Syphilis is a sexually transmitted infection caused by Treponema pallidum, subspecies pallidum. As these bacteria are difficult to culture, syphilis must be diagnosed by serologic testing. The introduction of automated treponemal tests has led to changes in the traditional diagnostic algorithm for syphilis, which began with a nontreponemal test. We present 15 cases of primary syphilis detected using these new tools and review the microbiologic techniques used for the diagnosis of early syphilis.
Material and methodsWe examined all cases of syphilis diagnosed in our department between January 2013 and September 2018 and selected patients with negative nontreponemal (rapid plasma reagin [RPR]) tests.
ResultsOf the 158 patients diagnosed with syphilis during the study period, 15 had a negative RPR test, and 14 of them had a positive treponemal test. Fourteen of the patients were men and ages ranged from 22 to 60 years. Polymerase chain reaction was used to detect T pallidum in the lesion exudate from 8 patients and was positive in all cases. The 15 patients were treated with a single injection of 2.4 million units of benzathine penicillin G.
ConclusionChemiluminescence immunoassays and T pallidum automated enzyme-linked immunoassays are useful in the diagnosis of early syphilis, and we believe that they should be adopted as screening tools given their diagnostic sensitivity, speed, and low cost.
La sífilis es una infección de transmisión sexual (ITS) producida por el treponema pallidum subespecie pallidum, bacteria difícil de cultivar por lo que se requieren técnicas serológicas para su diagnóstico. La aparición de nuevas pruebas treponémicas (PT) automatizadas ha supuesto un cambio en el algoritmo diagnóstico de la sífilis, el cual tradicionalmente se iniciaba con una prueba no treponémica (PNT). Presentamos 15 casos de sífilis primarias detectadas gracias a la utilización de las nuevas PT automatizadas y realizamos una revisión de las técnicas microbiológicas en el diagnóstico de sífilis precoz.
Material y métodosSe recogieron todos los casos de sífilis diagnosticados en nuestro servicio desde enero de 2013 hasta septiembre de 2018. Se seleccionaron los pacientes con PNT negativas, RPR en particular.
ResultadosDe un total de 158 pacientes diagnosticados de sífilis en este periodo, 15 presentaron PNT (RPR) negativas y de estos 15, todos excepto uno presentaron PT positivas. Catorce casos eran varones, con un rango de edad desde 22 a 60 años. Además a 8 pacientes se les realizó reacción en cadena de la polimerasa (PCR) del exudado de la úlcera, siendo en todos ellos positiva. Los 15 pacientes fueron tratados con 1 dosis única de penicilina G benzatina 2.4 millones UI.
ConclusiónResaltamos la utilidad de las nuevas técnicas serológicas automatizadas, Chemiluminiscence Inmunoassay (CLIA) y Automated Treponema Pallidum Enzime linked Inmunoassay (EIA) y apoyamos su implantación como pruebas de screening en el diagnóstico de sífilis, dado su sensibilidad diagnóstica, su rapidez y su bajo coste.
Syphilis is a sexually transmitted infection (STI) that is still very much present today. Twelve million people are diagnosed each year and the disease is a major public health problem throughout the world. The Treponema pallidum subspecies pallidum, the causative agent of syphilis, is a difficult microorganism to culture, and so diagnosis is based on sensitive serological techniques to confirm infection.1
For decades, most hospitals have used the traditional diagnostic algorithm based on an initial non-treponemal test (NTT)—usually the rapid plasma reagin (RPR) test—in serum as screening, and only in the event of positive findings are confirmatory treponemal tests (TTs) performed.
The availability of automated TT tests has driven a change in the diagnostic algorithm for syphilis, with such tests now used for screening. Based on this new reverse algorithm, we present 15 case reports of primary syphilis with negative classic screening NTT and we review the literature.2
Case HistoriesIn this study, we examined all cases of syphilis diagnosed in the dermatology department of the Hospital General Universitario in Valencia, Spain, between January 2013 and September 2018. A total of 158 patients were diagnosed with syphilis in this period. Fifteen of these had negative NTTs (RPR), with initial suspicion of syphilis confirmed thanks to positive results in the TTs. In all cases, serial dilutions had been performed to avoid a prozone phenomenon and thus rule out the possibility of false negatives for this reason.
