Vascular hyperplasia is a common finding in prurigo nodularis/lichen simplex chronicus (LSC). The term prurigiform angiomatosis was recently proposed to describe a histologic pattern characterized by prominent vascular hyperplasia in patients with LSC. The aim of this study was to identify cases of LSC with this pattern and analyze associations with clinical and pathologic features and disease course. We reviewed 54 cases of histologically confirmed LSC and detected findings consistent with prurigiform angiomatosis in 10 (18.5%). The patients (7 men, 3 women) had a mean age of 59.7 years. The lesions were pruritic and predominantly located on the extremities and trunk. The most notable histologic finding was vascular proliferation in the superficial dermis associated with a lymphocytic inflammatory infiltrate. Recognition of prurigiform angiomatosis is important as it helps not only to distinguish LSC from other entities (mainly vascular tumors) but also to detect lesions that need to be surgically excised due to poor response to topical treatment.
En el prurigo nodular/liquen simple crónico (LSC) es frecuente observar hiperplasia vascular. Recientemente, se ha propuesto el término angiomatosis prurigiforme (AP) para describir un patrón histológico en aquellos casos de LSC en los que la hiperplasia vascular asociada es prominente. El objetivo del estudio fue identificar los casos de LSC con patrón de AP y analizar sus características clínico-patológicas y evolución. Se revisaron 54 casos con diagnóstico histológico de LSC, diez de los cuales (18,5%) mostraron criterios de AP (7 varones, 3 mujeres, edad media: 59,7 años). Clínicamente, las lesiones eran pruriginosas y se localizaban predominantemente en extremidades y tronco. Histológicamente, el hallazgo más destacable fue la proliferación vascular en dermis superficial asociada a infiltrado inflamatorio linfocitario. La importancia de reconocer este patrón radica, además del diagnóstico diferencial que plantea principalmente con los tumores vasculares, en la limitada respuesta en algunos casos al tratamiento tópico, siendo necesaria su exéresis quirúrgica.
Recently, the term prurigiform angiomatosis (PA)1 has been proposed to describe a histopathological pattern characterized by prominent dermal vascular proliferation of capillaries and postcapillary venules of non-lobular distribution due to epidermal changes similar to those observed in nodular prurigo/lichen simplex chronicus (LSC).1 Previously, Kacerovska et al. described acquired “hemangioma-like” changes in lesions located on knees and elbows with histopathological findings consistent with nodular prurigo/LSC with marked subepidermal vascular proliferation.2 Although the exact mechanism through which PA changes occur is still unknown, some authors hypothesize it has to do with its reactive nature and suggest that mechanical damage, chronic pressure, and inflammation would be the triggers for the observed reactive angiogenesis.2 One of the most important angiogenic factors is the vascular endothelial growth factor (VEGF), which has previously been shown to be upregulated in various inflammatory and tumoral contexts at skin level.3
The interest in recognizing the PA pattern lies in the clinical and histopathological differential diagnosis it may present, mainly with vascular tumors,4 as this condition can cause uncontrollable itching and may also be refractory to medical therapy, requiring surgical excision in some cases.
The aim of this study was to identify cases of nodular prurigo/LSC with associated histopathological criteria of PA and analyze their clinical and histopathological characteristics, and the course of the disease.
Material and methodsThis was a retrospective, observational study of data from patients with a histopathological diagnosis of nodular prurigo/LSC, evaluated at our center from 2015 through 2020 to reevaluate both entities histopathologically in an attempt to identify those cases with a histopathological pattern consistent with PA. The hematoxylin-eosin sections corresponding to the selected cases were retrieved from the archives of our service for histopathological examination. Lesions located on the vulva and penis were excluded. Clinical information obtained and related to follow-up was provided by the dermatology service.
ResultsClinical findingsA total of 54 biopsies were reviewed, 10 of which (18.5%) showed prominent vascular proliferation due to the epidermal changes of LSC, which corresponded to 7 men and 3 women with a mean age of 59.7 years. Patients consulted for itching caused by the lesions and bleeding from scratching. The lesions presented as erythematous-violaceous, indurated, and pruritic plaques and nodules, some excoriated due to scratching, and often located in areas easily accessible to scratching such as extremities (#3), trunk (#3), buttocks (#2), or head (#2) (figure 1A-B).
In cases of multiple lesions (#5), the initial diagnostic orientation was nodular prurigo/LSC to rule out a cutaneous lymphoproliferative process, or other cutaneous neoplasms through biopsy. However, in cases of single or scarce lesions (#5), the differential diagnosis was between LSC and keratinizing tumor lesions, such as papilloma, or squamous cell carcinoma.
