The primary aim of oncologic surgery of the lower eyelid is complete tumor resection with clear margins; therefore, in some cases, the resulting defects require complex reconstructions to preserve eyelid function and achieve an acceptable cosmetic outcome. Large full-thickness lower-eyelid defects are a true challenge.1 We present a case in which we used a chondromucosal graft from the alar cartilage combined with a Mustardé-type cheek rotation flap to reconstruct a defect of these characteristics.
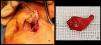
Case reportWe present a 91-year-old woman previously operated on a different center for a squamous cell carcinoma of the left lower eyelid, reconstructed with a Hughes flap. She was referred to our department for Mohs surgery after histologic confirmation of recurrence in the form of squamous cell carcinoma in situ. Two stages of Mohs surgery were required to obtain clear margins. The resulting defect involved the full thickness of the lower eyelid, affecting more than 75% of its horizontal length (Fig. 1a, b).
Description of the techniqueThe procedure was performed under general anesthesia with local anesthetic infiltration.
To reconstruct the posterior lamella, we used a chondromucosal graft harvested from the ipsilateral nasal alar cartilage.2 This graft was obtained through an external perialar approach. Local anesthesia (mepivacaine 20mg/mL and bupivacaine/epinephrine 2.5mg/0.005mg/mL) was injected subcutaneously into the nasal ala to facilitate dissection from the subcutaneous plane. The alar crease was then incised, and the ala was opened like a “swinging door,” providing direct visualization of the donor site, specifically the domus—the angle or transition zone between the medial and lateral crura of the major alar cartilage (Fig. 2a). The graft should be approximately the size of the defect, although depending on tissue laxity, posterior shortening may be necessary to avoid ectropion. Using this approach, a graft up to 25mm can be obtained, with a slightly convex shape, suitable for recreating the tarsus (Fig. 2b). The harvested graft is slightly thinned, and nasal vibrissae on the mucosal side are removed with a Colorado tip or straight Iris scissors. It is advisable to leave a small mucosal remnant on one side to evert it and recreate the eyelid margin. The intranasal donor site is coagulated with electrocautery and allowed to heal by secondary intention. The alar-crease incision is closed with 4-0 silk. The chondromucosal graft is sutured to the remaining medial and lateral tarsus, if present, or to the medial and lateral canthal tendons and to the residual conjunctiva using 6-0 absorbable sutures. The anterior lamella is then reconstructed using a Mustardé-type cheek rotation flap.
Indications and contraindicationsFull-thickness lower-eyelid defects>50% require reconstruction of both the anterior and posterior lamellae.1,3,4 Several options exist for anterior lamella reconstruction, such as cheek rotation flaps (Mustardé, Imre), transposition flaps (Tripier, nasojugal, Fricke), or V-Y advancement flaps.3–5 Regarding the posterior lamella, a Hughes flap had already been performed in this patient; moreover, it requires two surgical stages and temporary occlusion of the eye. Therefore, it is not ideal for monocular patients or those with poor vision in the contralateral eye. It is also unsuitable for patients with tumors at risk of spreading to the contralateral eyelid, such as conjunctival melanoma.2 Alternative single-stage options using autologous donor sites for the posterior lamella include: auricular cartilage graft, free tarsoconjunctival graft from the contralateral upper lid (which our patient refused), hard-palate graft, or chondromucosal graft from the septum or alar cartilage. Auricular cartilage lacks mucosa and is therefore insufficient when conjunctiva is absent and corneal protection is needed.1 Hard-palate grafts may be associated with donor-site complications such as bleeding, subperiosteal hematoma, mucosal necrosis, pain, or feeding difficulties.2 Septal grafts are technically more complex and carry risks of bleeding, nasal tip collapse, and postoperative perforation.3 Alar cartilage chondromucosal grafts are easy to harvest and have minimal donor-site morbidity, especially when taken from the described region between the lateral and medial crura of the major alar cartilage, where an optimal graft thickness, shape, and size can be obtained while minimizing the risk of nasal-ala collapse.
ComplicationsPossible complications include donor-site bleeding, corneal injury if hair remnants remain on the mucosa, ectropion, epiphora, conjunctivitis, eyelid edema, and periorbital ecchymosis/hematoma. Our patient developed only edema and ecchymosis in the immediate postoperative period (Fig. 3a–c).
ConclusionsWe highlight the use of the alar cartilage chondromucosal graft for posterior lamella replacement in large full-thickness lower-eyelid defects as a simple, single-stage alternative with low complication rates and excellent functional and cosmetic outcomes.