Trichotillomania (TTM) is an obsessive–compulsive disorder in which affected individuals recurrently pull-out hair from any region of the body, causing hair loss or alopecia. The management of TTM is a therapeutic challenge for dermatologists and consists of a combination of pharmacological and non-pharmacological alternatives. Cognitive-behavioral therapy has successfully been used to treat TTM. However, not all patients are willing to follow this treatment strategy. Unconventional support tools are proposed, such as electronic devices, Internet therapies and microneedling. N-acetylcysteine and memantine are considered suitable first-line therapies thanks to their favorable safety and efficacy profile, low risk of adverse effects, and significant benefits. The use of other drugs, including fluoxetine, clomipramine, olanzapine, and naltrexone has limited evidence of variable efficacy. The present review illustrates the current treatment modalities for the management of TTM.
La tricotilomanía (TTM) es un trastorno obsesivo-compulsivo en el que los sujetos afectados se arrancan el pelo de cualquier región del cuerpo de forma recurrente, provocando una pérdida de pelo o alopecia. El tratamiento de la TTM es un reto terapéutico para los dermatólogos, y consiste en un tratamiento combinado de alternativas farmacológicas y no farmacológicas. La terapia cognitivo conductual se ha utilizado con éxito en el tratamiento de la TTM, pero no todos los pacientes quieren o pueden cumplir con esta estrategia de tratamiento. Se proponen herramientas de apoyo no convencionales, como dispositivos electrónicos, terapias vía internet y microneedling. Se ha descrito la eficacia de la N-acetilcisteína y la memantina como alternativas adecuadas de tratamiento de primera línea debido a su perfil de seguridad favorable, con bajo riesgo de efectos adversos y beneficios significativos. El uso de otros fármacos, incluyendo la fluoxetina, la clomipramina, la olanzapina y la naltrexona, presentan una evidencia limitada de eficacia variable. Esta revisión presenta las modalidades actuales de tratamiento en el manejo de la TTM.
TTM is defined in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, Text Revision (DSM-5-TR), as an obsessive–compulsive (OCD) or related disorder characterized by subjects recurrently pull out hair from any body region, resulting in hair loss that, in diffuse patterns, might not be noticeable.1,2
