The development and progression of acne are conditioned by genetic, hormonal, and environmental factors. Hormonally, elevated androgen and growth hormone levels has been associated with acne exacerbations. Environmentally, it has been postulated that diets associated with a high glycemic index (GI), and the consumption of milk and chocolate, can exacerbate this condition1–3.
GI represents a score from 1 to 100 that expresses how quickly a carbohydrate is digested, absorbed, and metabolized2. Diets with a high GI have scores > 55. The Western diet is characterized by the consumption of dairy and high-glycemic foods.
Meixiong et al.2 conducted a systematic review evaluating the association of a high-GI diet and/or dairy intake with acne pathogenesis. They included a total of 34 articles (n=120,398): 28 were observational studies (42.9%, case-control studies; 14.3%, longitudinal cohort studies; and 42.9%, cross-sectional studies) and 6 were controlled clinical trials (5 were randomized and 1 non-randomized). A total of 77% of the 18 observational studies performed showed an association between high-GI diets and acne severity. Smith et al.3 randomized a total of 43 acne patients treated with facial cleanser to receive a low-GI diet (GI=43) or a control diet (GI=56) for 12 weeks. The low-GI diet group experienced better results than the control group: a decrease in the number of lesions -16 in the low-GI group vs –8.5 in the control group (p=0.04).
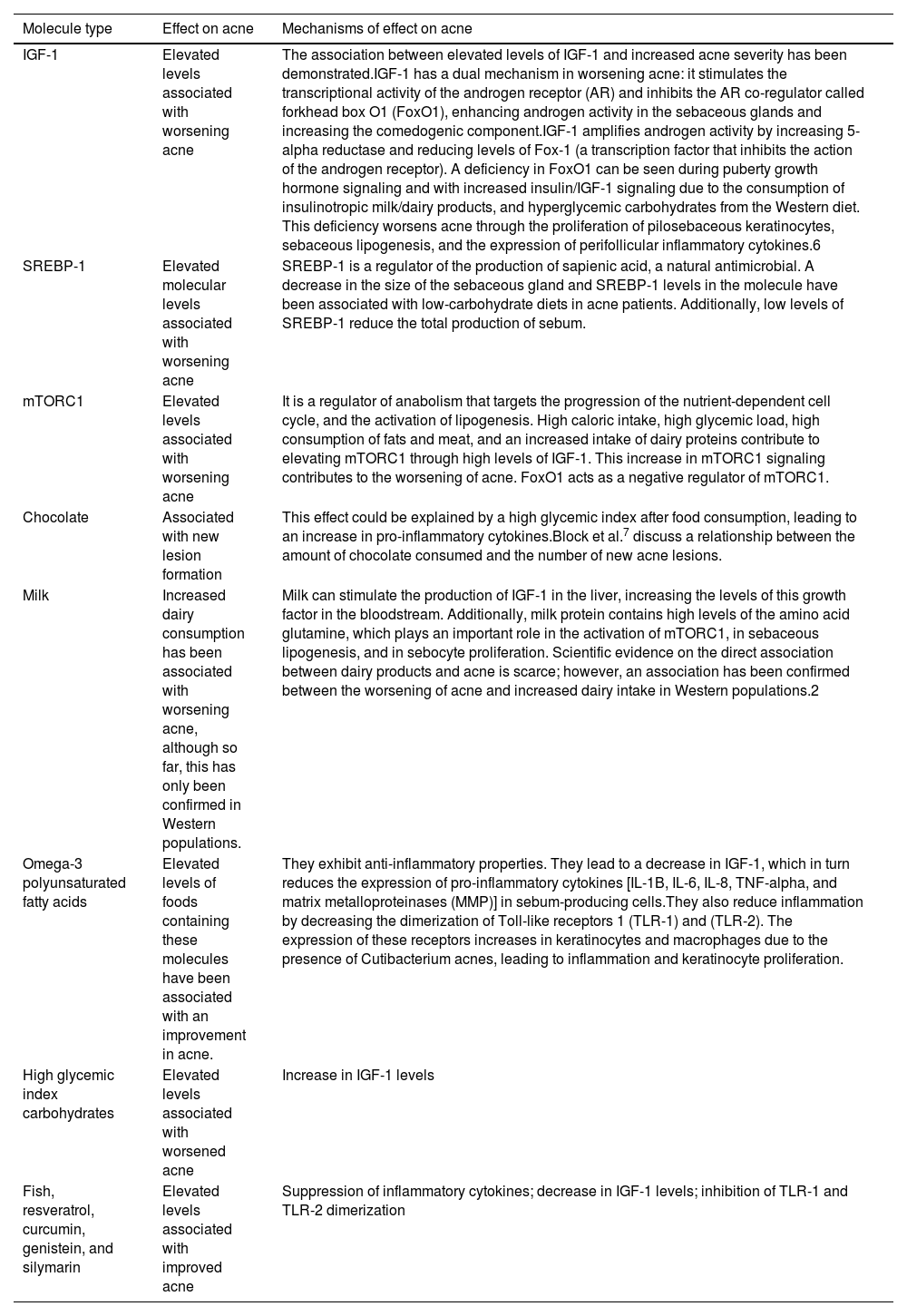
Conforti et al.1 conducted a review on foods that may be involved in acne pathogenesis and the pathophysiological explanation of the molecules involved (Table 1). High-GI diets are associated with hyperinsulinism, which leads to an increase in androgens, insulin-like growth factor 1 (IGF-1), and IGF-3, contributing to the development and worsening of acne1. Carbohydrate-rich diets are associated with hyperglycemia, reactive hyperinsulinemia, and elevated levels of IGF-1. However, a Mediterranean diet (MD), characterized by low-glycemic-load foods, minimal dairy intake, and an abundance of nutrients with antioxidant and anti-inflammatory properties such as fruits and vegetables, may decrease the signaling produced by IGF-1 and, consequently, acne4. These foods contain hydroxytyrosol, tyrosol, oleocanthal, and resveratrol, phenolic compounds with anti-inflammatory properties. Recently, Ah-Thiane et al.5 published a case-control study5 (n=80) to determine the relationship between acne severity in French women and adherence to the MD. In acne patients, a significant negative correlation was found between acne severity determined by the Global Evaluation Acne (GEA) scale and adherence to the MD, with a Spearman correlation coefficient of r=-0.47; p<0.001.
