Lymphangioma circumscriptum (LC) is a malformation-derived pseudotumoral lesion consisting of several cysts on the skin and subcutaneous tissue, occasionally after an acquired insult or stasis affecting the lymphatic system. It is often found on the head, neck, trunk and axillae; vulval lymphangiomas, though, are a rare finding.1 Vulval LC can be asymptomatic or cause discomfort or pruritus.2 LC requires histopathological confirmation. Misdiagnosis as condylomatosis is not rare, particularly in verrucous forms. Recurrences are frequent among all treatment modalities.2 We present two cases of very painful vulval LC initially diagnosed as condylomas, which resolved completely after CO2 laser therapy.
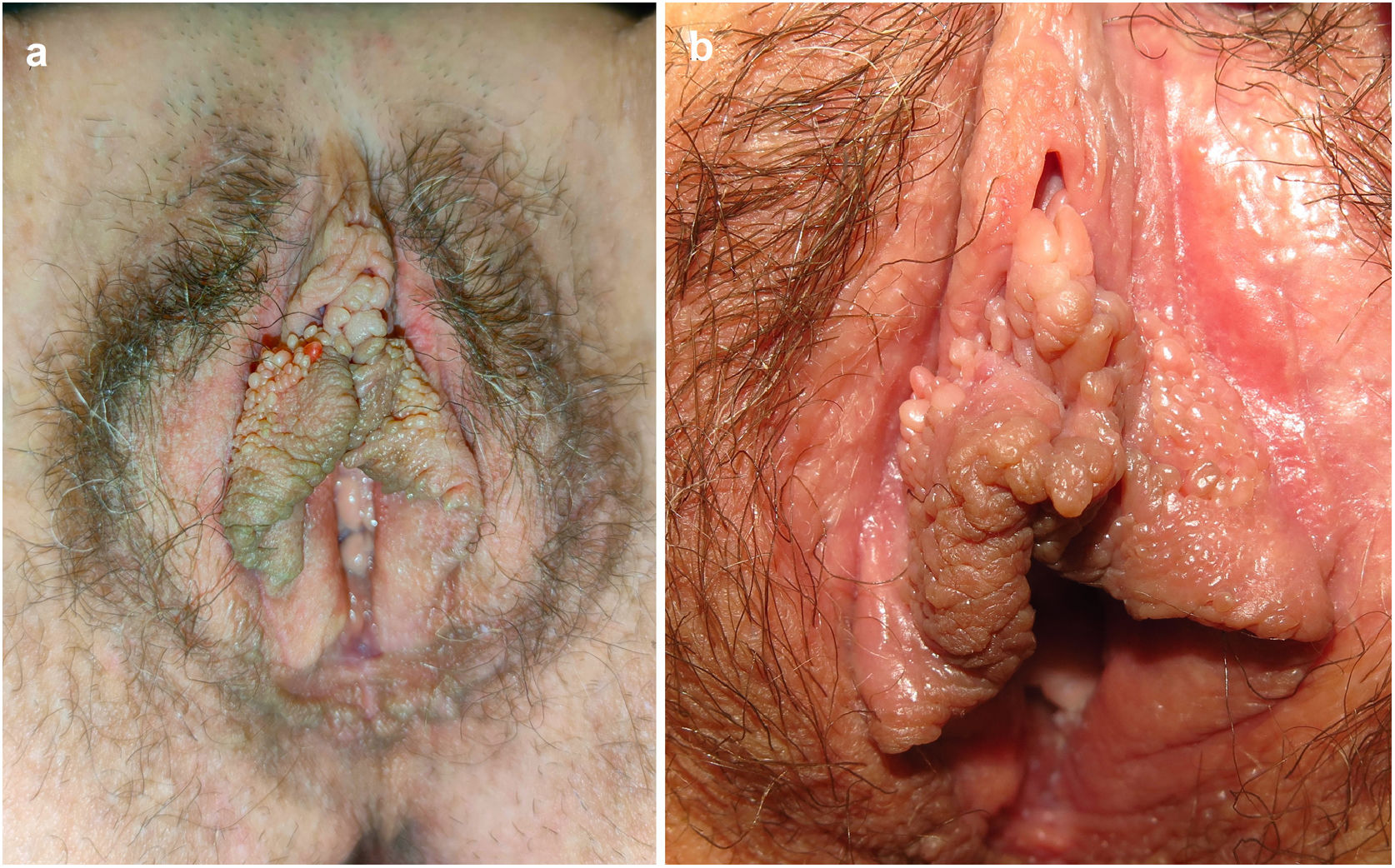
Case #1 was a woman in her 40s who presented with a 2-year history of periodically occurring vulval lesions. She reported the presence of pruritus and intense vulval pain. The physical examination revealed the presence of several translucent, coalescing papulovesicles on the two labia minora (Fig. 1). Condyloma acuminata was initially suspected, but acetowhite negativity signaled the need for a biopsy. The histopathological examination led to the diagnosis of LC (Fig. 2). Pelvic magnetic resonance imaging showed superficial bilateral tubulocystic structures on the vulva. No space occupying lesions on the draining lymphatics were identified. A single session of continuous-wave CO2 laser vaporization was performed, until all papulovesicles were gone. The patient will be followed-up at our center.
