Lentigo maligna (LM) is an in situ melanoma, for which the treatment of choice is surgical excision using Mohs surgery, making it possible to spare healthy skin and ensure the lack of involvement of surgical margins.1 Defining the clinical margin of LM and lentigo maligna melanoma (LMM) by means of clinical and dermoscopic examination can be challenging when planning surgical excision. We report 3 cases of LM and LMM, in which the use of Wood's light helped to better delineate the lesions before surgery.
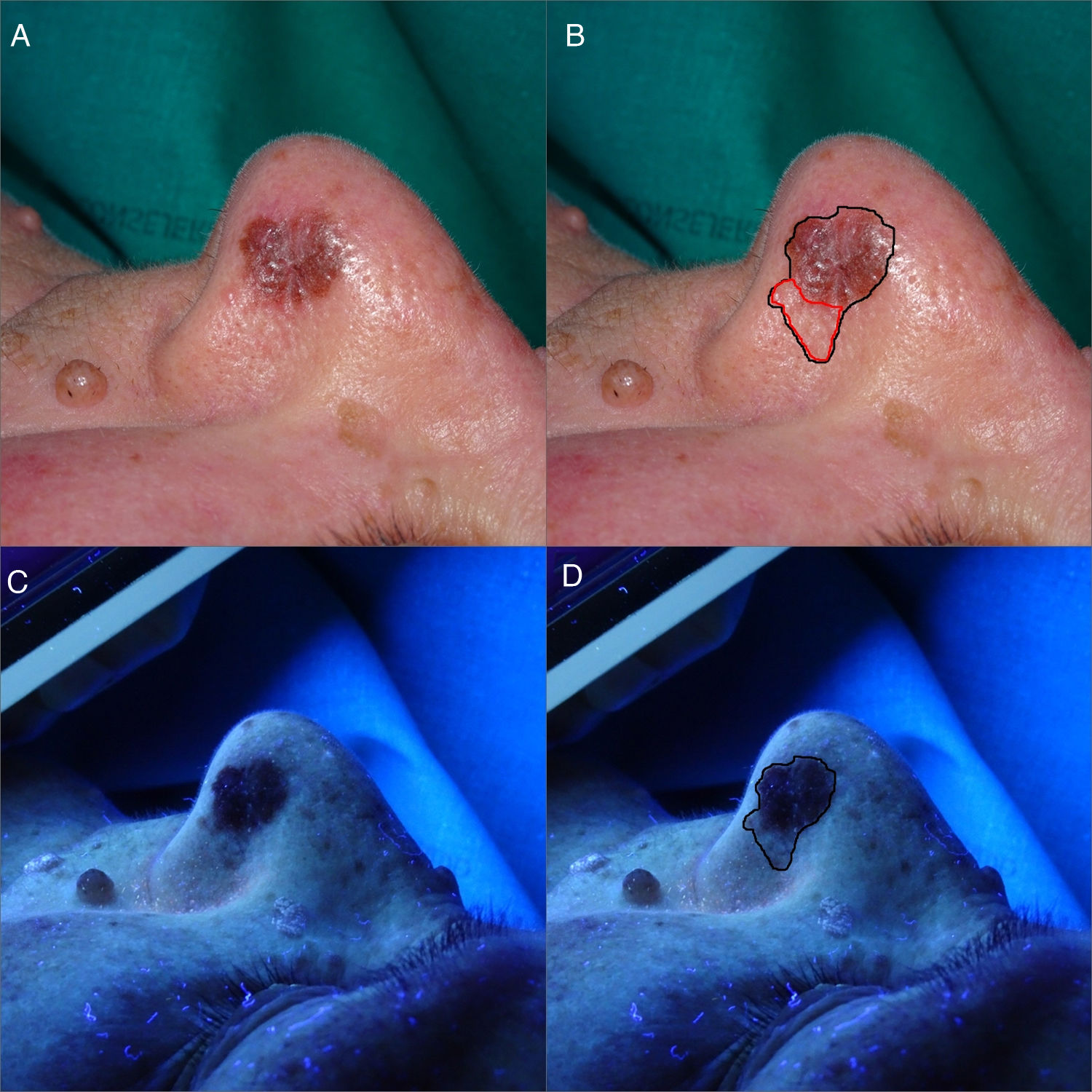
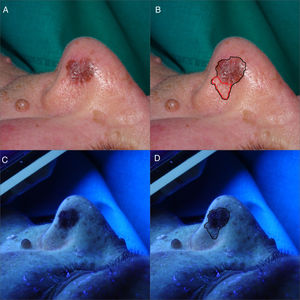
Case 1A 72-year-old woman was assessed for a pigmented lesion on the left nostril; the lesion had appeared years earlier and was growing progressively (Fig. 1). An incision biopsy was performed and LM was confirmed. It was decided to excise the lesion using Mohs micrographic surgery with delayed closure. Wood's light was used to delineate the lesion and revealed a pigmented region not visible clinically. The final measurements of the section were 25mm×18mm. Diagnosis was LMM with a Breslow thickness of 0.8mm, sparing the resection margins.