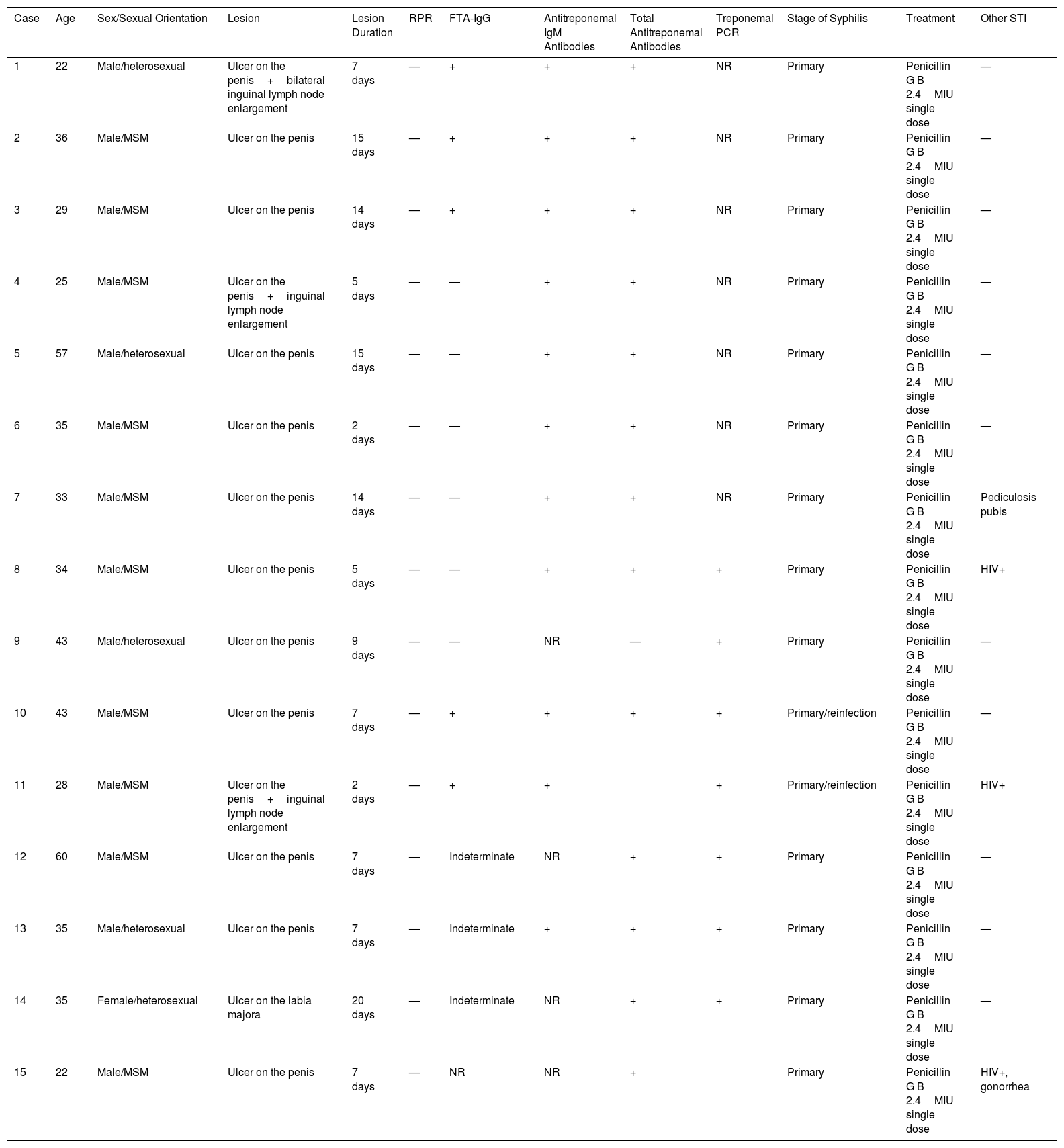
The most relevant clinical and microbiological characteristics of the patients, as well as the complementary tests performed are summarized in Table 1.
