A 61-year-old woman, originally from Venezuela and residing in Argentina for the past 18 months, with no relevant past medical history, presented with an asymptomatic hypochromic macule on the inner aspect of her right forearm. The lesion had been present for several years and had progressively increased in size.
Physical examinationA smooth hypochromic macule with sharply demarcated but slightly erythematous borders was noted, measuring approximately 5cm×4cm (Fig. 1). Thermal and pain sensitivity over the lesion were diminished.
HistopathologyHistological examination of a punch biopsy revealed dermal granulomas composed of epithelioid cells and Langhans-type giant cells, surrounded by a lymphocytic corona, in contact with the epidermis and encircling edematous nerve fibers and blood vessels. No acid-fast bacilli were identified using the Ziehl–Neelsen technique.
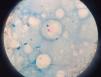
Additional studiesAn imprint smear from the skin biopsy turned out negative. Ziehl–Neelsen-stained bacilloscopy from both earlobes and bilateral nasal smears yielded positive findings: bacteriological index (BI) 2+ and morphological index (MI) 60% with scant globi in the right nasal smear, and BI 1+ and MI 50% with scant globi in the right earlobe smear (Fig. 2). Routine blood tests were within normal limits.
What is your diagnosis?
DiagnosisIndeterminate leprosy evolving toward borderline (dimorphous) leprosy.
Disease progression and treatmentThe patient received MMR therapy – moxifloxacin 400mg, rifampicin 600mg, and minocycline 100mg monthly for 12 months – because the classic multidrug regimen was not available in Argentina.
CommentaryLeprosy is one of the oldest known infectious diseases. It remains present in 120 countries despite being curable, having free global treatment availability, and a low rate of transmission (requiring close and frequent contact with a bacilliferous individual plus a susceptible immune system). According to the World Health Organization, leprosy was eliminated as a public health problem globally in 2000 (prevalence <1 case per 10,000 inhabitants). However, by 2009, >10,000 new cases per year were reported in several countries in Africa, Asia, and Latin America.1,2
This reality is largely unknown not only to the general population but also to many healthcare professionals who mistakenly consider leprosy an ancient, eradicated disease and absent from their region. This contributes to diagnostic delays, disease progression, and increased morbidity.
Indeterminate leprosy is the earliest clinical form of the disease and occurs in individuals lacking an adequate cellular immune response to eliminate the bacillus. It is the most difficult form to diagnose and requires high clinical suspicion. It presents with one or a few clean, dry, hypochromic macules in lighter phototypes and coppery macules in darker phototypes, usually 2–4cm in diameter, with poorly defined borders giving a “dirty” appearance to the perilesional skin. Lesions can appear on any part of the body. The cardinal sign for clinical diagnosis is hypoesthesia or dysesthesia due to involvement of small nerve fibers, initially affecting thermal sensation, then pain. Internal organs and mucous membranes are not affected.3,4 When the disease begins to shift toward either pole of the immunological spectrum, mild erythema or slight infiltration of the lesion borders may appear.5
Indeterminate leprosy may persist for up to 5 years. A small proportion of patients achieve spontaneous resolution, whereas in the majority, the disease progresses.
Diagnosis is not always straightforward, even with strong clinical suspicion and appropriate additional tests; in many cases, clinical evolution ultimately defines the disease. It is essential to continue educating both the public and healthcare providers to raise awareness that leprosy is a curable disease, to eliminate prejudice, and to reduce stigma and discrimination. Currently, leprosy remains a present disease – and it is curable.
Conflict of interestThe authors declare no conflict of interest.