EtiopathogenesisThe etiology of TTM is yet to be elucidated. Multiple independent or interrelated factors may contribute to its development, including genetic, psychological, social, and neurobiological factors.3 TTM has been categorized into 2 types: automatic, where the action is unconscious, and focused, which occurs consciously in response to situations of emotional stress, sadness, anger, or anxiety.2 It has been proposed that hair pulling produces a “counterirritation” phenomenon that reduces the brain's perception of stress.3
Clinical presentationClinically, TTM may present with a pattern of diffuse scalp involvement, irregular non-scarring alopecia in patches, or with 1 or 2 plaques (Figs. 1 and 2).2 Although the scalp is the most widely affected anatomical location, the eyebrows, eyelashes, limbs, pubic area, armpits, and anterior chest hair may also be affected. The alopecia pattern is often localized or diffuse with angular or irregular borders. Patients with TTM exhibit hairs of different lengths, creating a rough sensation when touching the scalp.2,3 TTM has a prevalence of 0.5% up to 2% of the population, with a female predominance of 4:1.2
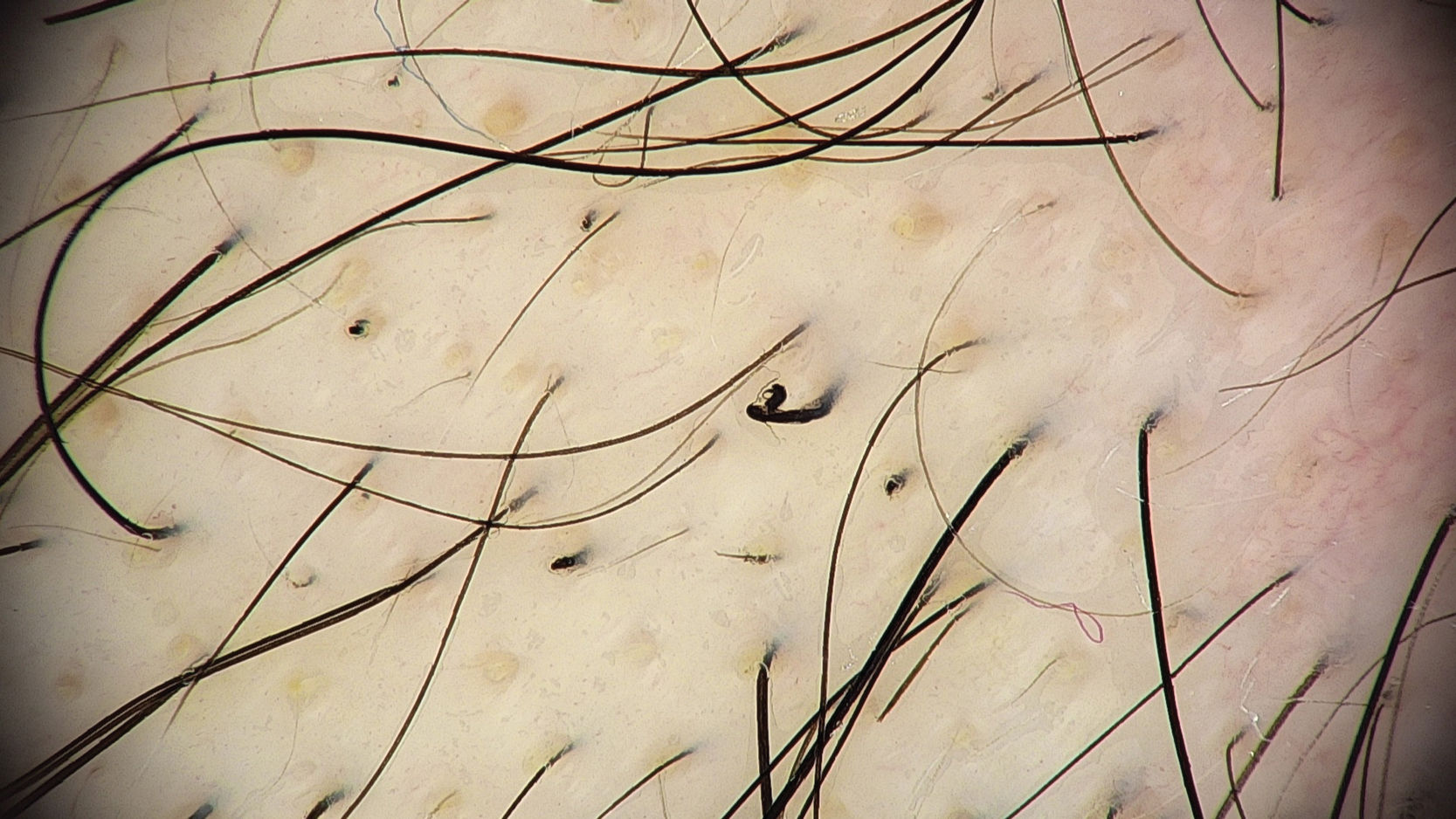
Trichoscopy reveals abnormalities resulting from stretching and breaking of hair shafts. Common trichoscopic signs include reduced hair density, black dots, broken hair shafts at different lengths, and yellow dots (Figs. 3 and 4). Other trichoscopic signs have been described, all representative of broken hair shafts.1,2,4
In the presence of diagnostic doubts, skin biopsy may be useful, where specific histological findings including trichomalacia and pigmented casts can be observed. Non-specific histological findings include follicular plugging, reduced number of follicles, inverted anagen-to-telogen ratio, decreased number of sebaceous glands, hyperpigmentation, increased number of fibrous tracts and vellus hairs, superficial dermal inflammation, evidence of hemorrhage, and presence of hair granulomas.3
ComorbiditiesThe prevalence of concomitant illnesses is up to 80%, with the most common being major depressive disorder, social anxiety disorder, OCD, post-traumatic stress disorder, and attention-deficit hyperactivity disorder.5
Course of the diseaseTTM is usually a chronic disorder with fluctuations in intensity over time. Various factors such as age and psychiatric comorbidities influence prognosis.1,2