Clinical and Serological Characteristics of Our 15 Patients Diagnosed With Syphilis by Automated TT, All With Negative NTT (RPR).
| Case | Age | Sex/Sexual Orientation | Lesion | Lesion Duration | RPR | FTA-IgG | Antitreponemal IgM Antibodies | Total Antitreponemal Antibodies | Treponemal PCR | Stage of Syphilis | Treatment | Other STI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 22 | Male/heterosexual | Ulcer on the penis+bilateral inguinal lymph node enlargement | 7 days | — | + | + | + | NR | Primary | Penicillin G B 2.4MIU single dose | — |
| 2 | 36 | Male/MSM | Ulcer on the penis | 15 days | — | + | + | + | NR | Primary | Penicillin G B 2.4MIU single dose | — |
| 3 | 29 | Male/MSM | Ulcer on the penis | 14 days | — | + | + | + | NR | Primary | Penicillin G B 2.4MIU single dose | — |
| 4 | 25 | Male/MSM | Ulcer on the penis+inguinal lymph node enlargement | 5 days | — | — | + | + | NR | Primary | Penicillin G B 2.4MIU single dose | — |
| 5 | 57 | Male/heterosexual | Ulcer on the penis | 15 days | — | — | + | + | NR | Primary | Penicillin G B 2.4MIU single dose | — |
| 6 | 35 | Male/MSM | Ulcer on the penis | 2 days | — | — | + | + | NR | Primary | Penicillin G B 2.4MIU single dose | — |
| 7 | 33 | Male/MSM | Ulcer on the penis | 14 days | — | — | + | + | NR | Primary | Penicillin G B 2.4MIU single dose | Pediculosis pubis |
| 8 | 34 | Male/MSM | Ulcer on the penis | 5 days | — | — | + | + | + | Primary | Penicillin G B 2.4MIU single dose | HIV+ |
| 9 | 43 | Male/heterosexual | Ulcer on the penis | 9 days | — | — | NR | — | + | Primary | Penicillin G B 2.4MIU single dose | — |
| 10 | 43 | Male/MSM | Ulcer on the penis | 7 days | — | + | + | + | + | Primary/reinfection | Penicillin G B 2.4MIU single dose | — |
| 11 | 28 | Male/MSM | Ulcer on the penis+inguinal lymph node enlargement | 2 days | — | + | + | + | Primary/reinfection | Penicillin G B 2.4MIU single dose | HIV+ | |
| 12 | 60 | Male/MSM | Ulcer on the penis | 7 days | — | Indeterminate | NR | + | + | Primary | Penicillin G B 2.4MIU single dose | — |
| 13 | 35 | Male/heterosexual | Ulcer on the penis | 7 days | — | Indeterminate | + | + | + | Primary | Penicillin G B 2.4MIU single dose | — |
| 14 | 35 | Female/heterosexual | Ulcer on the labia majora | 20 days | — | Indeterminate | NR | + | + | Primary | Penicillin G B 2.4MIU single dose | — |
| 15 | 22 | Male/MSM | Ulcer on the penis | 7 days | — | NR | NR | + | Primary | Penicillin G B 2.4MIU single dose | HIV+, gonorrhea |
Abbreviations: CLIA, chemiluminescence immunoassay; FTA, fluorescent treponemal antibody absorption; HIV, human immunodeficiency virus; MSM, men who have sex with men; NR, not reported; NTT, nontreponemal test; PCR, polymerase chain reaction; RPR, rapid plasma reagin; STI, sexually transmitted infection; TT, treponemal test.
Fourteen of the 15 patients were men, with an age ranging from 22 to 60 years. When recording the medical history, all patients recognized risky sexual practices.
In the physical examination, all patients had a painless ulcer in the genital area (Figs. 1 and 2). The duration of these lesions ranged from 2 to 20 days. Three of these patients had associated painless enlarged lymph nodes. None of the patients presented with other mucocutaneous manifestations. All patients had negative RPR titers in serum; however, the TTs based on the presence of total antibodies (IgM and/or IgG) were positive in all cases except one. All patients underwent differential diagnosis with other STIs including hepatitis A virus, hepatitis B virus, hepatitis C virus, and human immunodeficiency virus (HIV), with 3 patients known to be previously HIV positive.