In 4 cases of single lesions, excision of the lesion was chosen, achieving healing. No recurrences were seen in the short-term on the scar.
In cases of multiple lesions, topical treatment with corticosteroids was initially chosen, achieving complete remission in most cases. In some of them, topical treatment was supplemented with oral corticosteroids (#1), or oral methotrexate (#2) to prevent relapses. The discontinuation of treatment often led to recurrence of the lesions, and after discontinuation, most patients started showing lesions 30 days to 3 months after discontinuation.
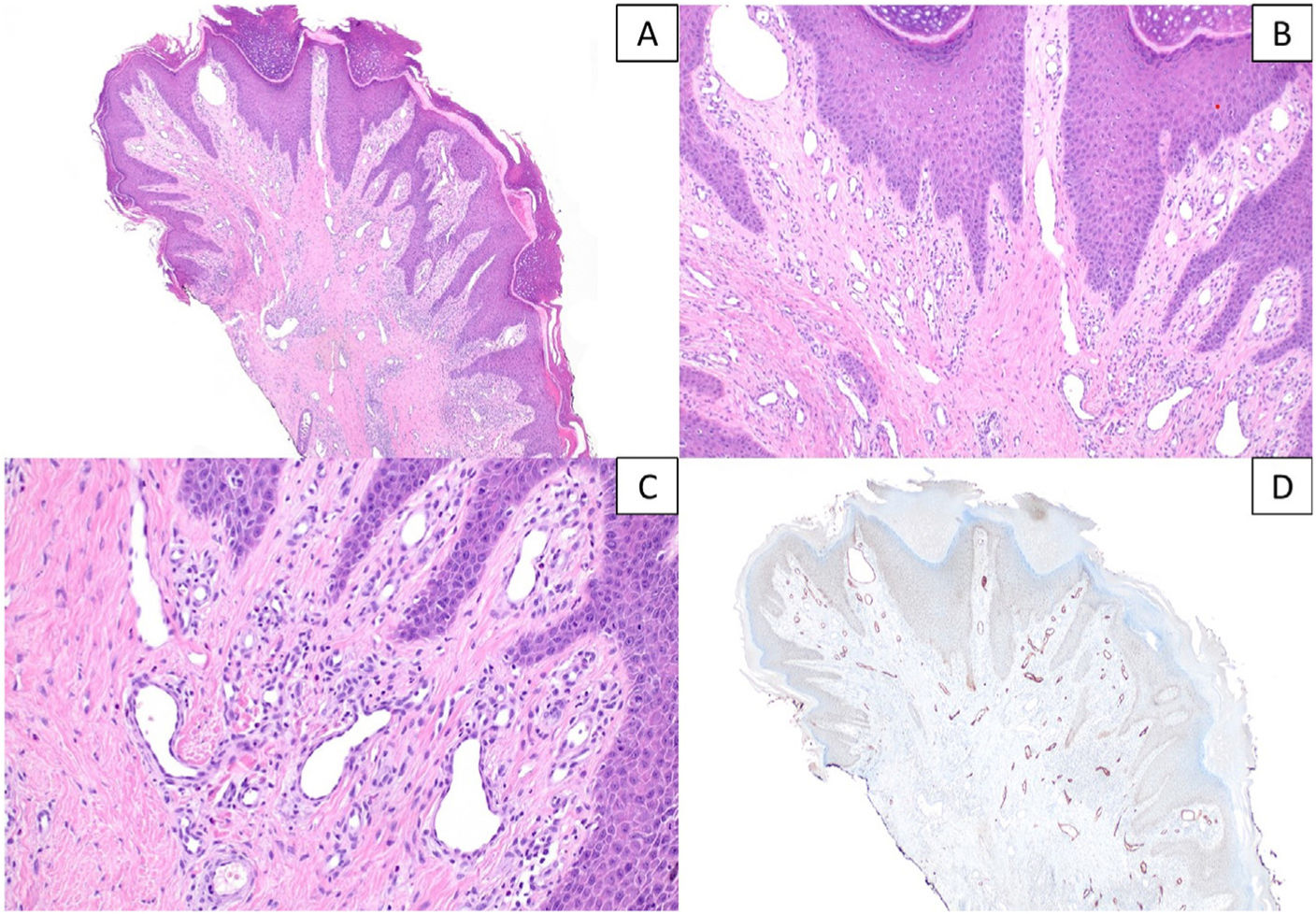
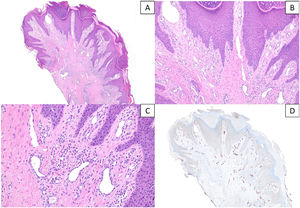
Histopathological findingsHistopathologically, the most remarkable finding in all cases, in addition to the changes of nodular prurigo/LSC, was the associated underlying subepidermal vascular proliferation, consisting of capillaries and/or postcapillary venules mainly distributed on the superficial dermis and accompanied by a mild-to-moderate predominantly lymphocytic infiltrate (figure 2A-C). Immunohistochemical study with D2-40 (podoplanin) was able to characterize the dermal vascular proliferation in 7 cases with histopathological criteria of PA. More lymphatic vessels intermixed with blood vessels were observed plus some occasional lymphangiectasias. This increase was categorized as mild in 4 cases and moderate in 3. In the remaining 3 cases, the study could not be conducted because we could not recover the paraffin (figure 2D). Differential diagnosis of vascular tumor was considered in 3 of these biopsies (figure 3). Changes to epidermal hyperplasia were observed in all the cases, mostly irregular, with focal parakeratosis and a discretely verrucous pattern in 5 of these cases. No microabscesses of neutrophil polymorphonuclear leukocytes were observed in the stratum corneum, or thinning of the supra-papillary plates, or associated ulceration.
