We report the case of a 56-year-old man with a history of fistulizing Crohn disease who presented at the emergency department with metabolic acidosis related to probable sepsis of abdominal origin. During admission, he was treated with multiple antibiotics, parenteral calcium gluconate supplementation, and hemodialysis.
Two weeks later, we were consulted about a series of pruritic skin lesions that had appeared on the patient's left forearm a week earlier.
Physical ExaminationPhysical examination revealed millimetric whitish papules in a sporotrichoid pattern surrounded by an erythematous halo that coalesced to form larger papules and plaques on the anterior surface of the left forearm (Fig. 1). They were firm on palpation, and did not cause any pain or ooze purulent or serous fluid when pressed.
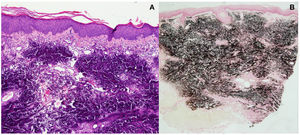
HistopathologyHistopathology showed large calcium salt deposits in the dermis in addition to foreign body-type multinucleated giant cells (Fig. 2A). The deposits stained black with Von Kossa staining, confirming the presence of calcium salts (Fig. 2B).
TestsLaboratory tests show hypocalcemia and elevated creatinine and urea levels; the rest of the values were normal.
What is Your Diagnosis?
DiagnosisIatrogenic calcinosis cutis in a sporotrichoid pattern secondary to calcium gluconate extravasation.
Treatment and Clinical CourseSince calcinosis cutis is a benign condition that resolved spontaneously in the reports to date, we opted for a watch-and-wait approach. At the follow-up visit 4 weeks later, the condition had improved; the inflammation and itching had resolved, and there was also a reduction in the size and number of lesions (Fig. 3).
CommentCalcinosis cutis was described by Virchow in 1855 and refers to the formation of insoluble calcium salt deposits in the skin and subcutaneous tissue. There are 4 types, each with a different pathogenic mechanism: dystrophic, which is preceded by trauma and is associated with normal calcium and phosphate levels; metastatic, which occurs in healthy tissues and is associated with systemic calcium or phospate alterations; idiopathic, which occurs in the absence of metabolic or tissue alterations; and iatrogenic, which occurs following the extravasation of intravenous solutions or the use of intramuscular electrodes containing calcium. Calcium gluconate solution is a very common cause of iatrogenic calcinosis cutis, but other substances, including calcium chloride, have been described.1
The cutaneous manifestations described in most case reports of iatrogenic calcinosis cutis are injection-site papules, plaques, or nodules following extravasation of large quantities of drug. The lesions may initially be associated with erythema, inflammation, and sometimes ulceration and necrosis, and usually develop within days of extravasation.2
Sporotrichoid-like calcinosis cutis, which has been described in the literature, is an uncommon manifestation consisting of calcium salt deposits along the veins of the forearm. Sporotrichoid spread is believed to occur after a transient increase in venous pressure and stasis during intravenous infusion of calcium solution. This increase can be caused by cuff ballooning for blood pressure measurement, which would result in extravasation of the solution along the veins of the forearm.3
Diagnosis is clinical, and histopathology shows calcium salt deposits in the dermis, with or without giant foreign body-type cells.
Iatrogenic calcinosis cutis is usually benign and resolves spontaneously within 2 to 6 months. It can, however, lead to complications such as soft tissue necrosis and secondary infections. Several treatments have been described, including topical sodium thiosulfate,4 intralesional triamcinolone acetonide injections,5 diltiazem, and surgical interventions,6 but their efficacy has not been investigated in clinical trials.
To prevent iatrogenic calcinosis cutis, it is important to use a clean, unobstructed line and avoid the use of a pressure cuff during intravenous administration of calcium preparations.
Conflicts of InterestThe authors declare that they have no conflicts of interest.