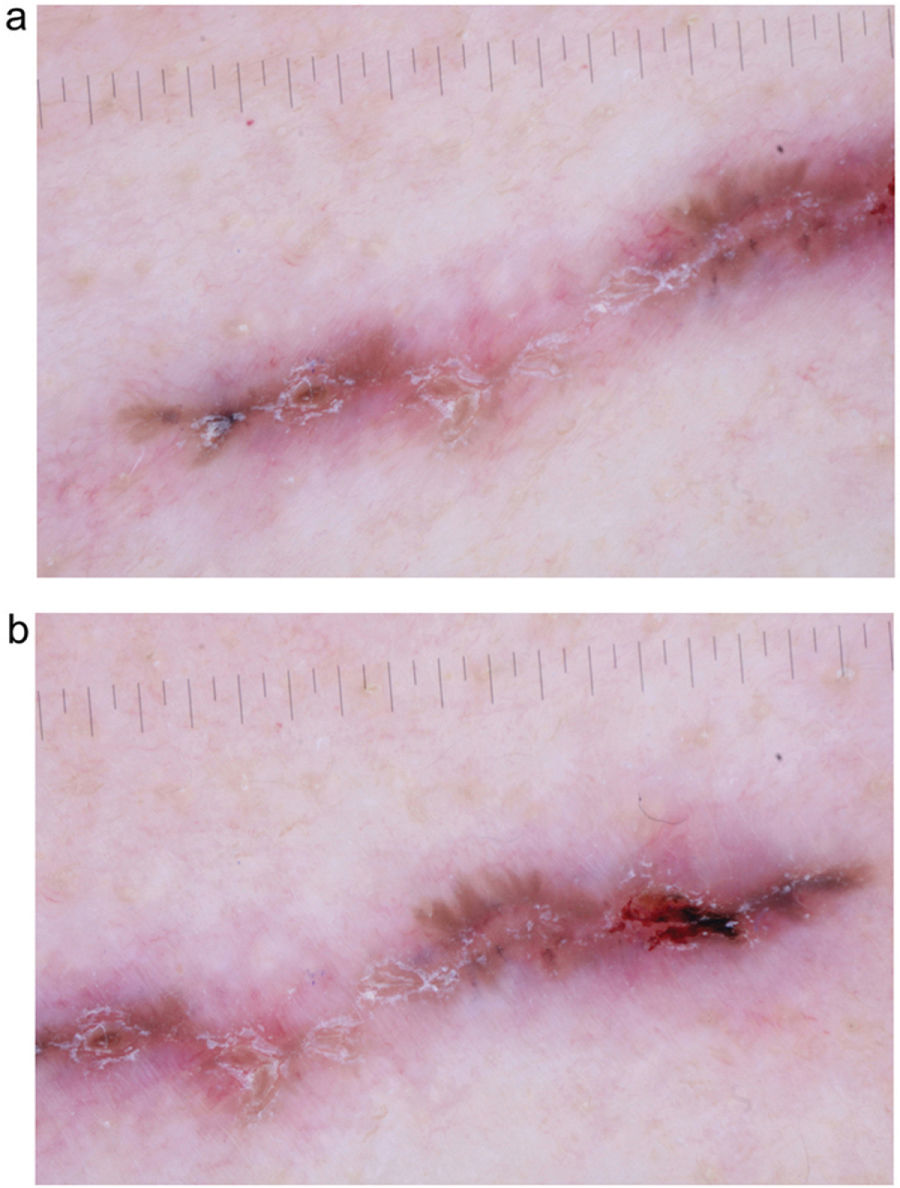
A 70-year-old woman, with no relevant past medical history, presented with a 1-year history asymptomatic lesion on her neck. Upon examination, she showed a 30mm x 2mm linear erythematous-brownish plaque, somewhat crusted, located in the depth of a fold on the left side of her neck (Fig. 1).
What is your diagnosis?
CommentDermoscopic findings shown in Fig. 2 are consistent with a non-superficial basal cell carcinoma. Complete excision of the lesion was performed, which confirmed the diagnosis of nodular and micronodular basal cell carcinoma with clear margins.
In our case, clinical differential diagnosis also included the following entities: scar, exogenous pigmentation, inverse pigmented lichen planus, and terra firma-forme dermatosis. Dermoscopy allowed us to establish an early diagnosis of basal cell carcinoma.
Linear basal cell carcinoma was first described in 19851 and is most commonly located in the periocular area and the neck2–6; the pathogenic mechanism by which the tumor tends to grow along skin tension lines is unknown to this date.2,3 No specific dermoscopic findings have ever been described for the linear variant of basal cell carcinoma.2,4,5 A recently published retrospective, descriptive study with 18 tumors of this type has analyzed their dermoscopic features4: more than 80% were pigmented, as in our case, a higher proportion than expected perhaps due to the ethnic characteristics of the study patients (mostly Hispanic/Latino) and a difficulty in diagnosing non-pigmented linear basal cell carcinoma that may lead to underdiagnosis.4,5 Dermoscopic structures specific to basal cell carcinoma most frequently observed were blue-gray globules, well-focused dots, and maple leaf-like structures4 (all present in our case).
We wish to mention the utility of dermoscopy to diagnose linear basal cell carcinoma, exclude other diseases that may also present a linear morphology,4 and more accurately delineate the tumor's extension, as reportedly, tumors have a greater-than-expected subclinical extension.3,6 Furthermore, dermoscopy can help guide the histological subtype before anatomopathological results become available and classify it as low or high risk, thus allowing for the selection of the most appropriate surgical technique and margins.2,6 The most common histological subtype of linear basal cell carcinoma is nodular,3–6 although it can sometimes be associated with more aggressive subtypes, such as the infiltrative or morpheaform subtypes.3,4 In retrospective studies and case series, Mohs surgery is the most widely used treatment for linear basal cell carcinoma,3,4,6 although other authors have also achieved good results with conventional surgery, as in our case, and recommend reserving Mohs surgery for aggressive histological subtypes, or those located in high or medium risk areas (H or M areas).6
Conflict of interestsThe authors state that they have no conflict of interests.