Few reports describing an association between UV radiation and fixed skin eruptions have been published since 1975. These reactions have received various names, including fixed sunlight eruption, fixed exanthema due to UV radiation, and broad-spectrum abnormal localized photosensitivity syndrome. We present a series of 13 patients (4 men [30.8%] and 9 women [69.2%]) aged between 28 and 56 years who were evaluated for fixed eruptions induced by UV radiation at a dermatology referral hospital in Bogotá, Colombia. The lesions were located on the inner thighs, buttocks, popliteal region, anterior and posterior axilla, and dorsum of the feet. Photoprovocation reproduced lesions in all the affected areas, and histopathology showed changes similar to those seen in fixed drug eruptions. While these UV-provoked reactions may be a type of fixed skin eruption, we cannot rule out that they may also be a distinct condition that simply shares a pathogenic mechanism with fixed eruptions.
Desde 1975 se han publicado algunos casos que asocian la radiación ultravioleta como un desencadenante de erupciones cutáneas fijas (erupción o exantema fijo por luz solar, o síndrome de fotosensibilidad localizada de amplio espectro). Describimos 13 pacientes con esta dermatosis, 4 (30,8%) hombres y 9 (69,2%) mujeres, con edades entre los 28 y 56 años, atendidos en un centro de referencia en dermatología en Bogotá (Colombia). Las lesiones se localizaron en la cara interna de los muslos, glúteos, región poplítea, axilar anterior y posterior y dorso de los pies. La prueba de fotoprovocación logró la reproducción de las lesiones en todos los casos en las áreas afectadas y la histopatología reveló cambios similares a los descritos en los eritemas fijos por medicamentos. Esta enfermedad podría corresponder a un subtipo de erupción fija, aunque no se descarta que sea una dermatosis diferente con una patogenia común.
A fixed eruption is a skin or mucous membrane exanthem that recurs on the same site after exposure to a trigger, being the most common trigger the use of topical or oral drugs.1,2 However, up to 25.2% of the patients with similar lesions deny using any drugs.3 Other causes of fixed skin eruptions have been identified, such as food,4,5 exposure to dyes, herbicides, and insecticides.3,6
In 1975, Emmett described the unusual association between a fixed eruption and sunlight exposure.7 Afterwards, several similar cases have been reported to date.8–11 In 2010, the term fixed sunlight eruption was coined,10 and more recently, the name broad-spectrum abnormal localized photosensitivity syndrome was proposed.11
These are the cases of 13 patients evaluated at the photodermatology unit of a dermatology reference center based in Bogota, Colombia, with clinical, histopathological, and photoprovocation testing regarding this dermatosis.
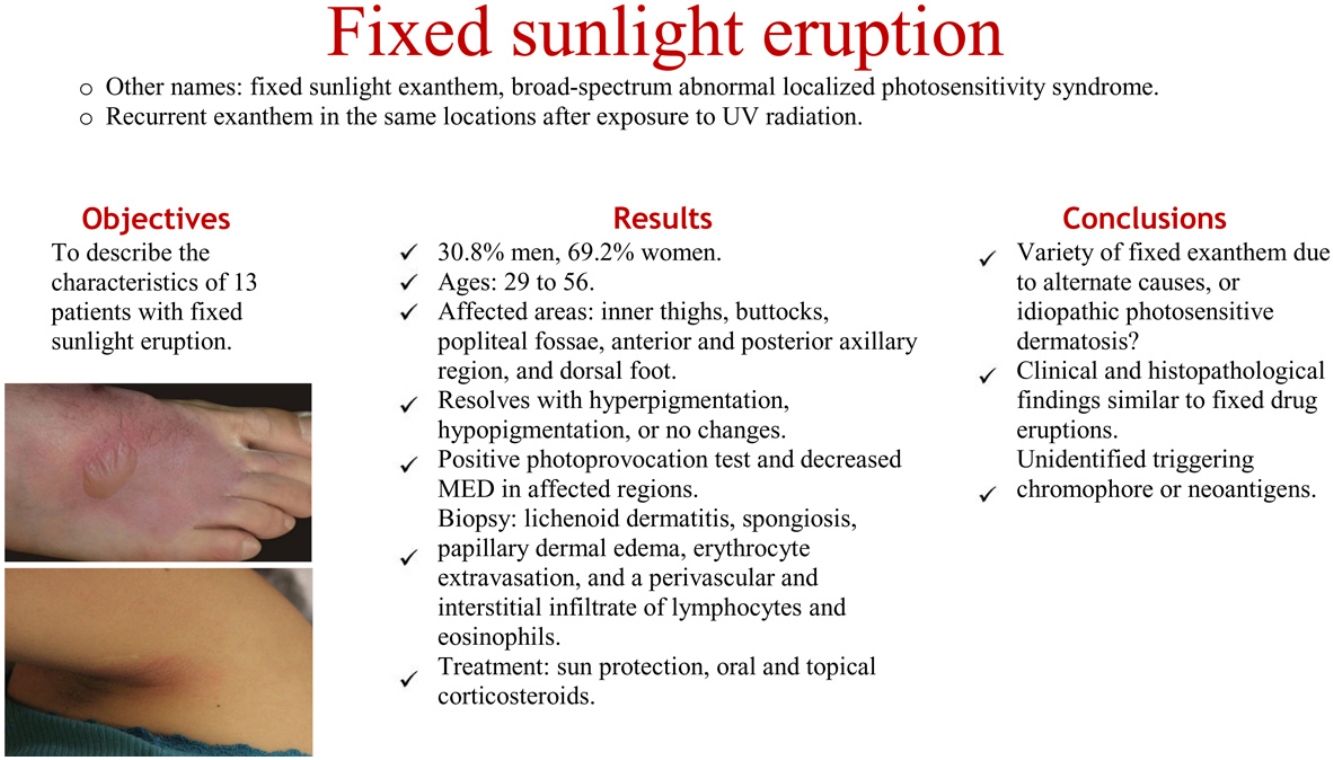