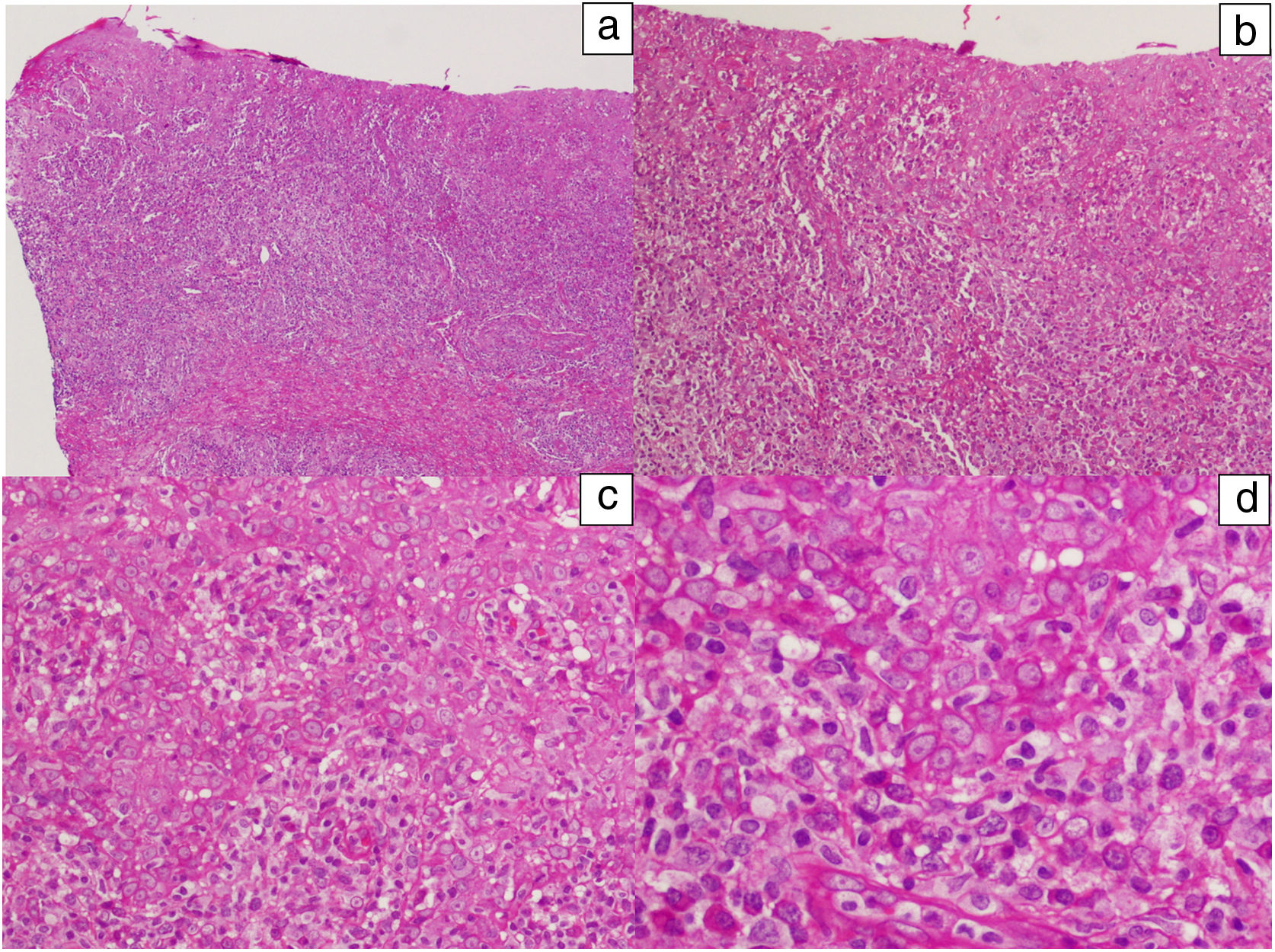
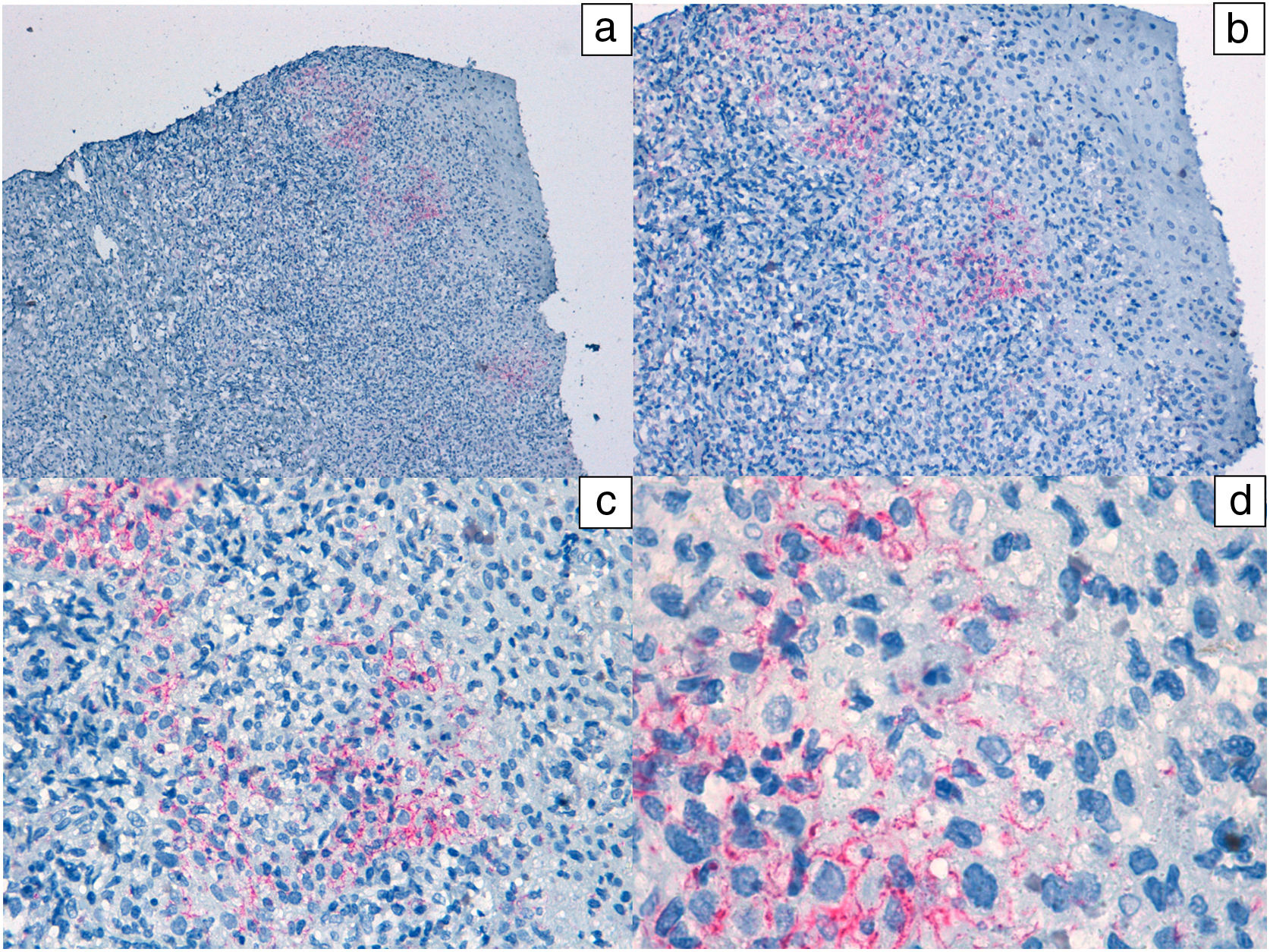
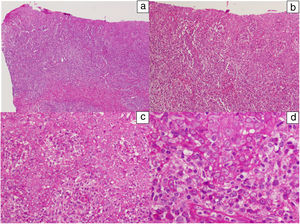
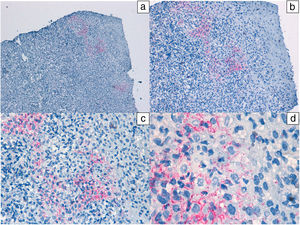
In addition, polymerase chain reaction (PCR) techniques were used in 8 patients for the detection of treponema from the ulcer exudate. The test was positive in all cases. In 2 cases, diagnosis of reinfection was established. PCR for herpes simplex virus was negative in all cases studied. In one patient, a biopsy of the lesion was performed (Figs. 3 and 4).
Histological images of a lesion with moderate irregular epidermal hyperplasia with pale keratinocytes and discrete spongiosis. There is a dense band of lymphoplasmacytic inflammatory infiltrate with involvement of the dermal-epidermal junction. Hematoxylin-eosin: a) ×10, b) ×20, c) ×40, and d) ×100.
All patients described here were diagnosed with primary syphilis and treated with a single dose of penicillin G benzathine 2.4MIU, with full resolution of the clinical symptoms. Of the 7 patients who underwent follow-up serum testing, 4 (57%) converted to positive RPR during the first 3 months, whereas the other 3 (43%) remained RPR negative.
DiscussionSyphilis, far from disappearing, affects millions of individuals annually. Dermatologists should keep up to date with the new techniques used for serological diagnosis of this disease to thus avoid erroneous interpretations.
