Surgical reconstruction of the external nose, a common site for nonmelanoma skin cancer, is difficult. Oncologic surgery often leaves large skin defects, occasionally involving the underlying cartilage and nasal mucosa. We describe our experience with the paramedian forehead flap for reconstruction of nasal defects.
MethodologyWe performed a retrospective study of consecutive patients in whom a paramedian forehead flap was used to repair surgical defects of the nose between July 2004 and March 2011. We describe the clinical and epidemiologic characteristics, the surgical technique, complications, secondary procedures, and cosmetic results.
ResultsThe series comprised 41 patients with a mean (SD) age of 67 (10.36) years. The majority were men (male to female ratio, 2.4:1). Associated risk factors included diabetes in 27% of patients, cardiovascular risk factors in 49%, and smoking or drinking in 19.5%. The tissue defects were distal in 80% of cases and nonpenetrating in 78%. The mean (SD) diameter was 21.6 (6.78) mm. Early postoperative complications occurred in 14.6% of patients and late complications in 31.7% (trap door effect in 22% and hair transposition in 19%), with a need for Readjustment in a second operation was needed in 19.5% of patients. The cosmetic results were considered acceptable or excellent in 90.2% of cases.
DiscussionThe paramedian forehead flap is versatile and provides skin of a similar color and texture to that of the external nose. It has a reliable vascular pedicle that guarantees the viability not only of the flap but also of other tissues that may be used in combination, such as chondromucosal or chondrocutaneous grafts. Revision of the technique in a second operation may sometimes be required to achieve an optimal result.
La pirámide nasal, área de difícil reconstrucción quirúrgica, constituye una localización predilecta del cáncer cutáneo no melanoma. La cirugía oncológica a menudo origina defectos cutáneos extensos, con la participación ocasional del cartílago subyacente y de la mucosa nasal. Nuestro objetivo es describir nuestra experiencia en el uso del colgajo paramediofrontal en la reconstrucción de defectos nasales.
MetodologíaEstudio retrospectivo de pacientes consecutivos en los que se empleó un colgajo paramediofrontal para la reconstrucción de defectos quirúrgicos nasales (julio de 2004-marzo de 2011). Se describen aspectos clinicoepidemiológicos, características de la técnica quirúrgica, complicaciones, procedimientos secundarios y resultados cosméticos.
ResultadosSe incluyen 41 pacientes, con edad media de 67 años (SD: 10,36) y de predominio masculino (2,4:1). Los factores de riesgo asociados fueron diabetes (27%), factores de riesgo cardiovascular (49%) y hábitos tóxicos (19,5%). Los defectos de sustancia eran mayoritariamente distales (80%) y no penetrantes (78%), con un tamaño medio de 21,6mm (SD: 6,78). Un 14,6% de los pacientes presentaron complicaciones posquirúrgicas precoces y un 31,7% secuelas tardías (22% abultamiento del colgajo y 19% transposición de pelo), requiriéndose técnicas de refinamiento secundario en el 19,5% de los pacientes. Los resultados cosméticos se consideraron mayoritariamente aceptables/excelentes (90,2%).
DiscusiónEl colgajo paramediofrontal es un colgajo versátil, que proporciona características similares en color y textura a la piel de la pirámide nasal. Su pedículo vascular seguro garantiza su viabilidad, así como la de otros tejidos, cuando se utiliza en combinación con injertos condromucosos o condrocutáneos. Para la obtención de resultados óptimos pueden requerirse procedimientos de revisión secundarios.
The external nose is one of the most common sites for skin cancer and one of the most complex anatomic regions for reconstruction.1 Complete excision of a skin cancer lesion on the nose often leaves a large skin defect, which may also involve the underlying cartilage and nasal mucosa.2 In such cases, particularly with defects that affect the distal region of the external nose or that are extensive (diameter greater than 1.5cm),3 the paramedian forehead flap represents an excellent option as it provides a large volume of cutaneous tissue with good viability.
The paramedian forehead flap is a standard procedure in reconstructive nasal surgery. It is based on axial vascularization and a temporary pedicle. Despite the inconvenience of a 2-stage procedure, many authors agree that this is a safe flap and that the cosmetic and functional results are good.3,4 The objective of the present study has been to describe our experience in the use of the paramedian forehead flap for the reconstruction of nasal defects.