Case descriptionA total of 13 patients including 4 men (30.8%) and 9 women (69.2%) between the ages of 28 and 56 years were treated at Hospital Universitario Centro Dermatológico Federico Lleras Acosta, Bogotá, Colombia from 2011 through 2021. They all reported a 1-to-12-year history of pruritic and burning skin lesions on the same sites, which appeared from half an hour to 24hours after sun exposure and improved 3 to 8 days later. Clinically, the lesions were round, or oval well-demarcated erythematous or erythematous-violaceous macules or plaques, some of them with blisters resolving with residual hyperpigmentation (5 cases), hypopigmentation (1 case), or no skin changes behind (7 cases). The most common sites were the inner thighs, the buttocks, the popliteal fossae, the anterior and posterior axillary regions, and the dorsum of the feet (Fig. 1). No drug or food consumption was identified before the onset of the lesions (see supplementary data).
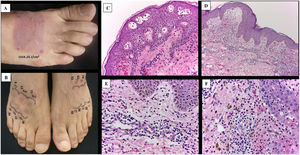
All patients underwent a complete blood count, ANA, anti-Ro, and anti-La tests, and only 2 patients revealed changes of some sort: 1 patient with a history of Sjögren's syndrome had positive anti-Ro antibodies, and another one who tested positive to the ANA test (titer of 1/160). However, no traces of autoimmunity were seen. Photoprovocation testing was performed using a single or repeated dose of 25J/cm2 of UVA according to the protocol of the unit, using a Daavlin hand and foot phototherapy booth (Bryan, OH, United States), which tested positive in all the patients in the affected regions (Fig. 2A) and negative in the regions unaffected by the rash. The minimal erythematous dose (MED) for UVB was determined in 4 cases, in both the affected and unaffected regions using the 601 Solar Light Multiport® simulator of 300 mw (Glenside, PA, United States), deny using decreased MED only in the affected regions (Fig. 2B).
A) Positive photoprovocation test. B) Comparison of MED in affected and unaffected skin, dose in mJ/cm2. C-F) Histopathological appearance of the lesions. C) Formation of intraepidermal vesicles with apoptotic cells (H&E, ×10). D) Epidermis with presence of apoptotic cells, upper dermis edema, along with perivascular lichenoid-like infiltrate. E and F) Infiltrate in the upper dermis with predominant lymphocytes and interspersed eosinophils and incontinence of melanin pigment (H&E, ×40).
Skin biopsies were taken from the sunlight-induced skin lesions, or from photoprovoked lesions, which revealed similar histopathological findings in all cases: lichenoid dermatitis with spongiosis, papillary dermal edema, erythrocyte extravasation, and a perivascular and interstitial infiltrate of lymphocytes and eosinophils. In some cases, several apoptotic keratinocytes were seen in both the basal and suprabasal layers of the epidermis (Fig. 2C-F).
Based on the clinical, photobiological, and histopathological findings made, all cases were diagnosed with fixed sunlight eruption. Photoprotection measures were advised, including proper clothing and broad-spectrum sunscreens. In 3 patients who traveled tosunny places, prednisolone at a dose of 0.5mg/kg/day was administered for their entire stay to prevent the occurrence of lesions. Another 2 patients applied a physical sunscreen to the affected areas, thus preventing any eruptions from happening after a new UVA photoprovocation test. A total of 9 of the patients were contacted during the entire follow-up. Only 1 patient did not experience any more lesions after 3 months living in a sunny region, 5 prevented the eruption using physical sunscreens and protective clothing, and the remaining 3 could only control the appearance of lesions with these measures partially.