Approximately 20% of patients exhibit trichophagia, which can lead to trichobezoars and GI disturbances requiring surgery.2 This disorder may have a limited course. An epidemiological study that recruited a total of 10,169 adults with current or past TTM, examined them via online surveys, and found that approximately 24.9% of individuals experienced remission without medical treatment or psychotherapy.6
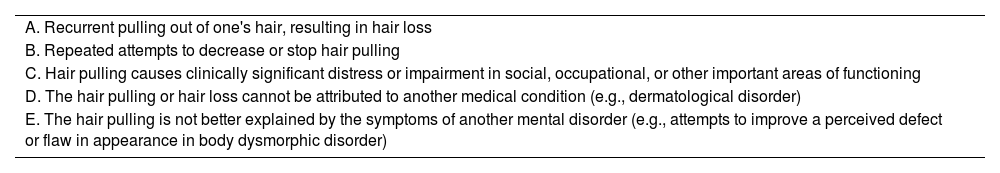
DiagnosisThe DSM-5-TR diagnostic criteria for TTM are listed in Table 1.1
Diagnostic criteria for trichotillomania according to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, Text Revision (DSM-5 TR).
| A. Recurrent pulling out of one's hair, resulting in hair loss |
| B. Repeated attempts to decrease or stop hair pulling |
| C. Hair pulling causes clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| D. The hair pulling or hair loss cannot be attributed to another medical condition (e.g., dermatological disorder) |
| E. The hair pulling is not better explained by the symptoms of another mental disorder (e.g., attempts to improve a perceived defect or flaw in appearance in body dysmorphic disorder) |
The differential diagnosis of trichotillomania primarily includes alopecia areata. The trichoscopy of both entities may show some common signs, such as exclamation mark hairs, tulip hairs, or black dots. The main difference is the presence of cut hairs at different levels in TTM, something that does not occur in the inflammatory process of alopecia areata, which produces a more homogeneous interruption of the hair anagen phase.
Other differential diagnoses include scalp ringworm, traction alopecia, telogen effluvium, and secondary syphilis.2,3
Non-pharmacological treatmentCognitive-behavioral therapyCognitive-behavioral therapy (CBT) is one of the most widely used treatments for TTM.1 It focuses on identifying and modifying dysfunctional thoughts and behavioral patterns. In patients with TTM, the habit reversal technique (HRT) is used to help them identify signals preceding hair-pulling to replace this behavior with healthier and adaptive responses.7
Nine controlled studies (27 participants on average) evaluated the effects of HRT plus CBT for TTM treatment. A meta-analysis showed a significant difference in favor of CBT plus HRT for improving symptoms (SMD [95%CI]2=−1.66 [−2.31, −1.02], p<0.0001).8
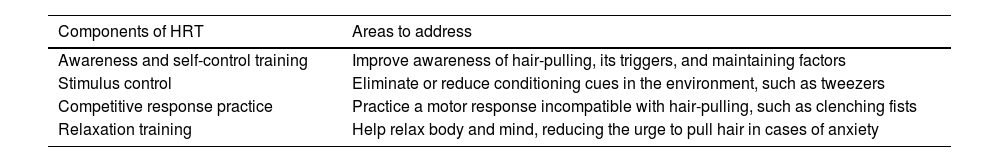
HRT is offered with a structured approach that uses core components9 (Table 2).
