At the 5th World Congress of Teledermatology held in Barcelona in September 2014, the use of teledermatology (TD) in the urban environment was studied in a session entitled “New Trends in TD. Urban TD”. Dr Santiago, Dr Witkamp and Dr Romero reviewed the situation of TD in Spain and Holland, and specifically its use in the urban environment (TD-U). At that session, the presenter asked a key question to start the discussion. Does telemedicine make sense in an urban environment? In other words, if the distance to the hospital is less than 10km or even less than 20km, is a conventional face-to-face consultation (FF) at the hospital outpatient clinic not a better solution than TD? There are 3 possible answers: yes, no, or there is insufficient evidence available to support a conclusion. In fact, the answer could vary between dermatologists living in different countries, working under different circumstances, or holding different personal opinions. It is, therefore, very important to use criteria based on the best evidence available in the literature.
Our main objective in this opinion article was precisely that—to analyze the literature on TD in an urban setting from a historical perspective, focusing particularly on the advantages and disadvantages of TD-U.
Urban Teledermatology: The ConceptTD-U refers to the use of telemedicine to deliver dermatological care to patients living in cities, generally in developed countries and densely populated areas. The opposite concept is that of rural TD (TD-R), referring to the use of TD in sparsely populated rural settings, which can be generalized to any underserved area.
Clearly, no one would hesitate to use telemedicine when the distances between doctor and patient exceed hundreds or even thousands of kilometers.1 We can offer the reader some classic examples. Telemedicine has been used from Australia to the Antarctic with savings on travel of more than 7,000km; for example, the first use of a radio link to deliver medical care over 100 years ago; the link between Earth and the moon in NASA's pioneering telemedicine projects in the 1960s, 50 years ago, with a saving of over 380,000km. A more recent example, in this case relating to dermatology, is the TD service offered by the University Hospital in Tromsø,2 which has eliminated the need for a dermatologist to fly 800km every month to see patients in the Arctic town of Kirkenes. In such cases, conventional in-person consultation is almost not an option, and the use of TD is universally accepted.
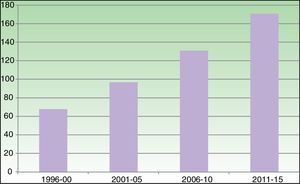
In fact, when the authors of the present article attended the first World Congress of Teledermatology in Graz more than 10 years ago (2006), we were surprised by the number of examples presented of TD-R in underserved areas, such as Alaska, the Manizales forest in Colombia, and Siberia, and, conversely, by the scant focus on TD-U. Today, however, the largest investment in telemedicine and the greatest use of these systems is in first world countries, in both sparsely and densely populated areas.3 Moreover, demographic trends indicate continued steady growth in the number of people living in densely populated urban areas and the aging of this population. It is therefore of great interest to make TD available in these densely populated areas, precisely because of the large number of potential users. This once again raises the key question of whether, if the distance to the hospital is under 10 to 20km, a conventional visit to a clinic would not be the best option? After reviewing the evidence in the literature, we can try to answer that question. We note that scientific production on the subject of TD has been accumulating steadily, reflecting the growing interest in the topic. Figure 1 shows the increase over time in the number of articles on TD published in PubMed. The United States is the country where most articles are published, followed by the United Kingdom, Spain, Holland, Italy, and Austria.4 From a historical standpoint, we can identify 3 phases in the development of TD, which are briefly analyzed below.
