Tunneled island flaps that transfer skin from a site adjacent to the wound are an effective way to reconstruct defects. These flaps provide good aesthetic and functional results and can be completed during a single surgical session, thus reducing complications. The procedure consists of taking an island of skin about the size of the surgical defect and moving it through a subcutaneous tunnel to cover the wound. We aimed to exemplify the use of these flaps in different regions of the face.
Material and methodsRetrospective descriptive study of 12 cases in which tunneled island flaps were used after removal of malignant tumors in different facial regions.
ResultsThe tumors, all of which were basal cell carcinomas, were removed by means of conventional surgery from 9 patients and Mohs micrographic surgery from 3 patients. Histology demonstrated tumor-free margins after excision in all cases. None of the tumors recurred during a mean follow-up period of 25 months. All complications were minor and transient. There were 3 cases of trapdoor effect and 2 each of postsurgical bleeding, transient superficial flap necrosis, and slight protrusion of the pedicle. The final cosmetic and functional outcome was satisfactory in all cases.
ConclusionsTunneled island flaps are particularly useful for repairing defects in the center of the face, where several anatomical structures converge. These flaps, which use donor skin that is similar to skin in the receptor site, can be used to close large defects in one-step procedures with only slight alteration of the facial architecture.
El colgajo en isla tunelizado (CIT) supone una opción eficaz para la reparación de grandes defectos faciales trasponiendo piel desde una unidad anatómica adyacente. La realización del colgajo aporta buenos resultados estéticos y funcionales en un único tiempo quirúrgico, evitando así complicaciones. El procedimiento consiste en labrar una isla de piel de dimensiones similares a las del defecto original, para luego desplazarla a través de un túnel subcutáneo a la región receptora. Nuestro objetivo es ejemplificar su uso en diferentes regiones de la cara.
Material y métodosEstudio descriptivo retrospectivo de 12 casos con reconstrucción mediante CIT tras la extirpación de tumores malignos en distintas áreas faciales.
ResultadosPresentamos una serie de 12 casos intervenidos de carcinoma basocelular, 9 mediante cirugía convencional y 3 mediante cirugía de Mohs. El estudio histológico mostró bordes quirúrgicos libres en todas las piezas de resección. El tiempo medio de seguimiento fue de 25 meses sin detectarse recidivas tumorales. Las complicaciones fueron menores y temporales: efecto trampilla en 3 pacientes, hemorragia posquirúrgica en 2, necrosis superficial transitoria del colgajo en 2 y protrusión leve del pedículo en 2 casos. El resultado final cosmético y funcional fue satisfactorio en todos los casos.
ConclusionesLos CIT son especialmente útiles en defectos centrofaciales donde convergen distintas unidades anatómicas. Permiten la reconstrucción en un único tiempo quirúrgico de grandes defectos faciales, aportando piel de características similares a las de la zona receptora y alterando mínimamente la arquitectura facial.
Reconstruction of large defects after excision of skin tumors is sometimes a challenge for dermatologists. Although a range of flap techniques and grafts are available, aspects such as site, size, or skin characteristics mean that the available options are not always sufficient for satisfactory repair. The mobility and function of different anatomical regions or the depth of the defect are other characteristics to take account when choosing reconstructive surgery.1
Tunneled island flaps are an effective alternative for repair of large defects in which different facial anatomical structures converge, particularly in the midfacial region. Good esthetic and functional outcomes can be achieved with flaps in a single surgical session. The technique consists of creating an island of skin of similar size to the original defect, and cutting a pedicle to enable transfer of the flap through a subcutaneous tunnel to the recipient region.2,3 We present our experience and outcomes after using tunneled island flaps in different facial regions. Our aim is to illustrate the versatility of the technique, reviewing cases in which the procedure was used at different anatomical sites and demonstrating that it is another option in the dermatologic surgeon’s arsenal.
Material and MethodsThis was a descriptive, retrospective study of 12 patients who had undergone reconstruction with tunneled island flaps after excision of malignant facial tumors. The patients were treated in the dermatology department of the Hospital General Universitario, Ciudad Real, Spain. The medical history of the patients (age and sex, cardiovascular risk factors, and concomitant medication), tumor and surgical characteristics (duration of the tumor, site, tumor size, type of surgery, resection margin, size of the surgical defect, and histopathological diagnosis), and events during follow-up (recurrence and short- and long-term postoperative complications) were reported. In all cases, the malignant skin tumors were removed under local tumescent anesthesia with or without sedation in a conventional surgical procedure or by Mohs surgery.
Flap TechniquesThe procedure begins by marking the resection border of the tumor, ensuring a suitable surgical margin. In patients who have undergone Mohs surgery, the piece is marked for subsequent fresh-tissue histology. Once the lesion has been excised, the tunneled island flap procedure begins:
- 1.
Design of the island: We select the donor surface by marking an island of skin of similar shape and size to the original defect. This area will be close, but not immediately adjacent, to the original defect. An area of skin is left where the subcutaneous tunnel will subsequently be made. It can be helpful to imagine the pedicle as a pendulum of sufficient length to allow rotation of the island to the defect.
- 2.