Core components of habit reversal therapy for treating patients with trichotillomania components.9
| Components of HRT | Areas to address |
|---|---|
| Awareness and self-control training | Improve awareness of hair-pulling, its triggers, and maintaining factors |
| Stimulus control | Eliminate or reduce conditioning cues in the environment, such as tweezers |
| Competitive response practice | Practice a motor response incompatible with hair-pulling, such as clenching fists |
| Relaxation training | Help relax body and mind, reducing the urge to pull hair in cases of anxiety |
A social support system is also often established.9 HRT using various toys has also proven effective in younger children.10 In selected cases, other therapy modalities may be effective.2
Electronic devicesElectronic devices are proposed to enhance the effectiveness of HRT. They monitor the frequency of behaviors and alert the patient of hand-to-head contact.9,11
An open trial included a device called AEMD (Awareness Enhancing and Monitoring Device), a unit for the neck and 2 wristbands with vibration alert functions that would continue until the patient had pressed a button (Fig. 5).11 After 9 HRT sessions, with weekly medical supervision, 13 out of 19 participants reported having “improved significantly.” There was patient dissatisfaction with the neck unit design.11,12
AEMD device. Neck unit and wristbands.11
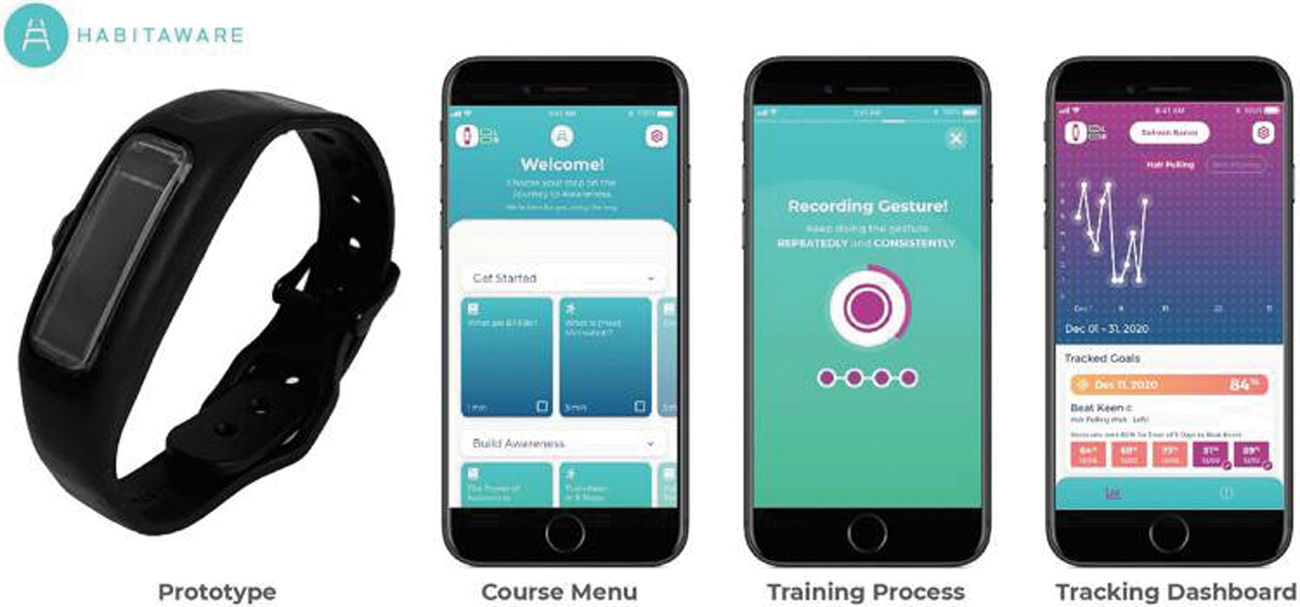
In a 4-week pilot study, 15 adults with TTM used a motion-detection wrist device and a mobile app (n=10), or just the wristband (n=5), developed by HabitAware® (Minneapolis, United States) for a mean 12.8h daily (Fig. 6).13
Prototype of a HabitAware® motion-detection device: wristband and accompanying app.1
Via Likert scale survey, they reported that the device and app were effective in increasing awareness of hair-pulling (M, 4.40; SD, 0.84) and reducing the behavior (M, 4.30; SD, 0.95).13
Internet therapyDue to economic, geographic, and social stigma reasons, patients may not accept or complete CBT. Asplund et al. conducted a study with 25 adult patients with TTM (n=7) or dermatillomania (n=18). They received 10 CBT modules via the Internet. They monitored pulling/pinching and had to complete tasks to access the next weekly module. They always interacted with the same therapist, and 43% of TTM participants achieved clinically significant changes, as defined by Farhat et al. Results were also significant at the 6-month follow-up.14
MicroneedlingThe use of microneedling with a “dermaroller” has been proposed by Christensen et al. as a tool for HRT. Three cases were described—1 adolescent and 2 adults—who were instructed to use a 0.5mm needle dermaroller on their scalp whenever they felt the urge to pull their hair. Topical minoxidil foam was also prescribed. They were evaluated at 6 and 12 months, showing significant clinical improvement, confirmed by trichoscopy. Microneedling is thought to stimulate hair growth and provide a sensation similar to pulling hair. The use of micro-needles for TTM is similar to ccertain harm-reduction strategies used for patients who self-harm; however, more controlled studies are needed to evaluate its efficacy.15
