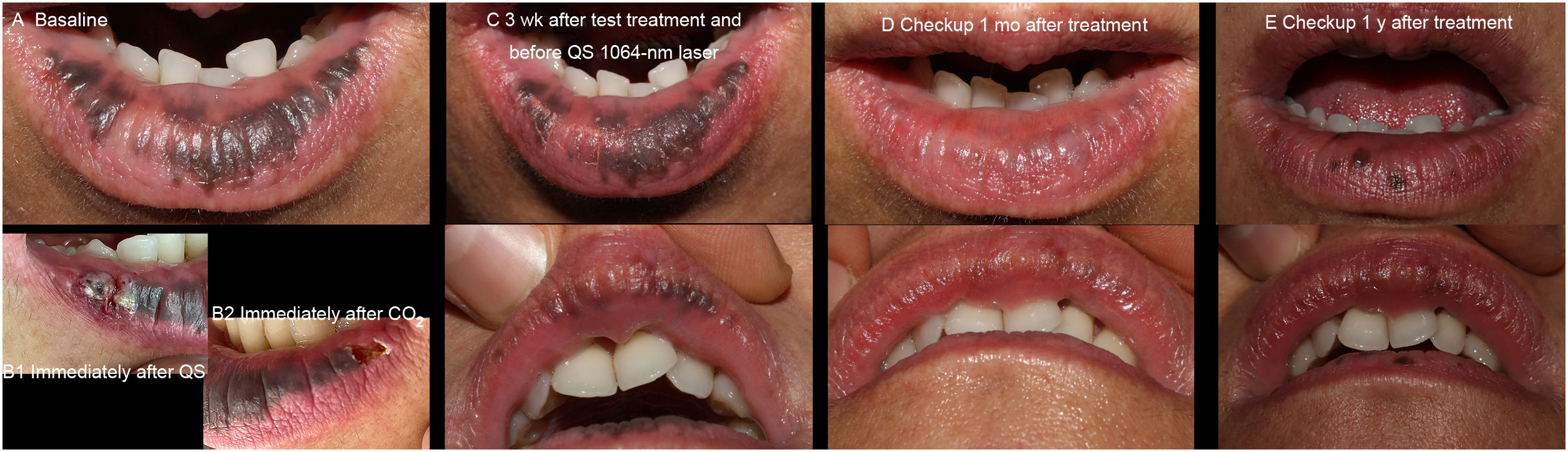
We report the case of a 35-year-old woman diagnosed with Laugier-Hunziker syndrome 20 years previously who inquired about the possibility of cosmetic treatment for coalescent pigmented macules on the vermilion border of both lips (Fig. 1A) that also partially affected the mucosa.
Photographs of the patient's clinical condition. A, Baseline. B1, Reaction immediately following a specific test treatment with the Q-switched Nd:YAG laser. B2, Reaction immediately after a specific test treatment with the carbon dioxide laser. C, Three weeks after the test treatment. Note how the 2 treated areas are similar in appearance with respect to resolution of pigmentation. D, Response to complete treatment with Q-switched Nd:YAG laser 1 month after the session. E, One year after a complete session recorded in image (C), with partial recurrence on the lower lip. This was later successfully treated following the same therapy schedule.
After obtaining her informed consent, we applied a test treatment under topical anesthetic at a specific spot on the right side of the lower lip with a Q-switched 1064-nm neodymium:YAG laser (Fig. 1B1) at 1500mJ/cm2 and at another on the left using a carbon dioxide laser (Fig. 1B2) (0.9W, 50Hz), with permanence, and in DEKA HP mode, a specific mode of the laser with reducing permanence for each shot. The approach does not require gel and generates less local heat, thus leading the laser to function in a similar way to an erbium:YAG laser. Treatment was prescribed with betamethasone cream 0.05% and gentamicin cream 0.1% twice daily during the 3 days following treatment. At least once-daily application of gel dressing was recommended during the following 2 weeks. The patient's clinical condition progressed in the form of hemorrhagic blisters and inflammation (more evident on the side treated with carbon dioxide laser) that developed during the 72h following treatment and, on the seventh day, gave way to superficial erosions that resolved completely in 2 weeks.
Both treatments proved equally effective at a checkup 2–3 weeks later (Fig. 1C), although more persistent discomfort and inflammation were observed in the area treated with carbon dioxide laser. Consequently, we opted for the treatment that led to a better postoperative outcome for the patient.
One month after this single session of Q-switched laser, the pigmented macules had almost completely disappeared on both the upper and lower lips (Fig. 1D). One year later, solitary macules had appeared on the lower lip (Fig. 1E). Further treatment of these lesions was successful.
Laugier-Hunziker syndrome is a benign, idiopathic disorder characterized by mucocutaneous macular hyperpigmentation mainly affecting the lips in the form of asymptomatic brown-to-black macules. It is accompanied by longitudinal melanonychia and pseudo-Hutchinson sign in up to 60% of cases.1 Histologically, the lesion is characterized by accumulation of melanin in the superficial dermis.2 Diagnosis is based on clinical features and by exclusion, ruling out other lesions that progress with mucocutaneous hyperpigmentation and systemic involvement, such as Peutz-Jeghers syndrome, Addison disease, and McCune-Albright syndrome.2 Treatment is cosmetic, and the effective therapeutic options reported in the literature include cryotherapy and various laser treatments (Q-switched 532-nm and 1064-nm Nd:YAG, Q-switched alexandrite, erbium:YAG, carbon dioxide, and diode).1–4 The relevant available literature is scarce and discusses mainly treatment with the Q-switched 532-nm Nd:YAG laser. Nevertheless, in one systematic review, various types of oral lesion were treated using different light devices with varying wavelengths.4 Furthermore, in our opinion, using a longer wavelength enables treatment of the superficial and deeper strata simultaneously. Treatment can also be applied less selectively, although as effectively, with carbon dioxide laser. Therefore, we used a test approach in this patient, whose previous treatments had proven unsuccessful.
The present manuscript highlights several points. First, it compares 2 lasers in the same patient. The outcome is equivalent, thus paving the way for alternative treatments in centers with limited availability of light sources. Second, it provides photographic images for each of the steps followed; this could prove useful for patients with a similar condition seeking cosmetic treatment for hyperpigmentation. Third, follow-up was over a long period, thus providing information on the long-term posttreatment clinical course and helping to plan in cases where the patient wishes to extend treatment of the lesions over time.
Conflicts of InterestThe authors declare that they have no conflicts of interest with respect to the present article.