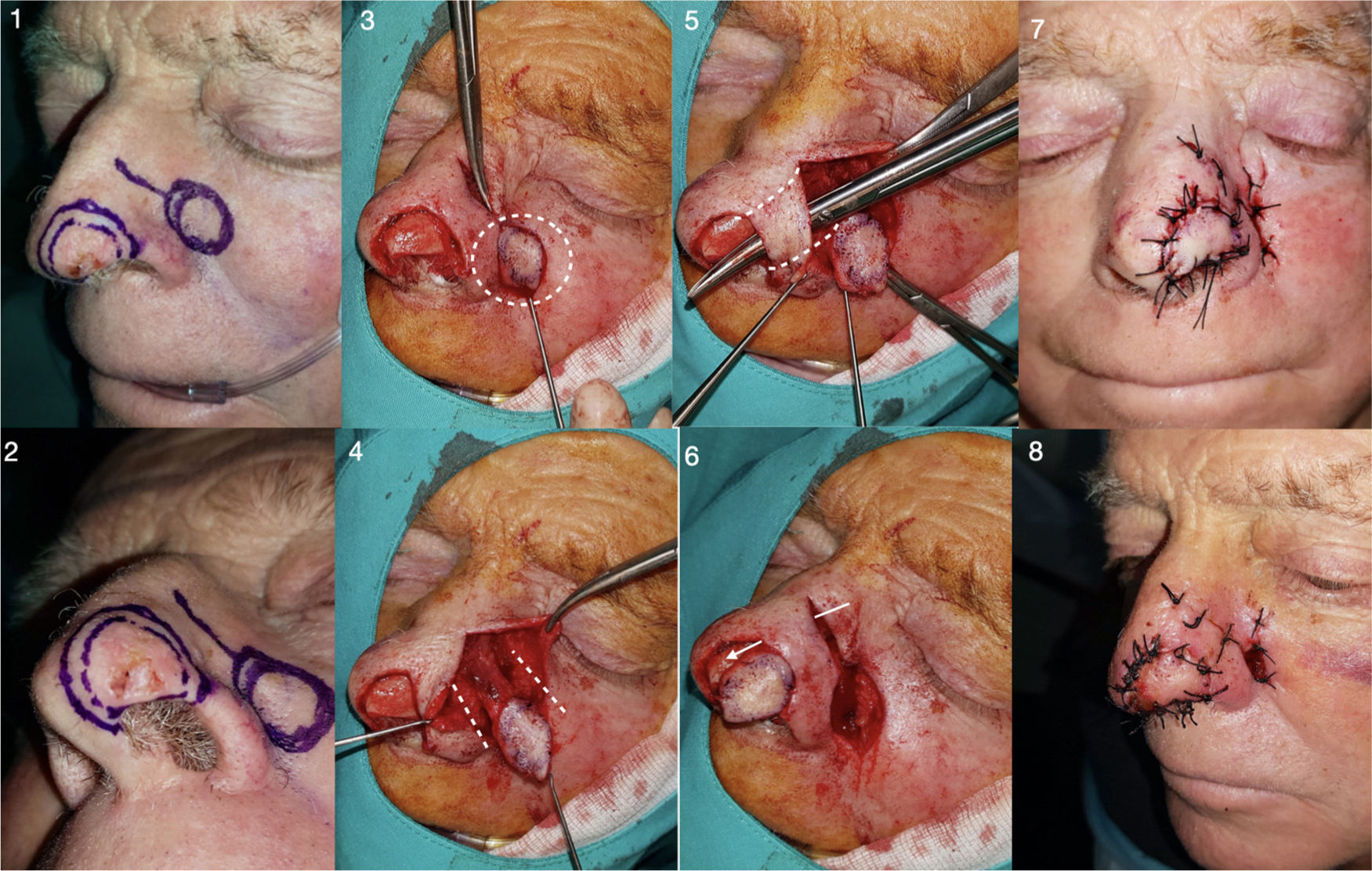
Elaboration of the pedicle: The pedicle can be subdermal or include skin that will subsequently be deepithelialized. This choice will not substantially impact the outcome, although each surgeon will have his or her preferences. In our opinion, the option of performing a cutaneous incision that is subsequently deepithelialized at the point where it passes through the tunnel is probably somewhat more laborious and time-consuming than subdermal incision. The island is cut in the donor area using a full-thickness vertical incision. We start to dissect the subcutaneous pedicle, conserving the area underlying the island, including all subcutaneous tissue and often the underlying muscle as well in the central area. The pedicle should have 2 essential characteristics: be thick enough with sufficient vascularization to avoid distress (10-20 mm wide) and long enough to transfer the island of skin to the original defect without excessive tension. If we move the flap with forceps, we can check that it is of sufficient length. Of note, flap vascularization is random in most cases (Fig. 1), although an arterial flap can be created under Doppler skin ultrasound guidance. In our series, there were 3 cases of paramedian forehead arterial flaps. The procedure involves using ultrasound to locate the corresponding artery, in this case, the supratrochlear artery, which originates from the ophthalmic artery and runs vertically in the paramedian region (approximately 2 cm from the medial line of the forehead) over the frontalis muscle (Fig. 2). When elaborating this pedicle, it is important to remember that the supratrochlear artery descends in its most proximal part between the orbicularis oculi and corrugator supercilii muscle, reaching the periosteal plane, and so the dissection should reach down to this anatomical plane.