Pharmacological treatmentSelective serotonin reuptake inhibitorsStudies comparing fluoxetine and placebo did not show significant differences in reducing the urge to pull hair, time spent pulling, or number of hairs pulled.2 The inclusion of SSRIs in the therapeutic regimen is reasonable due to the psychiatric comorbidities for which their efficacy is well-established, such as anxiety, depression, and obsessive–compulsive disorder.1,2
Tricyclic antidepressantsClomipramine blocks the reuptake of norepinephrine and serotonin in the synaptic space while blocking the cholinergic muscarinic, adrenergic, histamine H1, and serotonin 5-HT2 receptors. Due to its pharmacological profile, it has been widely used in the treatment of OCD.8 A controlled clinical trial compared clomipramine, CBT, and placebo, finding that CBT was significantly more effective than clomipramine (p=0.016) or placebo (p=0.026) in reducing TTM symptoms.8 Adverse effects are relatively common and include dry mouth, constipation, drowsiness, and sedation.2
N-acetylcysteineN-acetylcysteine (NAC) is the acetylated precursor of the amino acid l-cysteine. It works as a glutamate modulator and antioxidant. It is widely known as a mucolytic, antidote for paracetamol overdose, and nephroprotective agent for contrast administration.16 In a 12-week controlled trial with 50 patients with TTM, a dose of 1200 up to 2400mg/day achieved an average symptom reduction of 40.9% on the primary outcome measure, MGH-HPS (Massachusetts General Hospital Hair Pulling Scale), and a response rate of 56% (“significant improvement” or “very much improved”) on the Clinical Global Impression Scale (CGI) after a 9-week regimen vs placebo. No adverse effects were described.16 NAC is generally well tolerated, and other controlled trials have described similar results.
In children, the results have proven unsatisfactory.17 Possibly, children do not respond to NAC as adults do, because the hair-pulling pattern in children is probably predominantly automatic.2,8,18
Nausea, vomiting, diarrhea, and constipation have been reported with doses<2400mg/day. At doses>2400mg/day, fever, chills, skin rashes, and headaches may occur. NAC should be used with caution in asthmatics, patients prone to anaphylactic reactions, and patients susceptible to fluid overload.16
MemantineMemantine is a non-competitive antagonist of the NMDA (N-methyl-d-aspartate) receptor. It is primarily used for the preservation of cognitive function in moderate-to-severe Alzheimer's disease.