(A and B) Clinical images of LMM on the left nostril. Brownish macule measuring 10mm×10mm with a thick pigmented pseudoreticulum. In red, the clinically nonvisible pigmented area. (C and D) After illumination using Wood's light, the clinically nonvisible pigmented area can be seen. In black, the definitive surgical margin of 25mm×18mm.
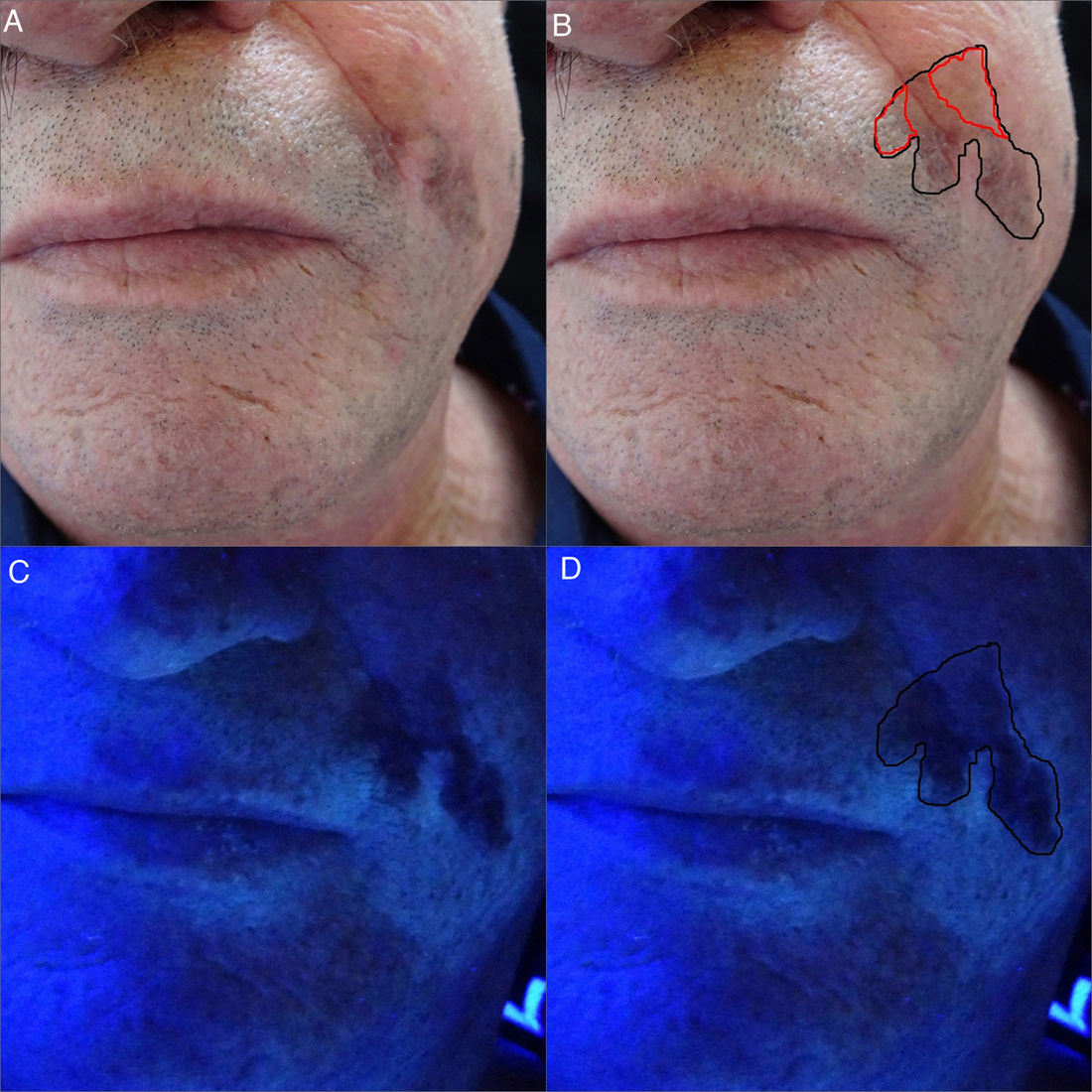
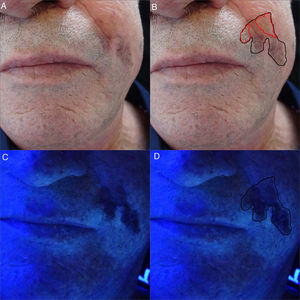
A 57-year-old man presented with a heterogeneous pigmented lesion measuring 2cm that had been growing progressively on the left nasolabial fold (Fig. 2). An incision biopsy was performed and confirmed LM. The patient was operated on using Mohs surgery with delayed closure following delineation of the lesion using Wood's light. The final measurements were 4.5mm×3cm. The diagnosis was LM with spared margin.
(A and B) Clinical images of LM in the left nasolabial fold. Poorly delineated hyperpigmented macule measuring approximately 2cm. In red, the clinically nonvisible pigmented area. (C and D) After illumination using Wood's light, the clinically nonvisible pigmented area can be seen. In black, the definitive surgical margin of 45mm×30mm.
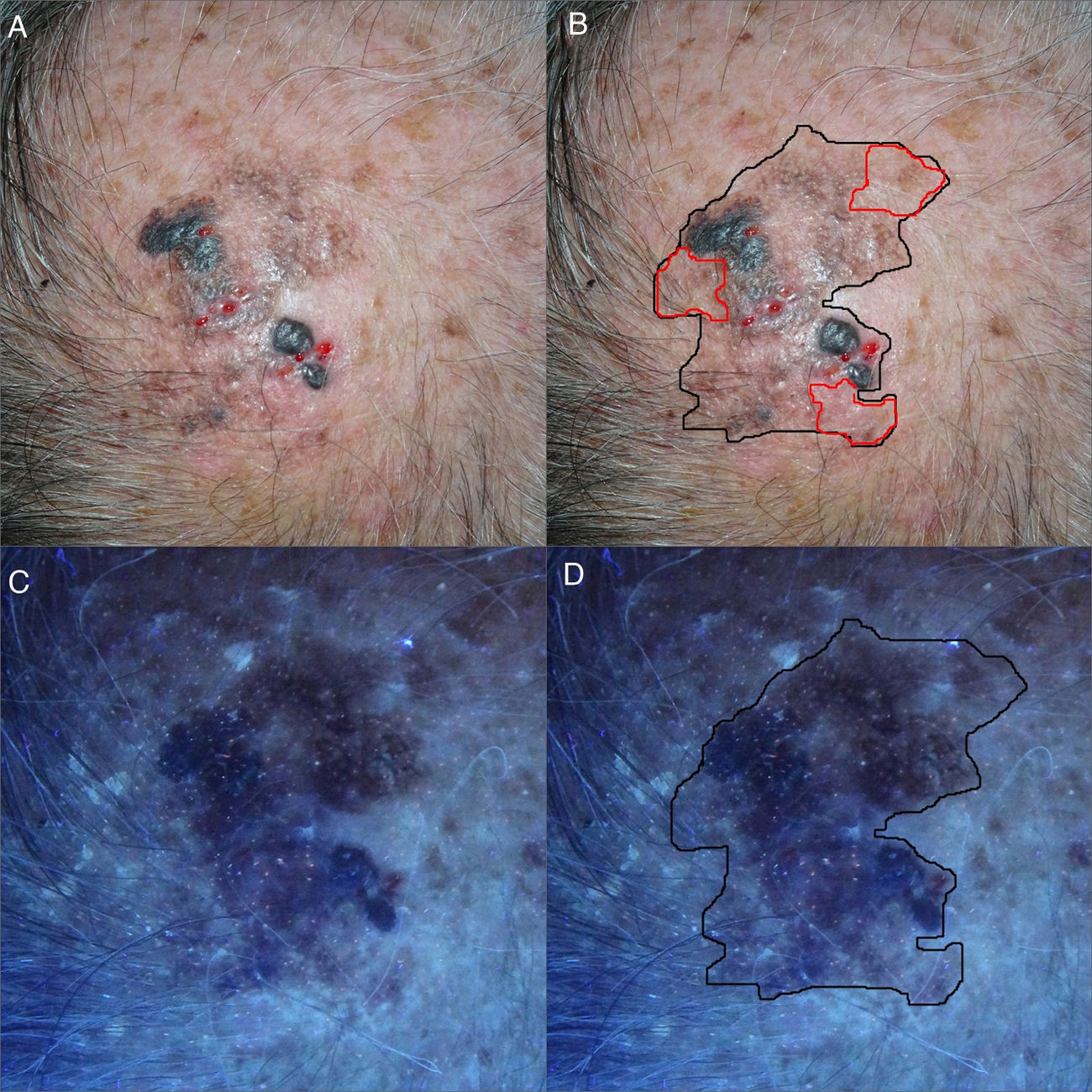
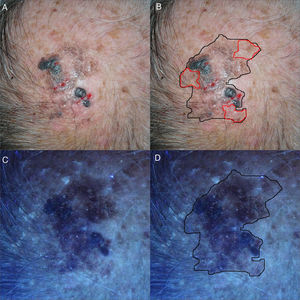
A 72-year-old man presented with a pigmented lesion on the scalp that had appeared 7 years earlier; the lesion had bled and had changed color (Fig. 3). Given the suspicion of malignant disease, several incision biopsies were performed