DiscussionThe exanthem triggered by exposure to UV radiation, which recurs in the same bodily areas, is a dermatosis with unclear pathophysiology. The medical literature reviewed to date has confirmed a total of 19 cases under names such as fixed long wavelength-UV eruption,7 fixed UV radiation eruption,8,12, fixed sunlight eruption,10,13–15 and broad-spectrum abnormal localized photosensitivity syndrome.11
According to former studies, this dermatosis predominantly affects women, as was the case in our series. Butt et al.11 reported that the mean mean age at onset of their 10 patients was 37 years, which is similar to the mean age of our cases (38 years). They sought medical care after a mean time of 8 years, compared to 5 years in our patients. The time elapsed from sun exposure to lesion onset ranged from 30min to 18hours, which is similar to that of our patients (30min to 24hours). While eruption resolved within 7 to 28 days, our cases resolved much faster (3 to 8 days).
The exanthem often appears in skin areas protected from sun-exposure, such as inner thighs, buttocks, popliteal fossae, hips, periaxillary regions, and less frequently, fingers and dorsum of the feet,10,12–15 similar to our patients. This distribution differs from the typical sites involved in fixed drug eruptions (lips, hands, and genitals).1 Characteristically, fixed sunlight eruption is not associated with the presence of abnormal lab test results. In this case series, 1 patient had Sjögren's syndrome and positive anti-Ro antibodies, a disease not previously associated with this type of lesions, and another one showed a positive ANA test positive ANA test (low titers) without any autoimmune associations.
Histopathological changes are consistent in all described cases, including those of our series, with an infiltrate of variable intensity—perivascular or band-like—of lymphocytes, eosinophils, and neutrophils, along with vacuolar or lichenoid damage of the interface, epidermal spongiosis, apoptosis of keratinocytes, and in some cases, melanin deposits on the superficial dermis.9,10,12,13,15. These findings are similar to those of fixed eruptions associated with drugs and foods.4
Photosensitivity to UVA and UVB radiation, and sometimes visible light can be seen in the affected skin.7,9,11,15 In some cases, there is an impaired photosensitivity in regions close to these lesions, or in unaffected sites, although much less compared to the affected areas.11 It has been possible to reproduce the lesions with low doses of UVA in previously affected areas, but not in unaffected skin,12,14,15 as our cases confirmed. After the exanthem resolved, the skin may remain unchanged or exhibit hypo- or hyper-pigmentation, as it also happens with fixed eruptions associated with drugs, although residual hyperpigmentation is more common in the latter.1
Regarding treatment, the use of protective clothing and broad-spectrum sunscreens is helpful.11,13,15 Topical corticosteroids reduce symptoms, accelerate lesion resolution, and in some cases, the prophylactic use of narrow-band UVB or UVA-1 phototherapy has improved photosensitivity.11 Oral corticosteroids prevented the appearance of lesions in 3 of our patients. However, these drugs cannot be used on a long-term basis considering their adverse effects.
Some authors suggest that this reaction could be a subtype of fixed eruption,12 while others consider it an immunologically mediated photodermatosis.13,14 The trigger or antigen activated by UV radiation is still unknown. An unidentified chromophores falling onto the skin and absorbing the wavelengths responsible for triggering this local reaction has been suggested.11 Others speculate that a photosensitive substance such as a food or some additive may be responsible.13 However, no triggering substance has ever been identified.
Several publications that this photosensitive dermatosis might not be a variety of fixed eruption because the lack of residual pigmentation, and histopathology changes.11,13 However, not all fixed eruptions leave residual hyperpigmentation; there are subtypes without pigmentary changes,16,17 while others exhibit hypopigmentation,18 which are 3 situations described in our case series. Additionally, if all the cases described are evaluated, the histopathological findings are consistent with those seen in fixed drug and food eruptions, especially in non-pigmented lesions.1,17,19 We can assert that these 2 diseases share several clinical and histopathological features, except for the involvement of mucous membranes, which is common in drug-induced fixed eruptions.
In conclusion, this photodermatosis could be a subtype of fixed eruption due to the deposition of some type of chromophore, or to the expression of UV radiation-induced neoantigens. Although, the possibility that we’re dealing with a different disease with a common pathogenesis cannot be ruled out.
FundingNone declared.
Conflicts of interestNone declared.