Traditionally, the diagnostic algorithm for syphilis started with the use of an NTT such as the RPR or Venereal Disease Research Laboratory (VDRL) test. Only in the event that one of these tests was positive would a specific TT be used for confirmation.
NTTs are useful for detecting the existence of active syphilis infection, as a positive result is indicative of the presence of tissue damage. Moreover, these tests serve to determine the possibility of reinfection with past syphilis, as well as to assess the effectiveness of clinical response to treatment. The quantitative test result increases early in the course of infection, stabilizes in the secondary phase, and then gradually decreases over time, even without treatment. Clinical guidelines advise follow-up using the same NTT, whether the RPR or VDRL test, to avoid quantitative variations in the results. Seroconversion of these tests normally occurs in the first 21 days after exposure, but patients can convert to positive up to 6 weeks after infection, resulting in a delay in diagnosis. The advantage of NTTs is that they are cheap and easy to perform. The main limitation is the possibility of numerous cases of false positives resulting from viral infections, pregnancy, malignant neoplasms, autoimmune diseases, advanced age, among others.3
The TTs, or specific tests, are more used for confirming diagnosis of syphilis in patients with positive RPR or VDRL findings, as well as to rule out false positives in NTT. Classic TTs include fluorescent treponemal antibody absorption (FTA-ABS), T. pallidum particle agglutination (TPPA), and T. pallidum hemagglutination (TPHA). The drawback of these techniques is that they require expert personnel to carry them out and interpret the results. TTs detect in an exclusively quantitative manner the presence of IgG and IgM antibodies specific to components of T. pallidum using recombinant antigens.4–6 The main drawback of TTs is that the quantitative results do not correlate well with disease activity and do not allow differentiation between treated and active syphilis, as patients