Reliability, Validity, and Efficiency of TD. Phase One (1996-2005)The initial phase, between 1996 and 2005, was characterized by enthusiasm, and the articles published confirmed the reliability and validity of TD. Most of the studies published in the early years demonstrated the high reliability and accuracy of telemedicine in dermatology. The results for TD were similar to those obtained in studies of conventional consultations, with respect to both the diagnosis and the management of skin disease. This equivalence was demonstrated in 42 studies of asynchronous store and forward TD (SFTD) and in 10 studies of real time TD using videoconferencing. Altogether these studies analyzed almost 8,000 patients, about 1,200 using real time TD and 6,600 using SFTD.5 The results of cost-effectiveness studies were, however, not as good. One randomized clinical trial (RCT) compared real TD and SFTD in different settings—rural and urban—in 2 places, Northern Ireland and New Zealand.6 In the overall analysis of that study, real time TD prevented more visits to hospital outpatient departments than SFTD, but was more expensive than an in-person consultation. At the time that study was carried out (2001), the most important factors in the sensitivity analysis for costs were the distances and the fixed costs for technology. TD was cost-effective only when the distance between patient and physician was over 50km. And, when this was the case, it was the patient who benefitted from the cost savings rather than the health service. In that study, the cost of the technology was the factor that determined the results. Today, however, the technology (computers, Internet access, digital cameras, etc.) is much less expensive and, as well as being more powerful, is already in place in medical settings and being used for other purposes. Consequently, the additional investment required to support TD is minimal, and the results of a similar cost effectiveness study would be very different today. Another study reported similar results, finding SFTD to be more expensive than conventional care.7 However, once again TD represented a saving in terms of the social benefit because distance is a key component of overall cost and TD reduces travel time. It also showed that TD increased the efficiency of the system because care was delivered much more promptly, a change that improved the cost-effectiveness ratio, prevented morbidity, and eliminated the need for unnecessary treatments. Distance is an important factor in efficiency, as are response time (speed of access to the specialist) and the cost of the technology.
Doubts and the Disadvantages of TD. Phase Two (2006-2010)During the second phase of its development, from 2006 to 2010, many doubts and concerns were voiced about the implementation and, most importantly, the appropriate use of TD.8 We can use this second phase to illustrate the disadvantages of telemedicine in dermatology. From Nottingham, an editorial published in 2007 defined the problems associated with TD by commenting on what we might call the 4 key articles on the topic during this phase. The first of those articles stated the obvious: FF is better than SFTD for many reasons. In TD, it is impossible to palpate the patient's skin in SFTD models it is difficult to judge what is really worrying the patient owing to the lack of direct interaction. Moreover, appropriate exploration of some areas of the skin may be omitted if these are not photographed, and correct management of the condition is impossible on the basis of poor quality images.9 Hence, our objective with TD should not be to replace FF. It should be viewed as a complementary tool and the teledermatologist cannot forget that fact. It is undeniable. The second of the 4 articles was an RCT in which teleconsultation via an SFTD system was used for all the patients in the study group.10 Using this ineffective model, only 20% of the patients avoided an outpatient appointment. What these results highlight is that patient selection is crucial in any SFTD system. It is also obvious that there is no good reason for an SFTD consultation in cases that will definitely require an in-person consultation at the hospital. The authors of the third article, a systematic review, made the point that TD was not a mature application, citing the need for more RCTs and more post-implementation RCTs.11 The final, and perhaps the most interesting arrow shot from Nottingham, was a longitudinal qualitative study12 in which the authors concluded with the view that using TD as a simple technological solution to resolve the problem of long waiting lists does not work. In other words, SFTD is not a simple or an effective way of resolving the problem of long waiting lists, at least in the short term.