Figure 1.Design, realization, and immediate postoperative outcome of a paranasal tunneled island flap with random vascularization (Patient 5). 1 and 2. Delimitation with 3-4 mm tumor margins (BCC) and design of the ipsilateral island. 3 and 4. Elaboration of the island of skin and dissection of the subcutaneous pedicle. 5 and 6. After obtaining a pedicle of sufficient length, the tissue between the donor and recipient area is tunneled, and the flap is passed through the tunnel, ensuring that the flap reaches the recipient area without excessive tension. 7 and 8. Direct closure of both areas, in this case with braided silk 4/0 thread.
Figure 2.Design, realization, and postoperative outcome of a paramedian forehead tunneled island flap with arterial pedicle (supratrochlear artery) (Patient 2). 1. After BCC resection from the tip of the nose with Mohs surgery, the supratrochlear artery with greatest flow is located using Doppler mode ultrasound (in this case, the left artery) and a paramedian forehead tunneled island flap is designed. 2-4. Cutting out the island and epithelized pedicle, checking that it is long enough to reach the recipient area. 5. Tunneling the area of skin between the recipient and donor areas. 6. Deepithelization of the pedicle to subsequently pass it through the tunnel. 7. Direct closure of both areas. 8. Partial distal necrosis of the flap on the third day after the operation (patient was a heavy smoker). 9. Outcome 1 year after the procedure.
- 3.
Tunnel creation and flap transposition: To open a tunnel in the area of skin between the island and the original defect, we lift up the subcutaneous plane with the help of forceps and blunt-tipped dissecting scissors to create a subcutaneous cavity of sufficient width for the flap to pass through. Once the tunnel is formed, we pass the flap through it pulling with the forceps to then place it in the recipient area. As mentioned earlier, we should ensure that the pedicle is not unduly twisted, stretched or compressed when passing through the tunnel, as this could cause distal distress or even necrosis. The flap is attached to the recipient area with simple nonabsorbable stitches. Direct closure of the donor area is performed using the same suture.
The transcartilage variant of the tunnel island flap is useful in the auricular region.3,4 The flap can be derived from the preauricular region5 or retroauricular one.4 A flap derived from this latter location is known as the flip-flop flap or revolving door island flap, and has certain peculiarities derived from the anatomy of the region. After delimiting the defect to be excised on the anterior face of the auricle, we design the flap in the retroauricular region. The island includes skin from the mastoids and skin from the posterior face of the ear, leaving the middle area centered on the retroauricular groove. To design this flap more precisely, we can pass a needle through the edges of the original defect, from an anterior to posterior direction, and thus mark the edges of the flap. Once the original defect has been cut out (with or without underlying cartilage) and the island and myocutaneous pedicle have been formed, we cut a hole in the auricular cartilage to form a tunnel and pass the flap to the anterior region, attaching it with simple stitching. Direct closure is performed in the retroauricular area of the donor site (Fig. 3).
Design, realization, and immediate and late postoperative outcomes of retroauricular tunneled island flap or revolving door flap (Patient 12). 1 and 2. Design and resection with 3-4 mm margins of BCC in antihelix, exposure of the underlying cartilage. 3 and 4. Elaboration of the retroauricular island of skin. 5 and 6. Tunneling towards the anterior auricular area through cartilage and transposition of the retroauricular island of skin towards the anterior auricular area. 7 and 8. Direct closure of both areas, immediate postoperative outcome and after 5 months.
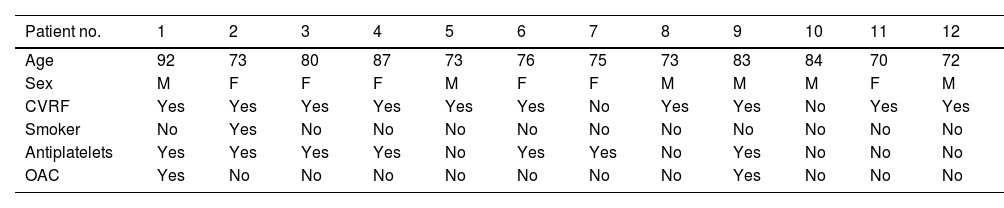
In total, 12 patients were included in the series, 6 men (50%) and 6 women (50%), with ages ranging from 70 to 90 years, and a mean age of 78 years. With regards personal history: 10 (83.3%) had hypertension, 2 (16.6%) had diabetes mellitus, 1 (8.3%) was a current smoker, and 4 (33.3%) had cardiovascular disease (ischemic heart disease, atrial fibrillation, stroke, and peripheral artery disease). Seven (58.3%) were receiving antiplatelet therapy (acetylsalicylic acid, clopidogrel, or both) that was maintained and 2 (16.6%) were receiving blood thinners (acenocoumarol) which was suspended prior to surgery (Table 1).
