Hyperhidrosis affects 3% of the population.1 Its management includes topical, systemic, and surgical therapies.2 Occasionally, it is a manifestation of other conditions such as thoracic outlet syndrome (TOS), also known as superior thoracic outlet syndrome. Below, we describe 2 patients with TOS-induced hyperhidrosis.
A 23-year-old woman with a 6-year history of anemia treated with oral iron consulted for edema and increased sweating in her right hand. Recently, she had noticed worsening with a burning sensation and an inability to close her hand. Additionally, the patient reported distal cyanosis.
On physical examination, edema, erythema, and hyperhidrosis were observed on the right palm, along with acral cyanosis (Fig. 1). Palpation of the right supraclavicular region elicited pain that was not reproduced contralaterally. The Adson test turned out positive.
A chest X-ray and ultrasound of the right upper limb were performed, showing no abnormalities.
An electromyogram revealed a mixed sensory-dominant neuropathy in the right median, ulnar, and radial nerves.
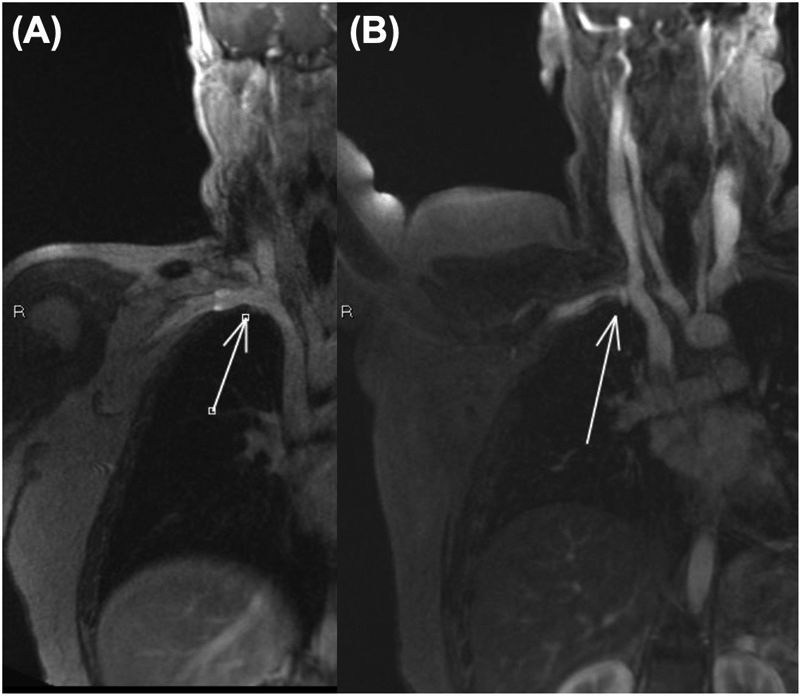
Dynamic magnetic resonance imaging (MRI) in abduction showed compression of the brachial plexus and subclavian vein at the costoclavicular space, which resolved in the anatomical position (Fig. 2).
She was diagnosed with mixed neurogenic and venous right TOS and referred to Thoracic Surgery and Vascular Surgery, where conservative management was recommended. The clinical outcome is unknown due to loss to follow-up.
A 27-year-old woman—a smoker with no other relevant personal history—presented with a 5-year history increased sweating in the left axilla and hand. Additionally, she reported cervicalgia, pain, and paresthesias in the left upper limb. Physical examination revealed hyperhidrosis in the left upper limb. A chest X-ray showed no abnormalities, while a cervical X-ray revealed bilateral mega-transverse processes at the C7 vertebra.
Dynamic MRI showed complete occlusion of the left subclavian vein at the costoclavicular space with forced abduction of the limb.
She was diagnosed with mixed neurogenic and venous TOS and referred to Vascular Surgery. She initiated rehabilitative treatment without improvement. Decompressive surgery was proposed, but the patient declined. Follow-up was subsequently lost.
TOS affects 8–25 people per million inhabitants per year. It predominates in women,3 with a higher incidence rate between 20 and 50 years of age.4
Three subtypes are distinguished: neurogenic, due to compression of structures of the brachial plexus, accounting for over 90% of cases5; venous, due to compression of the subclavian vein; and arterial, due to compression of the subclavian artery.5 The venous subtype accounts for 3–5% of cases, and the arterial subtype for <1%.3 Combined forms may occur.3
Compression can occur in the scalene triangle, costoclavicular space, or pectoralis minor space. It may be due to a cervical rib, muscular anomalies of the scalene triangle, or trauma.3,5
Clinical presentation is varied and depends on the affected structures. Nerve compression may be associated with pain, paresthesias, and loss of strength. These symptoms worsen with upper limb abduction or weight-bearing and improve at rest.6
Reflecting autonomic involvement, hyperhidrosis, reflex sympathetic dystrophy, or vasomotor symptoms may be observed.
Edema and cyanosis may occur due to venous compression, or pallor, coldness, and signs of ischemia due to arterial compression.5
The diagnosis is clinical and requires a thorough history and physical examination.
The Adson test involves asking the patient to elevate the chin and hyperextend or flex the neck toward the affected side. It is considered positive if it reproduces the symptoms.6,7
A cervicothoracic X-ray can rule out skeletal abnormalities, such as the presence of a cervical rib6 or a Pancoast tumor, which could present with symptoms similar to TOS.
MRI is a technique capable of differentiating the affected structures. It allows dynamic studies by reproducing symptoms and visualizing the compression point.6 It could be considered the diagnostic imaging modality of choice.
Arteriography is reserved for cases of arterial TOS where surgical management is considered or when the limb has been compromised.5 It is not useful in diagnosing neurogenic TOS. In some centers, this technique has been replaced by computed tomography angiography.5
Treatment requires a multidisciplinary approach. A total of 80% of patients respond to conservative rehabilitative treatment.8,9 Decompressive surgery is reserved for patients with poor clinical progression or limb compromise.8,9
We describe 2 cases in which unilateral hyperhidrosis was the key symptom of TOS. Understanding the pathophysiology and associated clinical features is required to consider this diagnosis in such patients.
Conflicts of interestNone declared.