Consolidation and Advantages of TD. Phase Three (2011-2016)We agree with the authors of those 4 articles and their conclusions. However, when we analyze the situation today, we see that telemedicine in general and TD in particular, is now an emerging technology. The growth in the implementation of telemedicine systems worldwide is exponential, with an expenditure of around $10 billion in 2011 growing to over $27 billion in 2016, a period of just 6 years and one characterized by economic recession.13 The greater investment in and use of these telemedicine systems is happening in first world countries, in both sparsely and densely populated areas. In Europe, the Scandinavian countries, with their low population density and high per capita income, have pioneered telemedicine systems.1 But certain very densely populated countries, such as the Netherlands and the United Kingdom, are equally active in this field.14 So, what is driving this growth and the success of TD? In our opinion, we are currently moving into a third phase: the consolidation of TD. TD is now seen as an unstoppable phenomenon and an integral part of the technological revolution currently affecting all aspects of our lives. In 2011, an editorial was published entitled “The TD train is coming: Get on board, get out of the way, or get run over”.15 The results of scientific studies carried out in recent years have started to support the use of teleconsultation in dermatology: TD is coming of age. We have already mentioned the systematic review of studies on the reliability and accuracy of TD that reported equivalence between TD and FF in diagnosis and management.5 Furthermore, an RCT found no differences in clinical outcomes between cases managed with SFTD and FF after 6 months of follow-up.16 Another systematic review showed that both real time and asynchronous TD eliminated the need for clinic-based consultations in at least half of the patients studied.17 There is a great deal of quality evidence to support the use of TD in the care of skin cancer, and the work of Spanish dermatologists is of particular note in this respect.18 Finally, another recent article about TD in the densely populated Netherlands showed that SFTD is feasible on a large scale and can provide effective care and reduce costs.14
The recent analysis by AEDV's eDermatology and Imaging Workgroup (GEDEI) reported that TD is an emerging technology in Spain.18 The number of hospitals offering TD services almost tripled in this country between 2009 and 2014 (25 to 70). By 2014, every clinic had more dermatologists handling teleconsultations than conventional visits and more hours were being spent each week on TD. An increase in the use of SFTD and a trend towards serving more patients living in urban areas was also observed. In 2014, 75% of hospitals in Spain providing TD services were delivering care to patients living less than 25km from the clinic. A similar increase in the use of SFTD systems and TD in general in the urban environment has recently been reported in the United States.19,20 In one of the largest and most important TD programs in the country, urban areas started to outstrip rural areas in the volume of TD care delivered from 2012 onwards.20
A Few Comments and the Answer to the Key QuestionHow can we explain the rapid growth and success of TD-U? It is true that the provision access to care without the need to travel long distances may be the main reason for the use of telemedicine in general and TD in particular. It is obvious that overcomes the barrier of space, but it can also break down barriers posed by time, a great benefit in both urban and rural settings. In a matter of seconds, information—including high quality video and images—can be transmitted from one place to another, avoiding thousands of kilometers of travel, dealing speedily with an urgent case or, why not, obviating the need to deal with traffic congestion or to transport very elderly patients across a densely populated city.18,21 What is not so obvious is that TD can also overcome other kinds of barriers. These include various kinds of disabilities, a particularly important aspect today owing to the progressive aging of the population in our society. And it can also overcome obstacles such as the lack of knowledge, promoting eLearning for general practitioners and thus facilitating prompt and accurate triage at the primary care level. In 2014 in Spain, 66% of the clinics or hospitals with TD services were using it to train primary care physicians. All of these advantages indicate that SFTD could be a very useful tool in many different scenarios, not just in the underserved rural areas where it has traditionally been used but also in urban areas, prisons, retirement homes, emergency response, military conflicts, and other settings.
Furthermore, urban environments also have architectural barriers, and there are generally rural areas close to modern hospitals in the West, justifying the creation of TD units because of the aging population living in both places. TD improves the efficiency of care delivery in both rural and urban settings. Several other important uses of TD are emerging: prioritization and triage of patients with cancer,22 rapid delivery of care in the case of emergencies,23,24 eLearning for family physicians, and improved coordination between primary and secondary care levels.1,18 TD helps to prevent unnecessary referrals and improves the health system's capacity to detect serious and urgent cases.
Therefore, the response to the original key question is “Yes, FF is generally better than TD, but not for all patients and not in all situations”. And “Yes, it does make sense to use teleconsultations for some patients in an urban setting, even those who live close to the hospital, because telemedicine can significantly improve the quality of healthcare in selected patients”.
