A 74-year-old man with no relevant history was referred to our department for evaluation of a lesion of 18 months’ duration on the right foot that made walking difficult. He had no remarkable personal or family history and did not report any travel, contact with animals, or insect bites. He was not taking any medication.
Physical ExaminationPhysical examination showed a single protruding nodular lesion with an ulcerated surface and a diameter of 2.5cm×2cm on the medial aspect of the right big toe (Fig. 1). He reported discomfort and occasional bleeding on walking. The rest of the physical examination was normal.
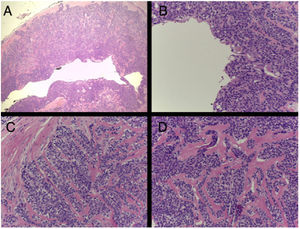
HistopathologyHematoxylin–eosin staining showed a well-circumscribed, nonencapsulated dermal lesion with cellular lobules, branched tubular structures, and a markedly hyalinized stroma (Fig. 2). There were 2 intermixed cell types: one with eosinophilic cytoplasm and large, central nuclei and another with clear cytoplasm and smaller, eccentric nuclei.
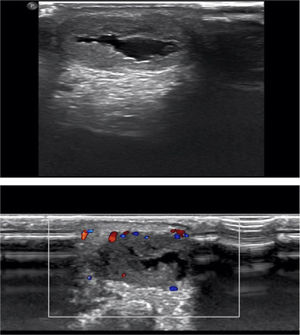
Additional TestsUltrasound showed a cystic area with well-defined borders and posterior acoustic enhancement (Fig. 3) The Doppler study showed minimal activity at the periphery of the tumor.
What Is Your Diagnosis?
DiagnosisNodular hidradenoma.
Treatment and OutcomeThe nodule was completely excised and there have been no recurrences to date.
DiscussionNodular hidradenoma is a rare benign tumor derived from the distal portion of the sweat glands. It has several synonyms, including clear cell hidradenoma, clear cell myoepithelioma, and eccrine acrospiroma.1 Until a decade ago, it was thought to be derived from the eccrine sweat glands, but recent findings (decapitation secretion, continuity through follicles, mucin production, and GCDPF-15 positivity in immunohistochemical studies) point more to an apocrine origin.2
Nodular hidradenoma generally appears in the fourth or fifth decade of life. It is very rare in children and slightly more common in women than in men. It has a predilection for the head, neck, trunk, and limbs, although it can occur anywhere.3
The clinical features of nodular hidradenoma are nonspecific. The tumor usually presents as an asymptomatic, slow-growing, nodular or solid cystic lesion with a diameter of 0.5 to 2cm. Serous or bloody discharge is sometimes observed. The overlying skin may be normal or atrophic, with a range of possible colors, including pink, orange, brownish, and red-blue.3 As occurred in our patient, the lesion may be ulcerated.
Histologically, nodular hidradenoma presents as a well-circumscribed, nonencapsulated nodular tumor. It is predominantly dermal, but can extend into the subcutaneous tissue. The epidermis is usually spared, although focal attachments are sometimes seen, on occasions the entire epidermis may be replaced, similarly to in eccrine poroma.
Nodular hidradenoma has a biphasic cell population, with frequent transition between cell types. Some areas show round, fusiform, or polygonal cells with eosinophilic cytoplasm and round or oval nuclei, while others show clear cells with clear cytoplasm and small, dark, eccentric nuclei.4
Atypical features such as nuclear pleomorphism, hyperchromatism, giant cells, and increased mitotic activity are sometimes observed. In such cases, the tumor is called atypical hidradenoma.2 These features are associated with a higher risk of recurrence and have potential for malignant transformation, hence the recommendation to perform a second operation with wide excision and more regular follow-up. Excision is normally curative, but follow-up is recommended to rule out the unlikely, but possible, occurrence of malignant transformation.3
Familiarity with nodular hidradenoma is important due to the broad differential diagnosis, which, like in our case, includes benign tumors (e.g., other adnexal tumors, dermatofibroma, and epidermoid cyst) and malignant tumors (basal cell carcinoma, squamous cell carcinoma, and melanoma).
Conflicts of InterestThe authors declare that they have no conflicts of interest.