Personal History.
| Patient no. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 92 | 73 | 80 | 87 | 73 | 76 | 75 | 73 | 83 | 84 | 70 | 72 |
| Sex | M | F | F | F | M | F | F | M | M | M | F | M |
| CVRF | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes |
| Smoker | No | Yes | No | No | No | No | No | No | No | No | No | No |
| Antiplatelets | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | No | No | No |
| OAC | Yes | No | No | No | No | No | No | No | Yes | No | No | No |
Abbreviations: CVRF, cardiovascular risk factors; F, female; M, male; OAC, oral anticoagulant.
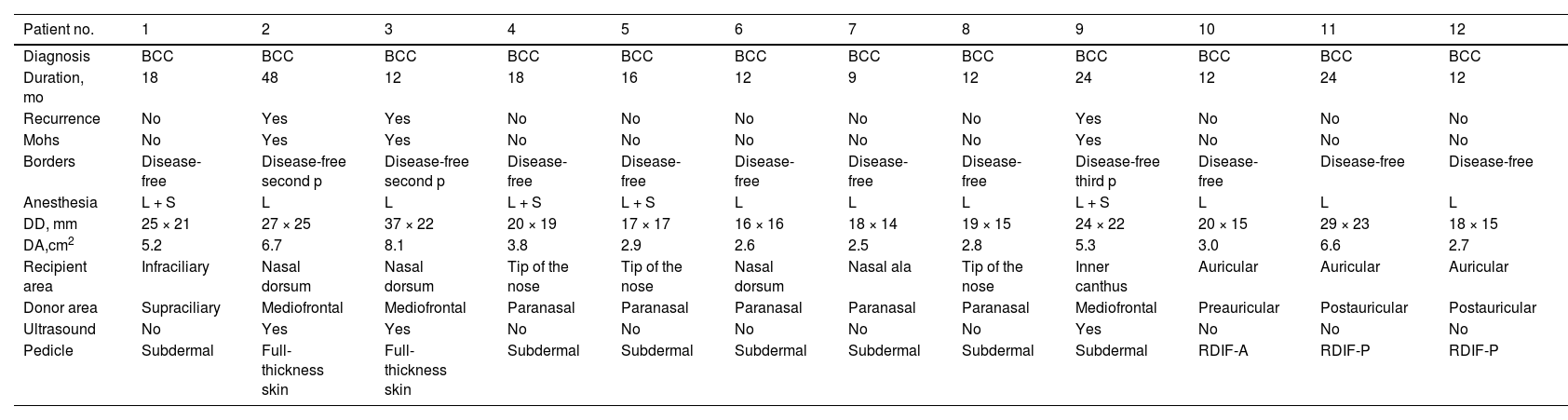
The excised lesion was basal cell carcinoma (BCC) in all cases, with a mean duration of 18 months (range, 9 to 48 months). Nine (75%) of the patients underwent conventional surgery and 3 (25%) underwent Mohs surgery as a recurrence of a previous BCC lesion was being removed, with disease-free borders achieved in the second pass (2 patients) or third pass (1 patient). All patients underwent the intervention under local tumescent anesthesia. Four patients also underwent sedation. Histologic study showed disease-free borders in all patients (100%). The long-axis of the defect ranged from 16 to 37 mm, with a mean of 22.5 mm, and an area between 2.5 and 8.1 cm2, with a mean of 4.4 cm2. The site of the defect was nasal in 7 patients (58.3%) (dorsum, tip and nasal ala), periorbital in 2 (16.6%) (subciliary and inner canthus), and auricular in 3 (25%) (triangular fossa, tragus, and the concha). The flaps were obtained from the frontal region (paramedian forehead, supraciliary) in 4 of the patients (33.3%), the paranasal region or nasolabial groove in 5 (41.6%), and the auricular region (preauricular, postauricular) in 3 (25%). With regards the flap characteristics, 9 patients (75%) had random vascularization and 3 (25%) ultrasound-located arterial pedicle. The pedicle was subdermal in 7 patients (58.3%), full thickness (subsequently deepithelialized) in 1 patient (16.6%), and auricular revolving door format in 3 patients (25%) (Table 2).
Surgical Characteristics: Tumor Type, Type of Surgery, Defect Size, Surgical Borders, and Type of Flap.