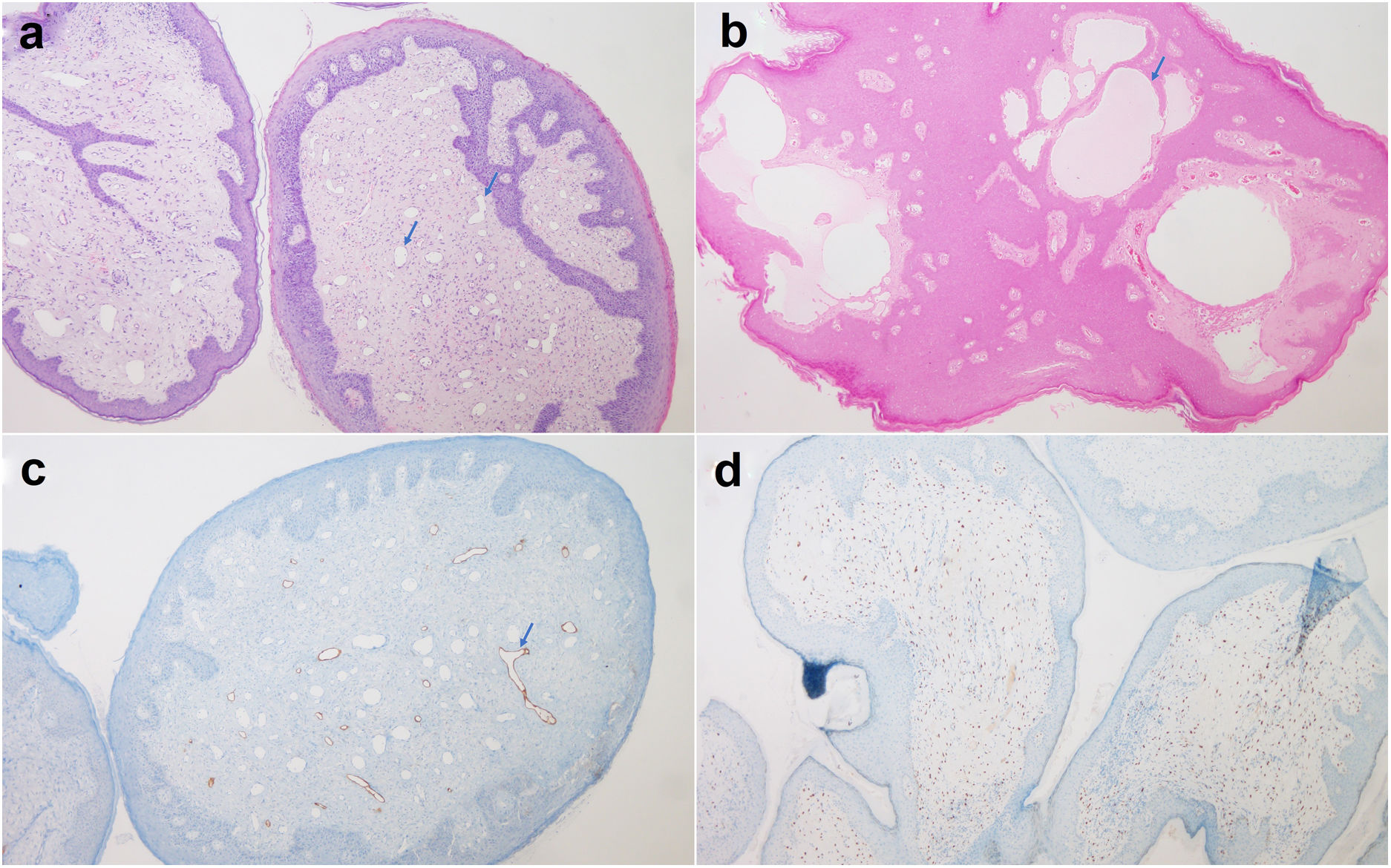
Microscopic findings of lymphangioma circumscriptum. (A and B) Histopathology examination revealing the presence of a polypoid lesion with dermal vascular proliferation and dilated vessels outlined by a single layer of endothelial cells (see arrows). (C) Patched positivity for D2-40. (D) Progesterone receptors expressed by stromal cells.