Material and MethodsThis was a retrospective descriptive study of a consecutive series of patients who underwent surgery in the dermatology department of Hospital Costal del Sol in Malaga, Spain, between July 2004 and March 2011 and in whom the paramedian forehead flap was used to reconstruct a nasal skin defect. The following variables were analyzed: the main epidemiologic features and clinical findings (sex, age, diagnosis, and comorbidities), characteristics of the tissue defect (site, size, number of anatomic subunits affected, thickness), surgical technique, early complications (bleeding, necrosis, infection, wound dehiscence), late sequelae (excessive flap thickness, presence of hair, nasal asymmetry due to retraction), and secondary revisional procedures. The comorbid conditions considered were the presence of diabetes mellitus, cardiovascular risk factors, and drinking and smoking. Cardiovascular risk factors included systemic hypertension, coronary artery disease, and a history of vascular surgery.
The cosmetic results of this type of flap were analyzed using pre- and postoperative photographs, which were evaluated by 3 independent dermatologist observers using a 3-point scale (1, unacceptable; 2, acceptable; and 3, excellent). An unacceptable result was defined as retraction or a loss of continuity, and acceptable and excellent results as partial or complete maintenance of the contour and volumes of the cosmetic units. In each case, the cosmetic result used was the score (1, 2, or 3) that achieved greatest concordance among the 3 observers.
Surgical ProcedureThe paramedian forehead flap is a skin flap with a temporary pedicle. It is a 2-stage procedure, with the operations separated by an interval of 2 to 3 weeks.
The first stage is usually performed under locoregional anesthesia (mepivacaine, 1% or 2%) with sedation, except in cases requiring reconstruction of full-thickness nasal defects, when general anesthesia is used. The flap is designed on the right or left side of the forehead, depending of the state of the forehead skin (old scars). An axial pedicle with a width of 10 to 15mm is drawn, starting close to the eyebrow and ascending 2cm lateral to the midline of the forehead. The flap is lifted, starting distally in the subcutaneous plane and advancing in the subgaleal plane for the remainder of the dissection, except in the region of the pedicle, where dissection is in the subperiosteal plane. After dissection, the flap is rotated axially through 180° and its distal part is applied to the nasal defect (Figure 1). The forehead wound can usually be closed by direct suture; when there is excessive tension, we perform frontotemporal advancement, and sometimes insert a full-thickness skin graft or allow healing to occur by second intention. A fast-absorbing suture is usually used to close deeper planes, and a 4/0 and 5/0 nylon monofilament suture for the skin.
Design of the paramedian forehead flap. Design of the axial pedicle, which is initiated in the proximal region of the eyebrow and ascends parallel but 2cm lateral to the midline of the forehead. Flap elevation and rotation through 180° on its axis, with subsequent suture to the nasal defect.
Any loss of cartilage or of the internal lining of the nose must be repaired before the skin is repaired. We usually use cartilage from the concha of the ear for cartilage reconstruction. Repair of the mucosa is achieved using folded skin flaps, septal chondromucosal flaps, or auricular chondrocutaneous grafts.
At the end of the operation, the pedicle is carefully wrapped in petrolatum gauze and is covered with mupirocin ointment. When a full-thickness reconstruction is performed, we pack the nasal fossa, which not only aids hemostasis but also provides internal support to the tissues during the healing process.
Patients remain in hospital for 24 to 48hours for pain control and to perform surgical wound care. Dressings are reviewed every 12hours during the initial days, with special attention being paid to the pedicle. Oral antibiotic prophylaxis is administered with cloxacillin, 500mg by mouth every 6hours for 1week.
The pedicle is divided after 3 weeks and the residual skin defect is closed. Subcutaneous thinning is usually performed at this time to better adapt the donor skin to the recipient site (Figure 2). The second operation is performed in ambulatory surgery under local anesthesia, and no specific preparation is required.
All the data gathered in this project were recorded anonymously, in strict compliance with current laws and guidelines on data protection (Organic Law 15/1999 of 13th December on the protection of personal data, and Law 41/2002 of 14th November on patient autonomy). A descriptive analysis was performed using measures of central tendency (mean and standard deviation) for quantitative variables and frequency distribution for qualitative variables. The χ2 test was used to compare subgroups (the Fisher test was used when expected observations were less than 5). A P value less than .05 was considered statistically significant.
ResultsIn the period from July 2004 to March 2011, 41 patients underwent operations involving a paramedian forehead flap. The mean (SD) follow-up was 70.9 (23.3) months. The clinical and epidemiologic details of the series, the characteristics of the tissue defect, and the surgical technique are presented in the additional material and in Table 1.