Role of foods and molecules associated with acne.
| Molecule type | Effect on acne | Mechanisms of effect on acne |
|---|---|---|
| IGF-1 | Elevated levels associated with worsening acne | The association between elevated levels of IGF-1 and increased acne severity has been demonstrated.IGF-1 has a dual mechanism in worsening acne: it stimulates the transcriptional activity of the androgen receptor (AR) and inhibits the AR co-regulator called forkhead box O1 (FoxO1), enhancing androgen activity in the sebaceous glands and increasing the comedogenic component.IGF-1 amplifies androgen activity by increasing 5-alpha reductase and reducing levels of Fox-1 (a transcription factor that inhibits the action of the androgen receptor). A deficiency in FoxO1 can be seen during puberty growth hormone signaling and with increased insulin/IGF-1 signaling due to the consumption of insulinotropic milk/dairy products, and hyperglycemic carbohydrates from the Western diet. This deficiency worsens acne through the proliferation of pilosebaceous keratinocytes, sebaceous lipogenesis, and the expression of perifollicular inflammatory cytokines.6 |
| SREBP-1 | Elevated molecular levels associated with worsening acne | SREBP-1 is a regulator of the production of sapienic acid, a natural antimicrobial. A decrease in the size of the sebaceous gland and SREBP-1 levels in the molecule have been associated with low-carbohydrate diets in acne patients. Additionally, low levels of SREBP-1 reduce the total production of sebum. |
| mTORC1 | Elevated levels associated with worsening acne | It is a regulator of anabolism that targets the progression of the nutrient-dependent cell cycle, and the activation of lipogenesis. High caloric intake, high glycemic load, high consumption of fats and meat, and an increased intake of dairy proteins contribute to elevating mTORC1 through high levels of IGF-1. This increase in mTORC1 signaling contributes to the worsening of acne. FoxO1 acts as a negative regulator of mTORC1. |
| Chocolate | Associated with new lesion formation | This effect could be explained by a high glycemic index after food consumption, leading to an increase in pro-inflammatory cytokines.Block et al.7 discuss a relationship between the amount of chocolate consumed and the number of new acne lesions. |
| Milk | Increased dairy consumption has been associated with worsening acne, although so far, this has only been confirmed in Western populations. | Milk can stimulate the production of IGF-1 in the liver, increasing the levels of this growth factor in the bloodstream. Additionally, milk protein contains high levels of the amino acid glutamine, which plays an important role in the activation of mTORC1, in sebaceous lipogenesis, and in sebocyte proliferation. Scientific evidence on the direct association between dairy products and acne is scarce; however, an association has been confirmed between the worsening of acne and increased dairy intake in Western populations.2 |
| Omega-3 polyunsaturated fatty acids | Elevated levels of foods containing these molecules have been associated with an improvement in acne. | They exhibit anti-inflammatory properties. They lead to a decrease in IGF-1, which in turn reduces the expression of pro-inflammatory cytokines [IL-1B, IL-6, IL-8, TNF-alpha, and matrix metalloproteinases (MMP)] in sebum-producing cells.They also reduce inflammation by decreasing the dimerization of Toll-like receptors 1 (TLR-1) and (TLR-2). The expression of these receptors increases in keratinocytes and macrophages due to the presence of Cutibacterium acnes, leading to inflammation and keratinocyte proliferation. |
| High glycemic index carbohydrates | Elevated levels associated with worsened acne | Increase in IGF-1 levels |
| Fish, resveratrol, curcumin, genistein, and silymarin | Elevated levels associated with improved acne | Suppression of inflammatory cytokines; decrease in IGF-1 levels; inhibition of TLR-1 and TLR-2 dimerization |
IGF-1, insulin-like growth factor 1.
Adapted from Conforti et al.1
Morales-Sánchez et al.6 recently conducted a clinical trial (n=52) with male patients aged 18 to 25 with moderate acne using the same treatment (topical adapalene 0.1% and systemic doxycycline 100mg daily). Patients were randomized into 2 groups based on whether they would receive a low-glycemic diet or a control diet, observing a statistically significant reduction in acne lesions in patients on the low-carbohydrate diet at 12 weeks.
Although more clinical trials are needed to establish whether there is a clear relation between high-glycemic foods, current studies anticipate a protective role of the MD in acne. Regarding dairy, to date, only 1 positive association between increased intake of these foods and worsening acne in Western populations has been reported.
We recommend a diet based on the consumption of fruits, vegetables, whole grains, nuts, extra virgin olive oil, fish, white meats, and a restricted intake of red meats, dairy, and sugary products.