A and B) Histopathological sections showing epidermal changes of nodular prurigo/lichen simplex chronicus with prominent vascular proliferation on the superficial dermis, associated with a mild-to-moderate lymphocytic inflammatory infiltrate (hematoxylin & eosin, x40 and x100). C) Detail at higher magnification of vascular proliferation mainly composed of capillaries, without any signs of endothelial atypia (hematoxylin & eosin, x200). D) Immunohistochemical staining for D2-40 (podoplanin) highlighting the moderate increase in lymphatic vessels, with occasional dilatations (x40).
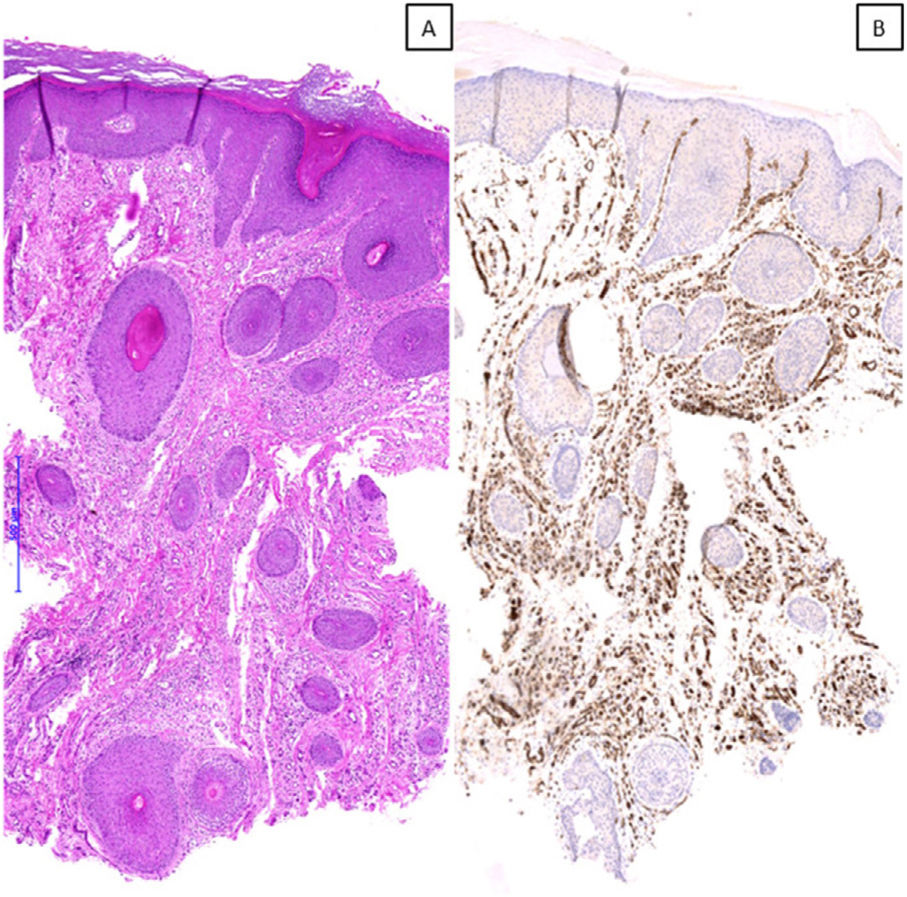
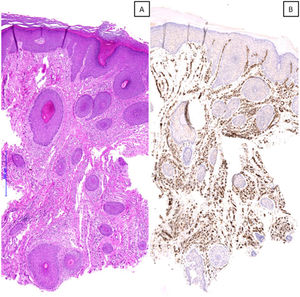
A) Microscopic image of a case with a histopathological pattern of prurigiform angiomatosis, showing a marked vascular proliferation on the superficial, mid, and deep dermis, suggesting the differential diagnosis of a vascular tumor (hematoxylin & eosin, x40). B) Immunohistochemical staining for CD31 confirming the observed findings (x40).