infected with syphilis usually remain reactive for life despite appropriate treatment.3–5 The essential advantage of TTs, in addition to their high sensitivity and specificity, is that these test are positive early in the course of infection. Antitreponemal IgM and IgG antibodies can be detected within 2 days of the onset of clinical symptoms, that is, between 2 and 4 weeks after initial infection.5,6
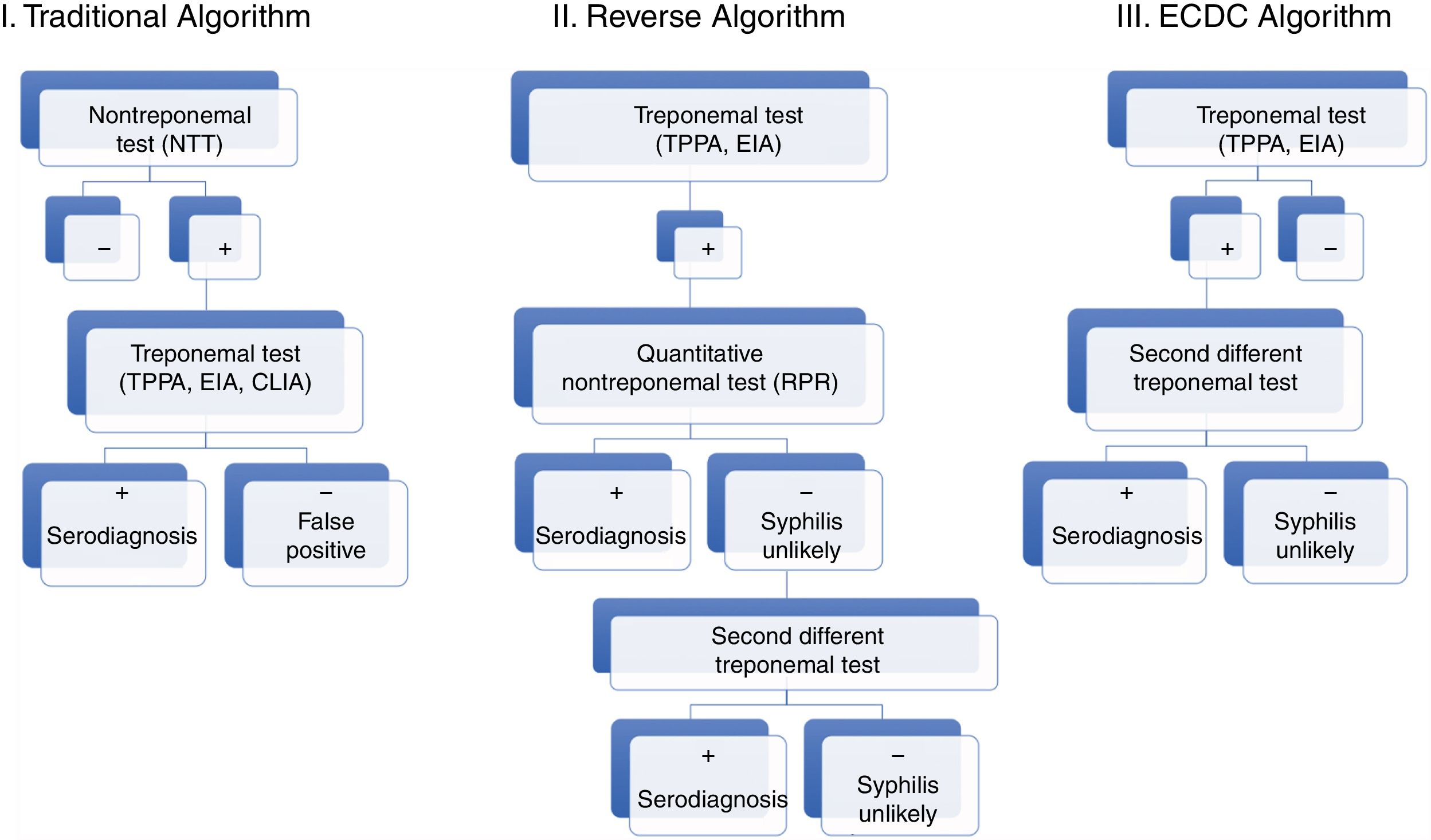
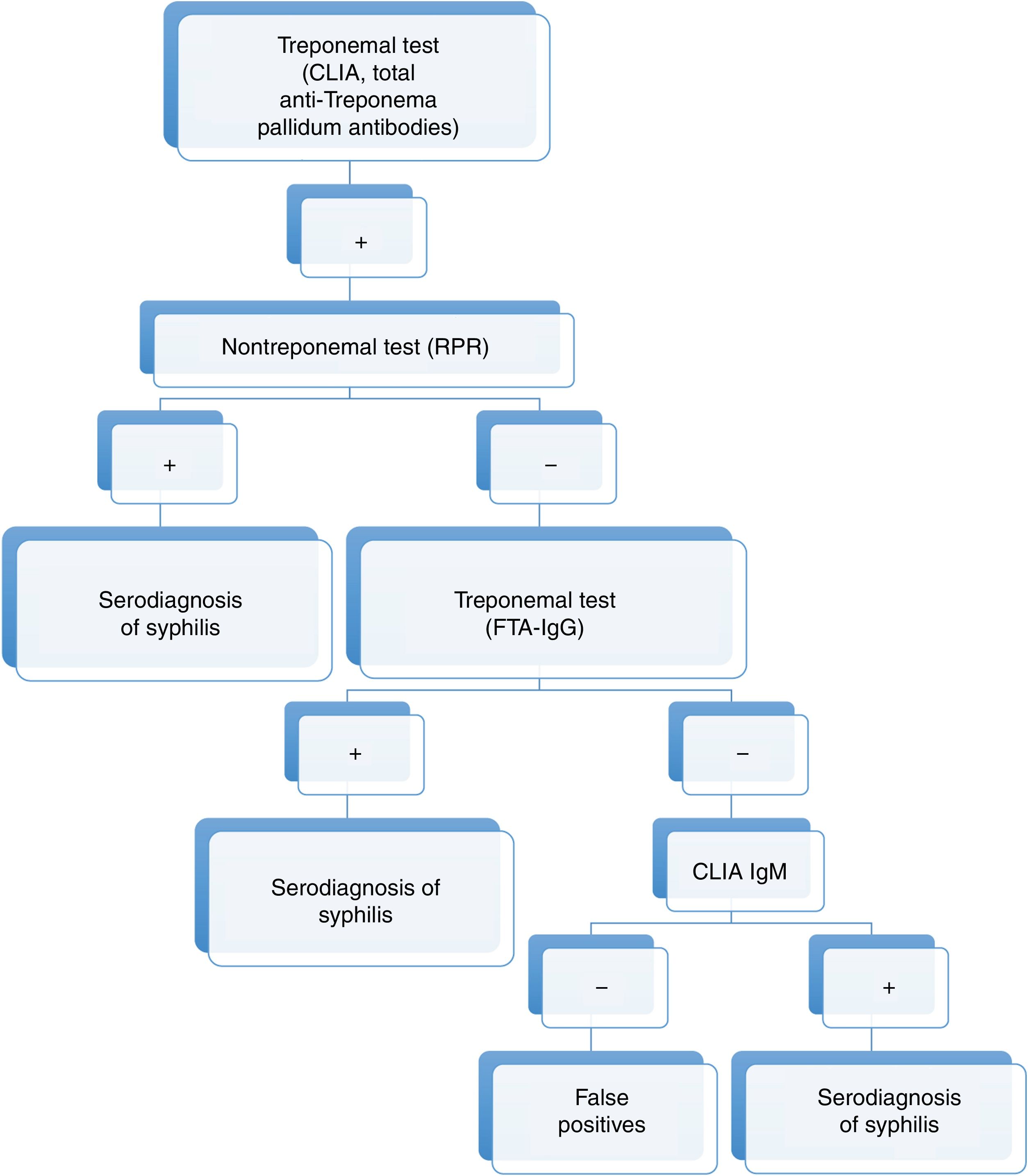
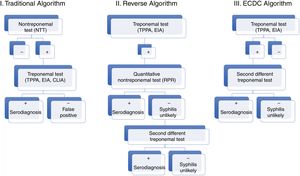
Nowadays, new automated TTs are available. These tests have a high sensitivity and can be performed rapidly, making them particularly useful for screening purposes. The automated T. pallidum enzyme-linked immunoassay (EIA) and/or chemiluminiscence Immunoassay (CLIA) are particularly noteworthy given their widespread use. These developments have led to replacement of the traditional algorithm with the reverse algorithm or the algorithm proposed by the European Centre for Disease Prevention and Control (ECDC), which are similar to the algorithm used in our hospital (Figs. 5 and 6).2
Diagnostic algorithms for syphilis (traditional, reverse, and proposed by the ECDC).
Source: taken from Man-Li et al.2
These new algorithms start with a TT (TPPA, EIA, CLIA). Subsequently, a quantitative NTT is used (usually RPR test). In the event that the NTT is negative, a second TT different to the one previously used for screening is employed.6
The FTS-ABS was considered until now the most specific method for confirming the presence of antibodies, but the new automated techniques, which also allow measurement of IgM and IgG antibodies specific to T. pallidum, have attained higher sensitivity and specificity. These automated techniques also avoid the error of observer subjectivity, which is inherent in the microscopic fluorescence technique on which the FTA-ABS method is based.3