At the end of this opinion article, we want to emphasize the importance of patient selection in the successful implementation of SFTD models in the urban setting. In systems designed exclusively to screen for skin cancer, in which the only decision is whether or not to refer the patient, SFTD can facilitate rapid initial diagnosis, making the use of this method justified in 100% of patients with tumors. It allows rapid prioritization of malignant lesions and obviates the need for a clinic-based consultation when the lesion is benign. By contrast, in models that refer all patients who present not just tumors but any kind of skin lesion, which are more common today in Spain, it is inefficient to handle 100% of these patients via SFTD. The ideal percentages for TD and FF have not been established and will depend on the peculiarities of each health administration. When there is a suspicion that a patient will eventually have to visit a dermatology clinic in person and the case is not urgent, referral by SFTD is not indicated. This is because the TD consultation will only duplicate the work that will be done when the patient visits the clinic, making the model inefficient. A prime example of this would be the case of multiple pigmented lesions in a patient at risk for melanoma, because proper management of such a case will always require a conventional in-person consultation.
A rational target might be between 10% and 50% of referrals via TD, depending on the particular circumstances in each hospital, preferably using SFTD (Table 1) for patients with limited mobility and for cases requiring rapid prioritization and prompt care, for example initial treatment of dermatological emergencies (pemphigoid flare, severe urticaria, etc.) or a potentially serious condition. In this phase, SFTD represents the best option for skin cancer screening, avoiding FF for unimportant lesions, such as seborrheic keratosis, which tend to overload the offices of specialist dermatologists, and prioritizing patients with melanoma, assigning them an early appointment by moving them up the waiting list. Another situation in which SFTD may be indicated is when a general practitioner is interested in a particular case for their own ongoing training or because they are unsure about how to manage the condition. This practice can prevent diagnostic errors and inadequate treatments, as well as the morbidity and expense these entail.
Proposed Objectives and Selection of Patients for Referral Via Teledermatology.
| Objectives |
| 1. Target: 10%-50% of all referrals |
| 2. Improve access to care |
| 3. Selection and prioritization |
| 4. Coordination with primary care and GP training |
| Selection of patients referred via TD |
| 1) Only patients meeting the normal criteria for referral (in-person consultation) |
| 2) Any skin condition can be screened using SFTD. In the following circumstances, however, referral by TD may be preferable: |
| a) Limited mobility or other accessibility problem: patients with disabilities or who are elderly, bed-bound, live at a distance or in a rural area, and those who have scheduling difficulties (because of the demands of their work or a social problem) |
| b) Urgent cases in which prompt assessment could reduce morbidity and cost |
| c) Interest on the part of the primary care physician in training and learning how to resolve doubts or avoid errors in management |
| d) Skin cancer cases in order to: |
| i) Reduce response time |
| ii) Refer the patient directly for dermatological surgery |
| iii) Improve the expertise of primary care physicians, thereby making the system more sustainable by improving gatekeeper efficiency. |
| e) When it appears that the case can be managed by TD. By contrast, avoid TD when management will inevitably require an in-person consultation (for example, patients with multiple pigmented lesions). |
TD is a very complex activity in which we can only achieve success if we have clearly defined objectives. The main objective should never be merely to deal in the short term with unacceptably long waiting lists, because it has been shown that TD does not achieve this goal.8,10,12 The objective of a TD service should be to enhance the quality of the care delivered to selected patients, improving accessibility and the classification and prioritization of each case, while at the same time optimizing coordination with primary care physicians and contributing to their ongoing training.25 These objectives are of interest in all types of patients, irrespective of whether they live in a rural or an urban environment.
TD is ready for a worldwide roll-out. This is already happening, as can been seen by the significant increase in its use everywhere. And to ensure that TD is used appropriately, it is dermatologists who should lead this implementation on the basis of scientific criteria.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Romero-Aguilera G, Ferrandiz L, Moreno-Ramírez D. Teledermatología urbana: concepto, ventajas y desventajas. Actas Dermosifiliogr. 2018;109:471–475.