Dermal vascular proliferation was associated with a predominantly lymphocytic inflammatory infiltrate of perivascular and interstitial pattern, ranging from mild (#7) to moderate (#3). Other findings detected in the dermis were fibrosis [mild (#4) and moderate (#1)] and edema [mild (#4)]. No signs of vasculitis or vascular atypia were identified in any of the cases studied.
DiscussionIn nodular prurigo/LSC, an increase in dermal vascular structures is frequently observed.5 However, in some cases, this vascular hyperplasia can be significant and lead to a histopathological differential diagnosis of vascular tumor.4 The term “prurigiform angiomatosis”1 has been coined specifically to refer to this clinical-pathological context, more commonly described in sites prone to certain pressure such as the buttocks or the intergluteal fold2 in elderly patients. Senile gluteal dermatosis (SGD) is a common but underdiagnosed entity reported in patients with gluteal lesions related to chronic pressure exerted in this area. Both the clinical and histopathological findings of SGD are common to those of the PA, except for the specific location of the SGD (buttocks and intergluteal fold) and its histopathological nonspecificity, with hyperkeratosis, psoriasiform epidermal hyperplasia, acanthosis, and vascular proliferation/dilation on the superficial dermis with mild accompanying lymphohistiocytic inflammation frequently observed. Therefore, recently Liang et al. have proposed to unify both entities under the term REAR (Reactive Epidermal Hyperplasia and Angiogenesis of the Rear),6 not only for to the clinical-pathological similarities, but also for the patients’ age in whom both entities usually present (5th-6th decades of life), making the term “senile” inappropriate. Similarly, the term “prurigiform” used in PA refers to the morphology of nodular prurigo/LSC and not specifically to the symptom of itching. Clinically, the differential diagnosis should be considered with tumor lesions (squamous cell carcinoma, lymphoma, extramammary Paget's disease), and cutaneous inflammatory diseases such as eczema, psoriasis, or pressure ulcers, among others.1,7
In our series of cases, the lesions were preferably located on the upper and lower limbs, trunk, and intergluteal fold, and patients presented associated symptoms such as itching and/or excoriation. In cases with single lesions, surgical excision was the treatment of choice, with no recurrences seen in the short term. However, in patients with multiple lesions, topical corticosteroid therapy was chosen, achieving good results in most cases, and supplemented with oral corticosteroids or oral methotrexate in some of them to prevent relapses.
The histopathological findings observed in our case series are consistent with those previously described in the scientific medical literature currently available.1 The absence of a lobular pattern and hemosiderin deposits contribute to histopathologically distinguish the PA pattern from changes due to vascular insufficiency.7 The study published by Liang et al.6 describes 4 cases with histopathological characteristics consistent with PA and more associated lymphatic vessels [mild (n = 3) and moderate (n = 1] intermixed with blood vessels resembling capillaries. This finding suggests that, at least in some cases of PA, lymphatic vessels could contribute to neovascularization.
Although the exact pathophysiology is still unknown, some authors2,6 suggest that inflammation, mechanical damage, or chronic pressure with consequent hypoxia could act as triggers of the reactive angiogenesis/lymphangiogenesis process, mediated by the production of VEGF by keratinocytes and endothelial cells to counteract the situation of hypoperfusion. Former studies have shown that under normal conditions, VEGFs are present in the epidermis at low levels and may be overexpressed in inflammatory or neoplastic processes that associate increased vascular angiogenesis and permeability, such as psoriasis or atopic dermatitis.3,8
In conclusion, term PA has recently been proposed to describe a distinctive histopathological pattern. The importance of recognizing it, in addition to the extensive clinical-pathological differential diagnosis it presents, lies in the limited response to topical therapy that may occur in a significant number of cases with single lesions, requiring complete excision, and the prevention of relapses with oral corticosteroids or methotrexate in those with multiple presentations.
FundingNone declared.
Conflicts of interestNone declared.