Case #2 was another woman in her 40s with a past medical history of chronic lymphedema on her lower limbs who came to our office due to spreading of the edema to the genitalia, and the onset of very painful vulval lesions. The gynecological examination revealed the presence of edematous vulval papulovesicles on both sides of labia majora and minora. Initially diagnosed as vulval condylomatosis, the patient received imiquimod, without a satisfactory response. The histopathological examination revealed the presence of enlarged lymphatic vessels in the papillary dermis, which led to a diagnosis of acquired lymphangioma circumscriptum. A diathermy loop was used to treat it that led to temporary remission. Five years later, the patient showed a recurrent vulval LC, which was successfully treated with a single session of continuous-wave CO2 laser vaporization and no further episodes have been reported to this date.
Congenital lymphangioma circumscriptum (LC) is a developmental defect of the skin lymphatic vessels, though most cases do not become apparent until adulthood. Non-inherited activating mutations in PIK3CA affecting the lymphatic endothelial cells have been identified3 causing lymphatic hyperplasia and leading to cyst formation due to fluid stasis. In contrast, acquired LC is triggered by lymphatic disruption4 following local processes such as pelvic surgery, radiation therapy, tuberculosis, fistulous Crohn's disease, or an obstructing neoplasm.5 Cases #1 and #2 describe a late-onset congenital and an acquired LC due to chronic lymphedema, respectively. Pathology and treatment options are the same for both these subtypes.
Vulval LC may occur at almost any age.2 It presents with diffuse or clustered millimeter-sized, thin-walled translucent or serous vesicles. Sometimes LC can have a verrucous appearance due to hyperkeratosis. Lesions may present with no symptoms or pruritus, a burning sensation, tenderness, discharge, or dyspareunia.5 Histopathology results show hyperplasia of the epidermis and dilatation of distorted, irregular lymphatic vessels in the papillary dermis, forming non-communicated cysts. Lymphatic channels can be identified by their flat endothelium expressing podoplanin (D2-40), PROX1, and VEGFR-3.
Neoplasm-related acquired vulval LCs are often due to pelvic and anogenital malignancies following radiation therapy or lymphadenectomy.6 The occurrence of lymphangiosarcoma in a case of long-standing LC has been reported.7 In the presence of a vulval LC without a previous history of lymphatic damage, an obstructive process in the draining lymphatics should be considered.8 We used magnetic resonance imaging over computerized tomography for a better study of the lymphatic system and soft tissues proximal to sites of a possible obstruction.
LC can simulate relapsing, smooth and hyperkeratotic condylomatosis. Herpes, impetigo, contact dermatitis, erythema multiforme, fixed drug eruption and some autoimmune bullous diseases and tumors can also mimic LC. Dermoscopy of LC shows the combination of lacunae and vascular structures in 71% of the cases. Other common features include the presence of white lines and the hypopyon sign.9
Indications for treatment of LC include cosmetic reasons, presence of symptoms, recurrent infections, or psychosexual dysfunction. Surgery,10 sclerotherapy, and several destructive treatments have often been used. Local recurrences are frequent, and non-surgical approaches have twice the recurrence rate of surgery,2 since the latter can remove the deep communicating lymphatic cisterns considered to be the main cause of recurrences. The second case shows how the persistence of the underlying cause in acquired LC probably also has a significant impact on recurrences. We used ablative CO2 laser therapy as a less invasive, well-tolerated, and safe alternative to surgery. CO2 laser induces vaporization of intracellular water, can penetrate up to the reticular dermis, seal lymph vessels, and induce sclerosis of vascular channels in LC.11 Laser settings are not standardized and vary widely between practitioners.
Vulval lymphangioma circumscriptum should be suspected in the presence of condylomatosis unresponsive to treatment. In vulval LC without a previous history of lymphatic damage, an obstructive process in the draining lymphatics should be ruled out. CO2 laser ablation is minimally invasive, effective, and safe against LC. However, more studies are needed to determine the most effective long-term treatment of vulval LC.
Conflict of interestThe authors declare that they have no conflict of interest.