| Patient no. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diagnosis | BCC | BCC | BCC | BCC | BCC | BCC | BCC | BCC | BCC | BCC | BCC | BCC |
| Duration, mo | 18 | 48 | 12 | 18 | 16 | 12 | 9 | 12 | 24 | 12 | 24 | 12 |
| Recurrence | No | Yes | Yes | No | No | No | No | No | Yes | No | No | No |
| Mohs | No | Yes | Yes | No | No | No | No | No | Yes | No | No | No |
| Borders | Disease-free | Disease-free second p | Disease-free second p | Disease-free | Disease-free | Disease-free | Disease-free | Disease-free | Disease-free third p | Disease-free | Disease-free | Disease-free |
| Anesthesia | L + S | L | L | L + S | L + S | L | L | L | L + S | L | L | L |
| DD, mm | 25 × 21 | 27 × 25 | 37 × 22 | 20 × 19 | 17 × 17 | 16 × 16 | 18 × 14 | 19 × 15 | 24 × 22 | 20 × 15 | 29 × 23 | 18 × 15 |
| DA,cm2 | 5.2 | 6.7 | 8.1 | 3.8 | 2.9 | 2.6 | 2.5 | 2.8 | 5.3 | 3.0 | 6.6 | 2.7 |
| Recipient area | Infraciliary | Nasal dorsum | Nasal dorsum | Tip of the nose | Tip of the nose | Nasal dorsum | Nasal ala | Tip of the nose | Inner canthus | Auricular | Auricular | Auricular |
| Donor area | Supraciliary | Mediofrontal | Mediofrontal | Paranasal | Paranasal | Paranasal | Paranasal | Paranasal | Mediofrontal | Preauricular | Postauricular | Postauricular |
| Ultrasound | No | Yes | Yes | No | No | No | No | No | Yes | No | No | No |
| Pedicle | Subdermal | Full-thickness skin | Full-thickness skin | Subdermal | Subdermal | Subdermal | Subdermal | Subdermal | Subdermal | RDIF-A | RDIF-P | RDIF-P |
Abbreviations: A, anterior; BCC, basal cell carcinoma; DD, defect diameter; L, local; p, Mohs pass; P, posterior; RDIF, revolving-door island flap; S, sedation.
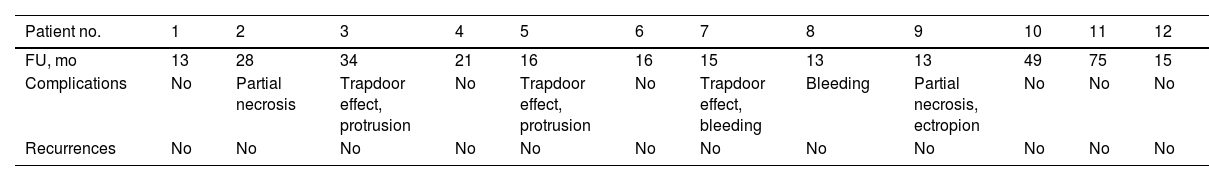
Mean postoperative follow-up was 25 months (between 13 and 75 months), with no recurrences detected to date. The complications were minor and temporary. These included trapdoor effect in 3 patients (25%), postoperative bleeding in 2 (16.6%), transient surface necrosis of the flap in 2 (16.6%), and protrusion of the pedicle in 2 (16.6%). Of the patients with a trapdoor effect, the complication resolved spontaneously in 1 patient in the months after the intervention (Patient 3). In the other 2 patients, the trapdoor effect improved but did not completely resolve (Patients 5 and 7), and the patients were offered the possibility of a surgical correction, which they declined. In the 2 patients who experienced distal necrosis of the flap, the complication resolved satisfactorily with surface debridement after surgery. In addition, successful correction was achieved in a second session in a patient who developed postoperative ectropion. The final cosmetic and functional outcomes (Likert scale) for the physician and patient was considered as good or very good in all cases (Table 3).
Postoperative Characteristics.
| Patient no. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FU, mo | 13 | 28 | 34 | 21 | 16 | 16 | 15 | 13 | 13 | 49 | 75 | 15 |
| Complications | No | Partial necrosis | Trapdoor effect, protrusion | No | Trapdoor effect, protrusion | No | Trapdoor effect, bleeding | Bleeding | Partial necrosis, ectropion | No | No | No |
| Recurrences | No | No | No | No | No | No | No | No | No | No | No | No |
Abbreviation: FU, follow-up.
Reconstruction of facial skin defects, without altering the face's natural structure, is a surgical challenge. Conventional flaps or full-thickness skin grafts are not always appropriate for repairing certain defects. Tunneled island flaps are a variant of conventional island flaps and they have been used both in facial and body skin defects, for repair of surgical and traumatic defects, and even burns.6,7 The interest in this type of flap seems to have grown in recent years, although there have been reports of the technique dating from the 1990s. They were initially described for the reconstruction of skin defects at sites such as the inner canthus8 or the nasal dorsum or ala.9 They are, however, more versatile as our series shows and as will be described.
In the classic advancement island flap, the pedicle is short with more tension and limited mobility, although sufficient to cover close, contiguous defects. With tunneled island flaps, a longer pedicle is cut with greater mobility, allowing transfer of donor skin from a distant, noncontiguous region of an adjacent anatomical unit.3 This is something common in the midfacial area where different anatomical units converge, and this is why the technique is useful for facial defects. After positioning the flap, the tunnel is cut passing through the border between the 2 units, which would be the glabella in frontonasal ones, the conchal cartilage in auricular ones, or the nasogenian groove in the paranasal ones. The skin at this border is not cut and its position is not altered, and so facial symmetry is perfectly conserved.2 The interpolated flap is identical, with the same advantages, but in this case, the pedicle is left at this border for several days, and it has to be excised in a second session.