and all of them confirmed LMM. The Wood's light made it possible to correctly delineate the lesion before surgery, with a final measurement of 3.5mm×4.5cm. The patient was operated on using Mohs surgery with delayed closure and the final diagnosis was LMM with a Breslow thickness of 3mm and a free margin.
(A and B) Clinical images of LMM on the cranial apex. Heterogeneous, poorly delineated hyperpigmented mark on the cranial apex measuring approximately 3cm. In red, the clinically nonvisible pigmented area. (C and D) After illumination using Wood's light, the previously nonvisible pigmented area can be seen. In black, the definitive surgical margin of 45mm×35mm.
Surgical treatment of LM and LMM is a therapeutic challenge because the microscopic margins are often affected or do not meet the recommended safety margin.2,3 Assessment of the margins prior to surgery for LM/LMM can be complex due to poor delineation of the lesion or lack of evident clinical pigmentation in some areas, and the use of techniques that facilitate correct delineation of the surgical margins is useful.
Wood's light is a useful though little-known tool for delineating the margins of LM or LMM, as it can reveal pigmented areas not visible to the naked eye or under normal light.4,5 Wood's light highlights the areas with a higher concentration of melanin, which appear darker in comparison to the healthy skin. Visible light may be insufficient for detecting the presence of melanin, due to its tendency to absorb radiation in the electromagnetic spectrum (350–1200nm), especially in short-wavelength frequencies.6
Another technique that has been shown to be of use in delineating pigmented lesions prior to surgery is reflectance confocal microscopy. However, its high cost, the learning curve required before using it, and the fact that it is not available in all clinics makes it less accessible than Wood's light in most cases.7
In our series, a physical and dermoscopic examination of the pigmented lesion was performed first, together with a subsequent examination using Wood's light. The border determined by the clinical and dermoscopic examination was smaller than that determined after using Wood's light in all cases. Although we have not assessed the difference in areas, and given the limitations of such a small series, all our patients required a single pass of Mohs surgery with delayed closure. In a recent series of LM treated with delayed Mohs, in which delineation of the lesions was performed clinically, the patients required between 1 and 4 passes to obtain a tumor-free surgical margin.8 Furthermore, in our patients LM or LMM in the areas highlighted by the use of Wood's light was confirmed by means of histology.
We propose the use of Wood's light to assess the surgical margins of LM and LMM before surgery in these patients, as it is an easy-to-use and accessible tool.
Conflicts of interestThe authors declare that they have no conflicts of interest.