A randomized, double-blind, 8-week clinical trial with memantine (10mg/day up to 20mg/day) or placebo included a total of 100 adults with TTM or dermatillomania. The modified NIMH (National Institute of Mental Health) TTM Symptom Severity Scale was used. A total of 60.5% of participants in the memantine group improved “significantly” vs 8.3% of participants from the placebo group. The drug was well tolerated, except in 2 cases that required discontinuation due to dizziness.19
Greenberg et al. indicate that further research is needed, especially to analyze TTM and dermatillomania separately, and to better understand the low placebo response rate in this study.20
AntipsychoticsOlanzapine is the most studied antipsychotic for the treatment of TTM. A 12-week, placebo-controlled study (n=25) evaluated the effects of olanzapine (target dose 20mg/day) for the treatment of TTM. A significant effect in favor of olanzapine was shown (85% vs 17% in the placebo group). Efficacy was measured using the Clinical Global Impression Scale. At least 1 adverse event was reported in 21 participants.1,2,8 Since olanzapine has been associated with metabolic syndrome, its use should be considered in association with its safety profile.18
NaltrexoneNaltrexone is an opioid receptor antagonist, approved as a supportive treatment for alcohol and opioid addiction. In dermatology it is used off-label for the treatment of TTM and other dermatoses, at doses of 50–100mg per day.2,21
A 10-month pilot study with 14 children with TTM and on a mean dose of naltrexone (66.07±22.23mg/day) found that 78% improved. At the final visit, 3 (21.4%) children said they did not pull their hair at all, while 8 (57.1%) improved their hair-pulling frequency.22
However, these results differ from the findings of Grant et al.23 in a double-blind, 8-week study with a target dose of 150mg/day, where naltrexone did not show any significant differences in reducing the urge to pull hair vs placebo.
In both studies, therapy was well tolerated, with only mild sedation being reported. These contradictory results could be due to differences in age groups and treatment duration. More studies are needed to define the efficacy of naltrexone in the management of TTM.2,21,22
DronabinolDronabinol is a synthetic cannabinoid. In an open trial with 12 patients, 2.2–15mg/day of dronabinol—which was well-tolerated—reduced hair-pulling behavior in 75% of the patients.1 However, a double-blind, placebo-controlled study with 50 adults with TTM (n=34) or dermatillomania (n=16), which assessed the efficacy of dronabinol at doses of 5–15mg/day vs placebo found no differences in symptom reduction.2,24 Dronabinol-related adverse effects are mainly confusion, dizziness, euphoria, and drowsiness.24
Monoamine oxidase inhibitorsGrant et al. presented a case series of 5 individuals whose TTM did not improve with, at least, 1 cycle of CBT, NAC—an antipsychotic—and a SSRI. Therapy was initiated with phenelzine or tranylcypromine. There was a marked clinical improvement in 2 patients (>40% improvement) with phenelzine, 1 improved with tranylcypromine, but 2 did not (<10%) with phenelzine. In 2 out of the 3 patients who improved, there was concurrent depression. Monoamine oxidase inhibitors could be considered in cases in which first-line alternatives fail to control the symptoms.25
ConclusionsThe treatment of TTM is a therapeutic challenge for dermatologists and requires a multidisciplinary approach with various methods, including psychotherapy and pharmacological treatment. CBT is the therapeutic alternative with the most efficacy evidence available, particularly HHRT.
When choosing treatment, the presence of psychiatric comorbidities and their temporal relationship with TTM should be considered. If the comorbidity is due to the effects of hair-pulling, it is advisable to focus the approach on the action of hair-pulling per se. If no temporal relationship is found, behavioral therapy should include cognitive approaches aimed at patients with ≥1 disorders. Regarding pharmacotherapy, many patients with comorbidities may require drugs that have proven ineffective in TTM clinical trials. The common adverse effects associated with each drug should also be taken into account.2,18
Given the lack of universally accepted and approved treatment options for TTM, further studies with stronger evidence are essential to improve the therapeutic approach for these patients. The usefulness of new technologies and techniques in the treatment of TTM, such as online therapies, applications, vibratory devices, and microneedling, can also be considered.