Dermatomyositis (DM) presents with various cutaneous manifestations, some of which associate with internal malignancies. To date, single case reports of vesiculo-bullous DM have been reported in the English literature.1–6 We describe herein 5 cases of vesiculo-bullous DM in patients with internal malignancy.
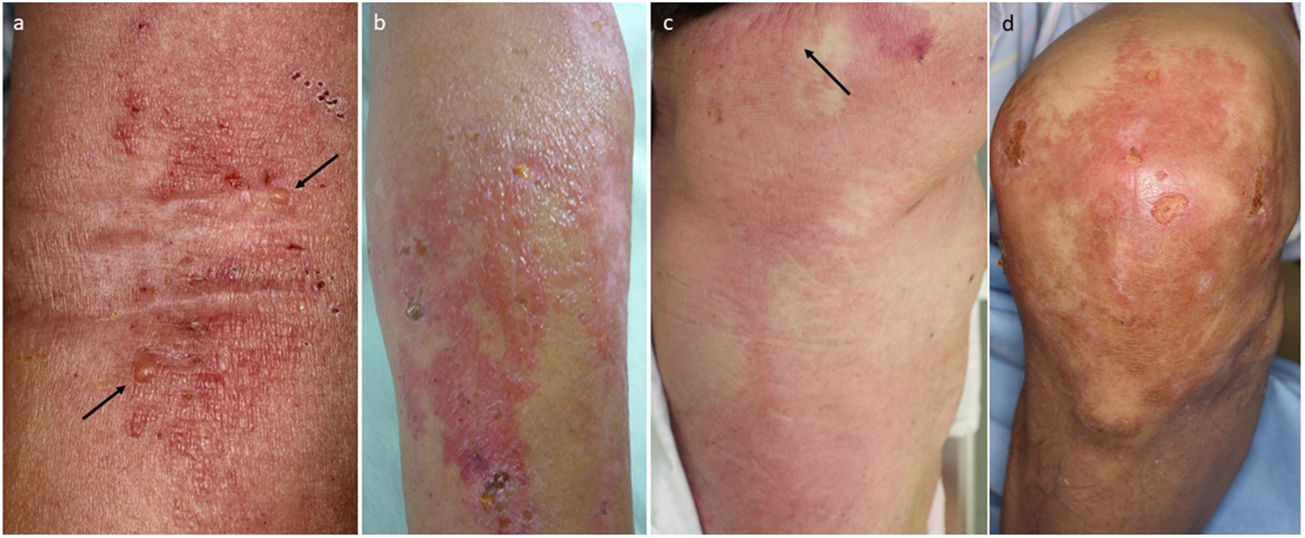
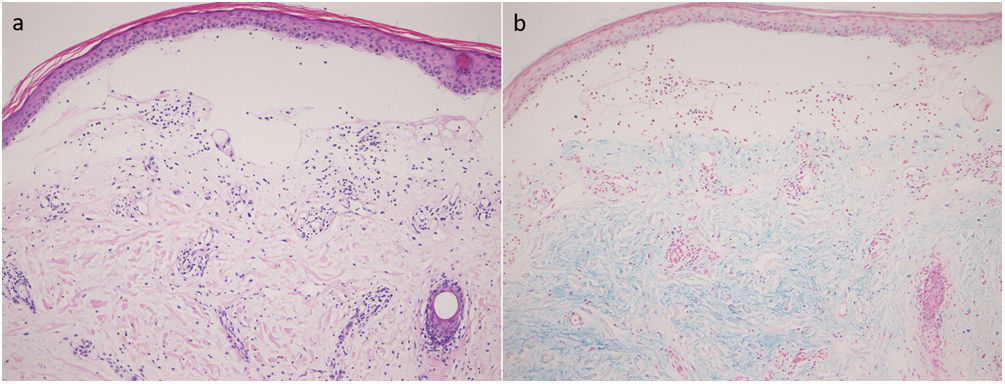
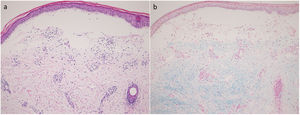
The present study included 5 patients with DM who developed vesicles and/or bullae during the course. The diagnosis of DM was based on the diagnostic criteria proposed by Bohan et al.7 The diagnosis of clinically amyopathic DM was made based on the classification criteria proposed by Sontheimer.8 The patients consisted of 4 males and 1 female, with an age range of 68 to 76 years (mean age: 71.6 years). The site of the bullous lesion was as follows: elbow (n=2), upper arm (1), knee (1), trunk (1) and shoulder (1) (Fig. 1). Biopsy was performed from the bullous lesion in 4 cases (Cases 1–4), which revealed marked subepidermal edema with mucin deposition in the upper dermis (Fig. 2). Direct immunofluorescence findings were negative at the basement membrane zone in all cases. Other cutaneous signs observed were Gottron's papules (n=4), poikiloderma (3), malignant erythema (2), seborrheic dermatitis-like facial erythema (1), and flagellate erythema (1). 3 cases (Cases 1, 3, and 5) were accompanied with myositis, and 1 case (Case 4) was diagnosed with clinically amyopathic DM. In only 1 case (Case 1), myositis-specific autoantibody was detected, which was anti-TIF-1γ antibody. Interstitial lung disease (ILD) was not observed in all cases. Malignancies were observed in all cases: lung cancer (n=3), esophageal cancer (1) and ovarian cancer (1). 3 cases (Cases 2, 4, and 5) were treated with chemotherapy. In Case 1, esophageal cancer was diagnosed after discharge from our hospital, and the patient's detailed medical condition was unclear. In Case 3, there were many metastatic lesions at the time of diagnosis of ovarian cancer, and the patient could not be treated with chemotherapy due to poor general condition. 3 cases (Cases 1, 3, and 4) were treated with oral prednisolone. The patient in Case 1 had progressive and severe dysphagia, and was treated with methylprednisolone (1000mg/day for consecutive 3 days), intravenous immunoglobulin therapy for 3 times, prednisolone and methotrexate. However, swallowing function was not fully recovered, and the patient repeatedly developed aspiration pneumonia. 3 patients (Cases 3–5) died of malignancy 6 months, 1 year and 2 years after the diagnosis of DM, respectively. Prognosis of the other 2 cases (Cases 1 and 2) was unknown. In all cases, the bullous lesions appeared in parallel with the onset of or increased disease activity of DM. DM was diagnosed at around the same time as the discovery of cancer, surgical operation of cancer or development of metastases (Table 1).