Epidemiological and Clinical Characteristics and Technical Surgical Aspects.
| Age, y | 66.7 (10.36) |
| Sex | |
| Ratio of men to women | 2.4 to 1 (29/12) |
| Etiology | |
| Skin cancer, 97.6% | |
| Basal cell carcinoma, 85.4% (n=35) | |
| Squamous cell carcinoma, 9.8% (n=4) | |
| Lentigo maligna melanoma, 2.4% (n=1) | |
| Trigeminal trophic ulcer, 2.4% (n=1) | |
| Characteristics of the defect | |
| Size, mm | 21.6 (6.7) |
| Site: | |
| Proximal (dorsum, lateral wall of the nose), 20% (n=8) | |
| Distal (tip, ala), 80% (n=33) | |
| No. of anatomic subunits: | |
| 1: 41.5% (n=17) | |
| 2: 43.9% (n=18) | |
| 3 or more: 14.6% (n=6) | |
| Depth of the defect: | |
| Superficial (cutaneous), 88% (n=32) | |
| Deep (cartilage or mucosa), 22% (n=9) | |
| Type of reconstruction | |
| Cutaneous reconstruction | |
| Paramedian forehead flap, 100% (n=39) | |
| Cartilage reconstruction, 22% (n=9) | |
| Cartilage graft, 88.8% (n=8) | |
| Septal, 22.2% (n=2) | |
| From the concha of the ear, 66.6% (n=6) | |
| Titanium mesh, 11.2% (n=1) | |
| Reconstruction of the mucosa, 22% (n=9) | |
| Septal flap, 11% (n=1) | |
| Septal chondromucosal flap, 22.2% (n=2) | |
| Auricular chondrocutaneous graft, 11% (n=1) | |
| Folded nasolabial flap, 55.6% (n=5) | |
The operations were performed on 12 women and 29 men aged between 41 and 85 years (mean [SD], 66.7 [10.3] years). All but 1 of patients presented nasal tissue defects secondary to the surgical excision of a nasal skin cancer (35 basal cell carcinomas, 4 squamous cell carcinomas, 1 lentigo maligna) (Figure 1) (Table 1).
The following risk factors were identified: diabetes mellitus (27%), cardiovascular risk factors (49%), and drinking and smoking (19.5% [smoking, 14.5%; drinking, 5%]).
Characteristics of the DefectThe diameter of the defect varied between 15 and 40mm (mean, 21.6 [6.7] mm). More than 1 cosmetic subunit was affected in over half of patients (58.5%). In 33 (80%) cases the defects were distal (21 at the tip and 10 on the nasal ala). In 9 (22%) cases the defects were deep, affecting the underlying cartilage and nasal mucosa in addition to the skin (Figure 1).
Reconstruction TechniqueThe paramedian forehead flap made it possible to close the skin defect in all cases. In the 9 cases with deep tissue defects affecting the cartilage and mucosa, the paramedian forehead flap was combined with additional reconstructive techniques.
In the majority of cases requiring reconstruction the lining of the nose we used a folded nasolabial flap. Chondromucosal grafts from the nasal septum, chondrocutaneous auricular grafts, or septal mucosal flaps were used in the other cases.
Cartilage repair was required in 7 (17%) patients; in 6 cases we used a cartilage graft from the concha of the ear and in 1 the cartilage was substituted by a synthetic titanium mesh.
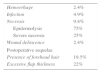
Complications (Tables 2 and 3)Postoperative complications (1 or more) occurred in 6 (14.6%) patients. The incidence of flap hemorrhage and of wound dehiscence was 2.5% (n=1 in each case), skin infection occurred in 5% (n=2), and necrosis of the plasty in 18% (n=5). No statistically significant association was observed between the appearance of early complications and factors such as diabetes, cardiovascular risk factors (P=.32), smoking (P=.11), or distal site of the flaps (P=.56) (Tables 2 and 3).
Early Postoperative Complications and Late Sequelae.
