the pathogenesis of this disorder.19 TNF-α is implicated in the immune response to herpes zoster and in a wide variety of inflammatory skin diseases, and is involved in forming and maintaining granulomas.
We agree with the reviewed literature2,3 that administration of systemic antiviral treatment probably has no effect on the appearance of the isotopic response.
Finally, the inverse of this phenomenon has also been reported and is referred to by some authors as the inverse isotopic response.25 This is a rare condition in which the dermatosis does not involve the skin previously affected by another disease. The second dermatosis tends to be inflammatory and the previous lesion or dermatosis may be highly heterogeneous, ranging from benign neoplasm to viral infection (such as herpes zoster), and may appear on different sites, such as an irradiated area of skin or the site of a previous vaccination.26
ConclusionsWe present 9 cases of Wolf's isotopic response, in which the most frequent initial dermatoses are herpes zoster and the most frequent second diseases are granulomatous dermatitis and lichenoid dermatitis, as reported in the literature. Three cases of specific infiltration are of note: one of these was used to diagnose a systemic follicular lymphoma and another to diagnose the progression of the patient's B-cell chronic lymphocytic leukemia. We therefore recommend always performing a skin biopsy in this type of lesion.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Jaka-Moreno A, et al. Fenómeno isotópico de Wolf: serie de 9 casos. Actas Dermosifiliogr. 2012;103:798-805.