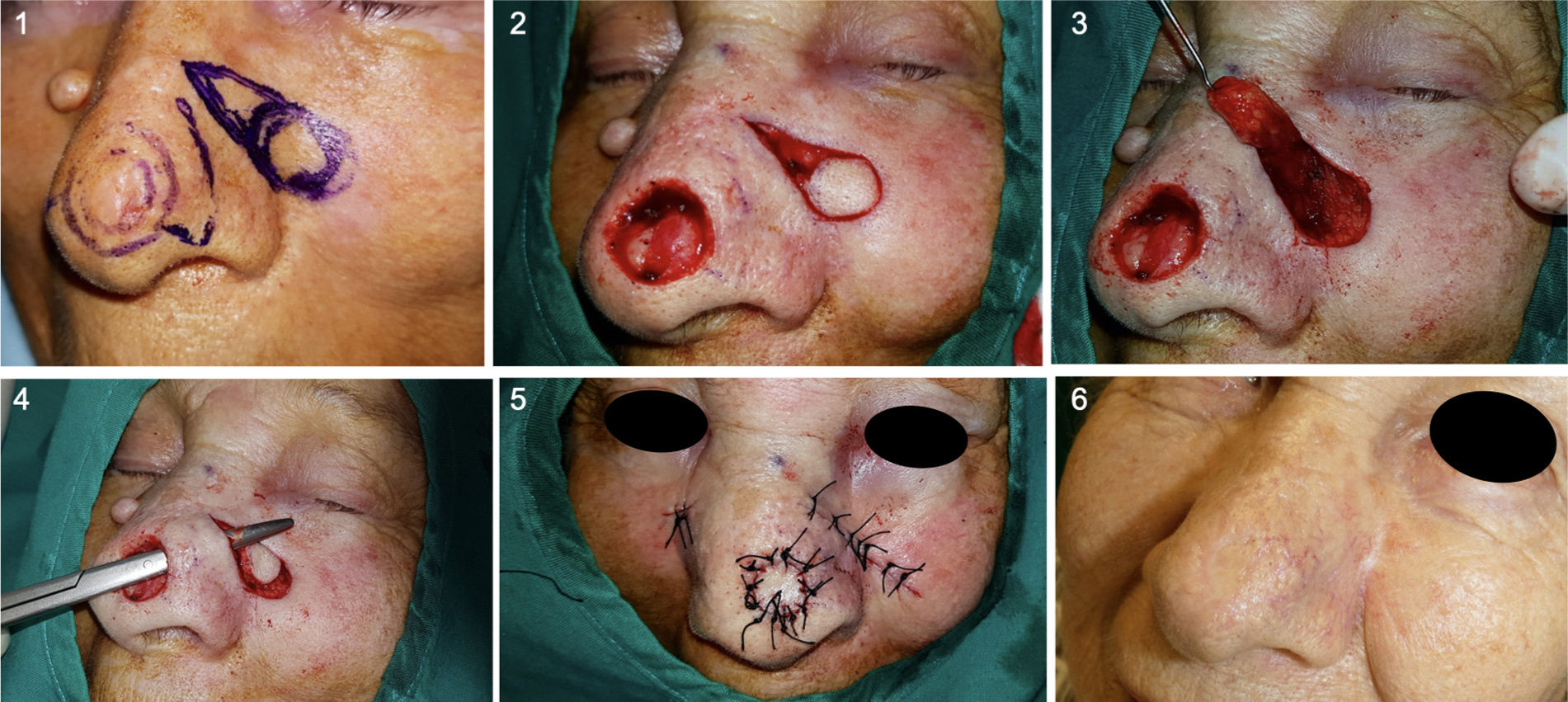
Paranasal tunneled island flaps are useful for repairing defects on the nasal tip, dorsum, or ala, transposing skin from the cheek. This allows the original defect to be repaired with skin of similar thickness and characteristics (Fig. 4). The nasal ala effectively retains the curvature and positioning of the ala and nasolabial groove. Defects that involve the free alar border can also be repaired with this technique.10 Given the reduced postoperative ala retraction, which helps maintain the outline, concavity, and position of the groove, and the possibility of hiding the pedicle scar in the nasogenian groove itself, this is an ideal technique that provides excellent esthetic and functional outcomes.11–13 In the classic flap of the nasogenian groove, the same skin from the cheek is transposed to the nose, often changing the position of the groove and its attachment to deep layers. Deep anchoring sutures are therefore needed to keep the groove in position and prevent tenting. This is not an issue with paranasal tunneled island flaps.
Left paranasal tunneled island flap to repair surgical defect on the tip of the nose (Case 4). 1. Design and resection of BCC with 4 mm margins and design of the flap. 2 and 3. Elaboration of the subcutaneous pedicle until achieving sufficient length to reach the recipient area. 4. Tunneling of the area between the 2 regions to subsequently pass the flap through the tunnel. 5. Direct closure of both areas. 6. Outcome 5 months after surgery.