The detection of anti-T. pallidum IgM (TP-IgM) antibodies is an important tool for the early diagnosis of syphilis, as this is the marker that appears earliest in an initial infection. The TP-IgM tests detect antibodies specific to lipoproteins of the external membrane of T. pallidum, such as Tp15 (15 KDa), Tp17 (17kDa), Tp47 (47kDa), and Tp42 (42kDa), all highly immunogenic antigens and considered the main target candidates for diagnosis. Detection of TP-IgM is strongly related to efficacy of treatment, as the concentration of this marker decreases rapidly after effective treatment while it can be detected for weeks if no treatment is administered. However, there is some controversy about its utility in cases of reinfection, given that a negative result cannot rule out diagnosis of active syphilis.1,7 Recently, Pastuszcak et al.1 ascribed relevance to these TP-IgM antibodies in individuals with HIV infection, as these patients more often have detectable concentrations of TP-IgM during the early stages of syphilis than those without HIV coinfection.
Currently, although diagnosis of syphilis is still based on serum tests, the new PCR technique performed with exudate from ulcers in patients with suspicion of primary syphilis, especially those with negative serum tests, is a supporting technique for dermatologists as it enables early diagnosis and is easy to perform.
In conclusion, the new automated serological techniques (CLIA, EIA) are useful and could be incorporated as screening tests in the diagnosis of syphilis, given their diagnostic sensitivity, rapidity, and low cost. Dermatologists in particular should be aware of the important progress in diagnostic tests and the changes in the diagnostic algorithm for syphilis that this progress has driven. The presence of an initial negative NTT according to the traditional algorithm may lead to failure to diagnose early cases of syphilis, as reflected in the 15 cases described here, with potential complications for the patient, as well as perpetuation of the epidemiological chain.8–12
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Legaz Martínez M, et al. Utilidad de las nuevas pruebas treponémicas automatizadas en el diagnóstico de la sífilis precoz. A propósito de 15 casos. Actas Dermosifiliogr. 2020;111:135–142.