5 patients presenting with vesiculo-bullous dermatomyositis.
| Case | Age | Sex | Site of bullous lesion | Other skin lesion | Interstitial lung disease | Malignancy | Myositis | CK (U/L)45–163 | ANA | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 74 | M | Elbow | Gottron's papules, poikiloderma, seborrheic dermatitis, nail fold bleeding | − | Esophagus | + | 8028 | 320 (homogeneous) | mPSL, PSL, IVIG, MTX |
| 2 | 68 | M | Upper arm | Gottron's papules, poikiloderma | − | Lung | No data | 462 | 160 (homogeneous & speckled) | Chemotherapy |
| 3 | 76 | F | Trunk | Gottron's papules, malignant erythema | − | Ovarian | + | 264 | 80 (homogeneous) | PSL |
| 4 | 72 | M | Elbow, shoulder | Flagellate erythema, malignant erythema | − | Lung | − | 139 | <40 | PSL, chemotherapy |
| 5 | 68 | M | Knee | Gottron's papules, poikiloderma | − | Lung | + | 2966 | <160 | Chemotherapy |
mPSL, methylprednisolone; PSL, prednisolone; IVIG, intravenous immunoglobulin; MTX, methotrexate.
Vesicular formation in DM is relatively rare, but highly associated with internal malignancy. All of our patients had solid cancers, which were lung cancer (n=3), esophageal cancer (1) and ovarian cancer (1). Drug-induced bullous eruption was excluded. According to the report by Kubo et al., 19 cases of vesiculo-bullous DM were reviewed, of which 6 cases were males and 13 cases were females.1 Internal malignancy was observed in 10 cases: in the ovary (n=4), cervix uteri (n=2), stomach (n=1), uterine tube (n=1), mammary gland (n=1), and lung (n=1). After their report, we collected 17 cases of vesiculo-bulous DM, including those having mammary cancer (n=3), nasopharyngeal cancer (n=2), ovarian cancer (n=1), lung cancer (n=1), malignant lymphoma (n=1), colon cancer (n=1), gastric cancer (n=1), and thyroid cancer (n=1). However, there was no malignancy in 6 cases, while ILD was observed in 4 cases. The incidence of internal malignancy was much higher in patients with vesiculo-bullous DM than in those without bullous lesions.1
Myositis-specific autoantibodies were examined in a few of our cases, because examination of those autoantibodies became available only recently. Anti-TIF-1γ antibody was examined in 1 case (Case 1), which showed positive titers. The prevalence of cancer in anti-TIF-1γ-positive patients varies between 38% and 80%.9 A recent report suggests that abnormally changed tumor antigens can trigger autoimmune response by cross-reactive immunity, leading to muscle damage10; however, the mechanism of the induction of vesicular formation in association with tumor antigen is unknown.
In conclusion, in DM, a vesiculo-bullous lesion is a paraneoplastic cutaneous sign of internal malignancy, rather than ILD. Clinicians should be aware of the vesiculo-bullous DM.
Conflict of interestThe authors declare that they have no conflict of interest