Paramedial forehead tunneled island flaps are useful for repair of large defects on the nasal dorsum or tip, where repair with conventional flaps or grafts does not always yield good outcomes. The anatomy of the nose or the depth of the defect to be repaired may hinder this task. These tunneled island flaps allow large defects to be repaired in a single surgical procedure, unlike other variants that require more than one session.14 Although this is one of the most laborious flap procedures to perform, the esthetic and functional outcomes are satisfactory. Random vascularization is a valid option, especially if the flap’s length does not exceed 3 times its width.15 In our case, we demonstrate the usefulness of Doppler ultrasound in 3 cases of paramedian forehead tunneled island flaps. An arteriovenous flap was obtained irrigated by the supratrochlear artery, a branch of the ophthalmic artery, that lies at approximately 2 cm from the paramedian forehead line, reaching the periosteal plane at the level of the orbicularis and corrugator supercilii muscles. This type of vascularization ensures effective blood supply to the flap.16
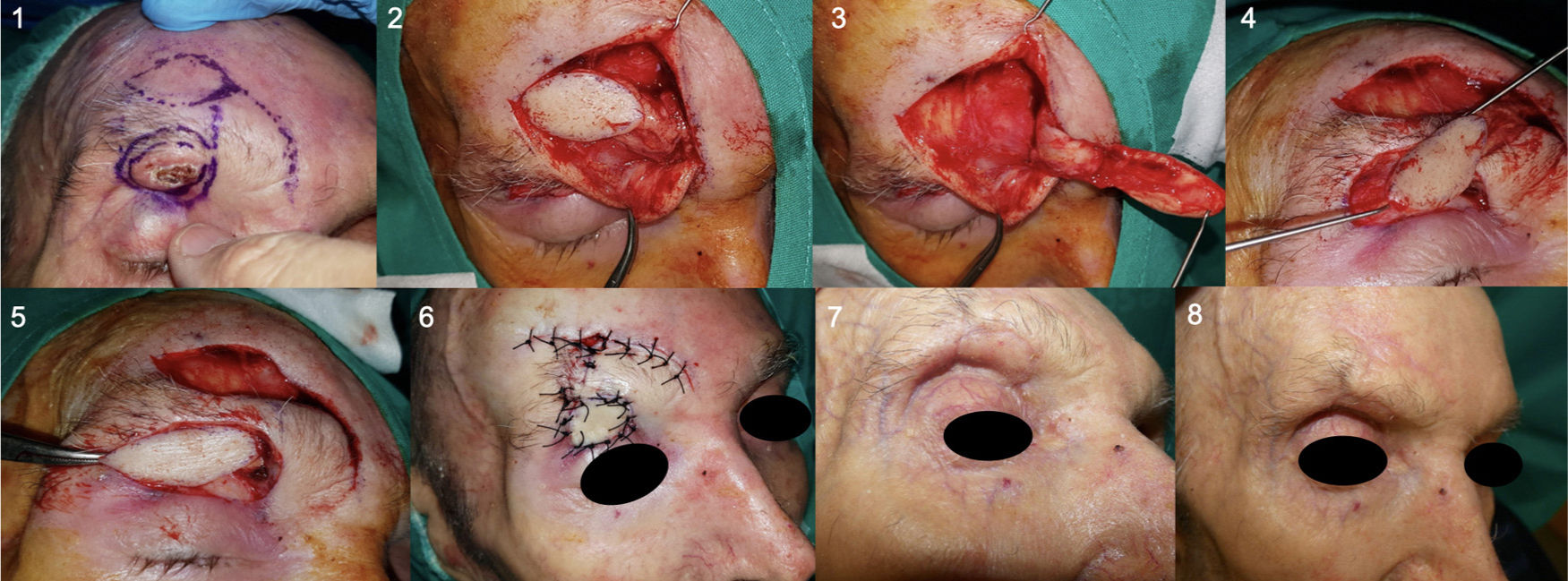
In one of our patients, a contralateral paramedian forehead tunneled island flap was performed to repair a substantial defect at the level of the left inner canthus (Fig. 5). At this site, care is required to avoid impacting palpebral structure and function. Postoperative ectropion developed in this patient, as expected by the need for full thickness resection at the inner corner of the eye, and this required a second session procedure with an excellent final outcome.
Mohs surgery to resect BCC on the left inner canthus (Patient 9). 1 and 2. Delimitation of the margins for Mohs surgery and defect after 3 Mohs passes. 3. Design of paramedian forehead contralateral tunneled island flap with arteriovenous pedicle guided by Doppler ultrasound. 4-6. The posterior lamella is reconstructed with a split graft from the contralateral upper eyelid tarsus. 7-10. Subsequently, the island of skin is cut, dissecting the subcutaneous pedicle and tunneling the glabellar area. The flap is passed through the tunnel and direct closure performed in both areas. 11 and 12. Postoperative outcomes with ectropion of the lower eyelid after 3 months, and after repair in a second session.
Laterofrontal and supraciliary tunneled island flaps are a useful option for repairing large periocular defects. It is a valid alternative both for the inner canthus and the infraciliary region, as shown in the case presented (Fig. 6), with the eyebrow and periocular anatomy preserved.