| Risk Factors | Early Complications | Postoperative Sequelae | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| DM | CVRF | Drinking and smoking | Anticoag | Hemorrhage | Infection | Epidermolysis | Dehiscence | Flap Thickness | Hair Transposition | |
| Case 2 | -- | -- | Smoker | -- | -- | -- | -- | -- | -- | + |
| Case 5 | + | + | -- | -- | + | + | -- | -- | + | -- |
| Case 6 | -- | -- | Smoker | -- | -- | -- | + | -- | -- | -- |
| Case 7 | -- | + | -- | + | -- | -- | -- | -- | + | -- |
| Case 8 | -- | -- | Smoker | -- | -- | -- | + | + | -- | -- |
| Case 9 | -- | + | -- | -- | -- | -- | -- | -- | + | -- |
| Case 10 | -- | -- | -- | -- | -- | + | -- | -- | + | + |
| Case 11 | + | + | -- | + | -- | -- | -- | -- | + | -- |
| Case 12 | -- | + | -- | + | -- | -- | -- | -- | + | + |
| Case 13 | -- | -- | Not recorded | -- | -- | -- | -- | -- | + | + |
| Case 15 | + | + | -- | + | -- | -- | -- | -- | + | -- |
| Case 16 | -- | + | -- | + | -- | -- | -- | -- | -- | + |
| Case 19 | -- | -- | -- | -- | -- | -- | + | -- | + | + |
| Case 26 | -- | -- | -- | -- | -- | -- | -- | -- | -- | + |
| Case 30 | + | + | -- | + | -- | -- | + | -- | -- | -- |
| Case 33 | -- | -- | -- | -- | -- | -- | -- | -- | -- | + |
| Case 36 | -- | + | -- | + | -- | -- | -- | -- | + | -- |
Abbreviations: Anticoag, anticoagulant or antiplatelet treatment; CVRF, cardiovascular risk factors; DM, diabetes mellitus.
Postsurgical sequelae, including excessive thickness of the initial flap and the presence of hair, occurred in 31.7% of patients. Excessive thickness of the flap developed in 36.5% of cases (n=15), and this persisted beyond the first 6 months after surgery in 22% of cases (n=9); surgical correction was performed in 7 (77%) of these cases. The transposition of forehead hair with the flap was observed in 19% of cases (n=8), though only 25% of these patients requested electroepilation treatment. No patients developed nasal asymmetry as a postsurgical sequela due to scar retraction of the ala. Dermabrasion of the flap was performed in 7.3% of patients (n=3) in order to achieve a homogeneous scar and improve the cosmetic result.
Cosmetic ResultsThe cosmetic results were considerable unacceptable in 9.8% of cases, acceptable in 46.3%, and excellent in 43.9%. No statistically significant relationship was detected between the cosmetic results and the presence of early postoperative complications or late sequelae (P=.09 and P=.57, respectively).
DiscussionThe origins of the forehead flap date back to Hindu surgery in the year 600 bce. Many modifications to the classic forehead flap technique have been proposed since its first descriptions in the European literature,5,6 and many studies have demonstrated the usefulness of the paramedian forehead flap for the reconstruction of complex nasal defects. Many authors now consider this flap an excellent option for reconstruction of the cutaneous plane in deep nasal defects and those larger than 1.5cm.3,4 We have presented a series of 41 patients with loss of nasal tissue substance and repair of the skin defect using a paramedian forehead flap. In our experience this flap has shown numerous advantages, mainly for its very varied indications, its good cosmetic results, and its low rate of complications.
In our series, the paramedian forehead flap was found to be highly versatile in its design and, as a result, covered a wide range of possible indications. The flap can be adapted to proximal and distal nasal defects by simply varying the length of the pedicle. Likewise, its size can be modified to provide sufficient tissue to replace the skin of the whole of the external nose.4,7
Another property of the paramedian forehead flap is its excellent vascularization. This is a flap with a thick axial pedicle that guarantees the viability of the donor skin and can even enhance nutrient delivery to other tissues (chondromucosal and mucocutaneous grafts) that may be used in combination with a paramedian forehead flap for the reconstruction of deep nasal defects.8–11 Furthermore, its rich blood supply helps to achieve a low rate of complications, even in patients with comorbid conditions.4,12
Necrosis is the most common complication reported (16%),13 and this was also the situation in our series (10%) (Figure 3). Equally, because this is a flap with an open pedicle, bleeding is common during the first 24hours, but tends to cease spontaneously. Excessive bleeding or its persistence beyond the early postoperative period is very rare (2.5% in our series). The incidence of other postoperative complications, such as infection or wound dehiscence, is very low.13
The robust blood supply of the pedicle means that, if necrosis develops, it is usually only superficial or partial.13 A number of studies have reported a relationship with certain risk factors, particularly with smoking,13,14 cardiovascular diseases, and diabetes, and with technical aspects that reduce the viability of the flap (a long pedicle, transverse scars on the forehead) or that increase the vascular demands of the flap (large area of donor skin, trauma to the flap by hair follicle electrolysis). In patients with risk factors, quitting smoking14 and the use of deferred transposition techniques15 (incision of the perimeter of the flap in an initial operation and flap elevation 3 weeks later) are the main measures used to prevent vascular suffering of the flap. In our series only 1 patient presented extensive necrosis of the whole flap; that patient was a heavy smoker. In other patients who presented necrosis, it was superficial and affected only limited areas; those cases may have been related to the use of distal flaps in patients with diseases that increase vascular risk. All our cases with necrosis resolved with conservative debridement, and the final cosmetic and functional results were not affected.