Supraciliary tunneled island flap to repair a subciliary defect (Patient 1). 1. Subciliary ulcerated BCC; the tumor is resected with 3 mm margins and an island flap designed in the supraciliary area. 2 and 3. Elaboration of the island of skin and dissection of the subcutaneous pedicle. 4 and 5. Tunneling of the area between the 2 defects to subsequently pass through the tunnel with collagen, bringing the island of skin to the original defect. 6, 7, and 8. Immediate postoperative outcome and after 3 months, preserving ciliary structure and functionality of the upper eyelid.
Auricular tunneled island flaps allow defects in the anterior face of the ear to be repaired. In defects close to the tragus or the earlobe, tunneled island flaps can be performed, taking donor skin from the preauricular area,5 as the subcutaneous fat in this region is useful for preserving the contour and thickness of the lobe.17 The retroauricular variant, known as the revolving door flap was initially described for repairing detects in the concha.18–20 This option allows closure of large defects in a single session using skin with characteristics similar to the retroauricular region.21,22 Although the technique was originally described for repair of conchal defects, the cases presented in this series and other series have shown good results in areas such as the antihelix, triangular fossa, and scaphoid fossa.4
Although flap design is not particularly difficult, the procedure requires a certain manual dexterity and experience in dermatologic surgery. After correctly measuring the original defect to mark out an appropriately sized island, the pedicle should be cut with sufficient thickness to avoid necrosis or distress, but not so wide or redundant that it is difficult to move and would protrude into the tunnel compressing the vessels. Whenever possible, it is preferable that the pedicle includes muscle to improve the chances of survival.23 Careful and delicate dissection of the pedicle is key to avoid complications. The length of the pedicle is assessed by pulling with forceps; it should be sufficiently long to reach the area of the original defect without excessive tension or torsion.12 As can be seen in the cases presented here, the esthetic and functional outcomes are excellent.
Complications arising from tunneled island flaps are for the most part minor and short-lived. The most common according to the literature are those often seen with other flaps: bleeding, wound infection, and partial necrosis of the flap. In 2 cases in our series (patients 2 and 9), partial necrosis of the distal area of the flap occurred; this resolved satisfactorily with surface debridement during postoperative dressing changes. Patient 2 was a smoker who continued to smoke in the postoperative period, and this may have been a major factor in the development of this complication. Of note is that in both cases necrosis was partial and involved the most distal and superficial area, and epithelization on the transposed collagen gave an excellent final outcome. Among the complications of tunneled island flaps, protrusion of the pedicle is particularly noteworthy, especially the trapdoor effect (Fig. 7). This complication is common in most island flaps,2,3 by causing closed triangular or circular scarring,24 which appears protruding from the surrounding surface. It has been attributed to several causes, including lymphatic obstruction, scar contraction, hypertrophy, excess subcutaneous thickness, and a beveled edge. However, avoiding an excessive flap thickness or making a vertical cut to avoid beveling do not always prevent the development of a trapdoor effect.24 It should be highlighted that an appropriate thickness is beneficial for repair in certain sites such as the tip of the nose, as it helps to restore the original form and volume in defects with exposed cartilage, commonly seen after nasal tumor resections. To minimize this complication, it is recommended to reduce the island area by 20% to 25%,6,11 undercut the edges of the surrounding skin25, and design a pedicle with as small a base as possible.26 During the postoperative period, massaging can be employed to improve lymphatic drainage12, and a wait of at least 3-6 months would seem advisable as many defects improve spontaneously6 as shown in Patient 3 (Fig. 7B). In persistent cases, use of intralesional corticoids or surgical repair (with Z-plasty or shaving) can be effective alternatives.12
Postoperative follow-up in 2 patients who developed the trapdoor effect. A. In Patient 5, the trapdoor effect and protrusion of the pedicle can be seen at the nasogenian fold at 2 months after surgery. In this case, surgical correction in a second procedure was not needed. B. In Case 3, a notable trapdoor effect can be observed at 2 months after surgery. Spontaneous improvement occurred as the months went by. Excellent esthetic outcome at 24 months after the operation.
In conclusion, we present this case series of tunneled island flaps, used to repair large skin defects. This technique is particularly useful in central facial areas, where different anatomic units converge. These flaps have the advantage of being able to repair defects whose depths mean that the use of free grafts would yield less satisfactory esthetic outcomes, for example those on the nasal ala or tip; flaps can provide necessary volume (dermis and subcutaneous tissue). The benefits derived from repair in a single session are also worthy of mention. This reduces surgical risk and use of anesthetics, as well as time in the operating room. Keeping the process to one session limits the inconvenience to the patient and avoids complications arising from a second operation. The versatility of the technique is without doubt one its is most noteworthy characteristics. Finally, tunneled island flaps show good esthetic and functional results, yielding skin with characteristics similar to those of the recipient area and with minimal impact on facial structure. Although the technique requires care and certain manual dexterity, if correctly applied, the complications arising from this type of flap are minor and self-limiting, with the most characteristic one being the trapdoor effect.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rogel-Vence M, Carmona-Rodríguez M, Moro-Bolado F, González-Ruiz L, Sánchez-Caminero MP, Romero-Aguilera G. Versatilidad del «colgajo en isla tunelizado» para la reconstrucción de defectos faciales. Actas Dermosifiliogr. 2022;113:123–133.