A final advantage that should be noted for this type of flap is the good cosmetic and functional result that can be achieved in the majority of cases. This is due in part to the use of skin from the forehead to create the flap; the texture, color, and flexibility of this skin are very similar to the skin of the external nose.
The paramedian forehead flap does have some possible disadvantages that the surgeon must be aware of. The main disadvantage is that it is a 2-stage procedure, usually with an interval of 3 weeks between the operations. Although the second stage (in which the vascular pedicle is divided) is a simple, low risk procedure that can be performed under local anesthesia, the fact that the overall surgical procedure is prolonged can considerably reduce the patient's quality of life. A reduction in the interval between operations16 and tunneling the vascular pedicle beneath the healthy skin17,18 of the dorsum of the nose have been described by various authors as options to reduce this disadvantage without affecting the cosmetic result. However, tunneling the vascular pedicle is a complex surgical technique, particularly in distal defects, when it can often provoke skin thickening over the whole of the dorsum of the nose.
Further disadvantages include the scar created on the forehead and the large amount of healthy forehead skin that is lost when the pedicle is divided. However, despite this considerable loss of forehead tissue, the defect can often be closed directly or by the advancement of adjacent tissues, with no major cosmetic repercussions.2
Finally, the paramedian forehead flap can give rise to specific sequelae due to its particular anatomic features; important sequelae are the transposition of forehead hair (Figure 4) and excessive flap thickness (Figure 5). The transposition of hairy skin from the scalp to the area of the nose occurs in patients with a low hairline; this can be resolved later by electrolysis or laser treatment of the hair follicles. Excessive flap thickness is the most common sequela. The main preventive measure is surgical thinning of the flap. Although this can be performed early (during dissection of the flap or when the pedicle is divided), postponement is recommended in patients with vascular risk factors in order to avoid compromising the viability of the donor tissue. Corticosteroid infiltration in the thickened area can also accelerate the thinning process.19 However, excessive thickness resolves spontaneously over the first year in a large percentage of cases, and many authors therefore recommend a conservative approach.
Our experience has revealed some clues to the optimization of flap results. An appropriate design and a meticulous technique are essential to ensure the blood supply and viability of the flap. The design is based on the supratrochlear artery, which ascends vertically in the paramedian region (2cm from the midline) over the frontalis muscle. Distally, its terminal branches are connected to the vessels of the subdermal plexus of the scalp. However, the most proximal segment of the supratrochlear artery descends between the orbicularis oculi and corrugator muscles to reach the periosteal plane. Here the artery anastomoses with branches of the angular and supraorbital arteries. Meticulous dissection of the flap will preserve the 3 vessels, maximizing blood flow to the pedicle.4 Designing the flap to respect the anatomic subunits of the nose20,21 allows the incisions to be concealed in the borders between these subunits, thus improving the cosmetic results. Finally, procedures for secondary review, such as dermabrasion of the skin surface, can improve the cosmetic result and achieve a more homogeneous appearance21,22 in those cases in which this is required.
The limitations of our study stem from its retrospective design and the small size of the sample. Further studies are necessary to analyze the factors associated with possible complications, such as measures of the subjective evaluation by the patient (perception of changes in quality of life and tolerance of or satisfaction with the results).
In conclusion, the paramedian forehead flap is a useful, safe, and versatile technique. Its main indication is for the repair of nasal tissue defects with a diameter greater than 1.5cm, which exceed the possibilities of local flaps, particularly when the defects affect the full thickness of the wall (skin, cartilage, and mucosa). Optimization of results depends on the use of a careful technique and preservation of the cosmetic subunits (Figure 6). Further studies are necessary to know patients’ opinions and the repercussions on their quality of life.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this research.
Confidentiality of dataThe authors declare that they followed their hospital's regulations regarding the publication of patient information.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Blázquez-Sánchez N, Fernández-Canedo I, Repiso-Jiménez JB, Rivas-Ruiz F, De Troya-Martín M. Utilidad del colgajo paramediofrontral en cirugía reconstructiva nasal: estudio retrospectivo de una serie de 41 pacientes 2016;107:133–141.