Acral lentiginous melanoma (ALM) arises in areas that are not generally exposed to UV radiation. Chronic trauma has been hypothesized to play a role in the development of this tumor. The aim of this study was to analyze the association between the presence and characteristics of ALM and location in stress- and non–stress-bearing areas.
Material and methodsObservational, descriptive analysis. For 95 patients with ALM evaluated at Fundación Clínica Vida in Medellin, Colombia between January 2016 and August 2020 we collected demographic, histologic and clinical variables and assigned the patients to 2 groups depending on whether their tumor was located in a stress-bearing area or not.
ResultsNinety-five patients (36 men and 59 women) with a median age of 59 years were studied. ALMs were more common in stress-bearing areas than in non–stress-bearing areas (58 [61%] vs. 17 [17.8%]). A history of direct trauma at the site of the tumor was reported in 18.9% of the cases (p = .025) and was most common in patients with nail lesions. Invasive ALMs in stress-bearing areas had a greater Breslow thickness (p = .006) and higher ulceration rates than those in non–stress-bearing areas (p = .018).
ConclusionsALM on both the feet and hands is more common in stress-bearing areas. Our findings support the hypothesis that mechanical stress may have a pathogenic role in ALM.
El melanoma lentiginoso acral (MLA) se presenta en zonas con poca exposición a la radiación ultravioleta. Se ha planteado que el trauma crónico puede predisponer a su desarrollo. El objetivo del presente estudio fue relacionar la presencia del MLA y sus características con las zonas acrales que se consideran de presión y de no presión.
Material y métodosSe realizó un estudio observacional, descriptivo, con intención analítica. Se recogieron los datos de 95 pacientes con diagnóstico de MLA evaluados en la Fundación Clínica Vida en Medellín, Colombia, entre enero de 2016 y agosto de 2020. Se recolectaron variables demográficas, histológicas y clínicas del tumor, las cuales se analizaron en dos grupos, según si estaba sometida a fuerzas de presión o no.
ResultadosSe incluyeron 95 pacientes con MLA (36 hombres y 59 mujeres), con una mediana de edad de 59 años. Se presentaron más melanomas en las zonas de presión que de no presión (58 [61%] vs. 17 [17,8%]). Se refirió la existencia de un trauma directo previo en 18,9% de los casos, el cual fue más frecuente en las lesiones de las uñas (p = 0,025). Los melanomas invasores tuvieron un mayor Breslow (p = 0,006) y presencia de ulceración (p = 0,018) en las zonas de presión y en las uñas que en las zonas de no presión.
ConclusionesEl MLA es más frecuente en zonas de presión que de no presión, tanto en la mano como en el pie. Esto apoya la hipótesis de que el estrés mecánico puede jugar un papel en la patogénesis de este tipo de tumor.
Acral lentiginous melanoma (ALM) is a subtype of melanoma that occurs on the palms, soles, and nail bed. While the incidence is the same in all populations, its proportion of the total of all melanomas ranges between 1% and 7% in the Caucasian phenotype,1 up to 15% in the Hispanic phenotype,2 between 45% and 58% in the Asian phenotype, and 70% in the black phenotype.3,4
The behavior of this tumor is different than that of melanomas in other locations. Specific risk factors have been reported, as ALM is less associated with light phototypes or pre-existing melanocytic nevus and tends to present in areas with little exposure to ultraviolet radiation (UVR).5–7
It has been suggested that chronic trauma in acral areas may predispose the patient to presenting this type of tumor.5 This is because it presents more frequently in areas of greater mechanical stress, the front and rear areas of the foot, suggesting that it is because the pressure leads to greater damage to the skin and, in turn, a higher propensity to develop ALM, in comparison with other areas considered non–stress-bearing areas.5,6 Although fewer studies of ALM are available, findings have also been observed that support this hypothesis, such as the fact that melanomas, unlike nevus, are not located on the proximal area of the palm but on the pads and on the distal part of the palm, which tends to present greater mechanical stress.8
The objective of this study was to link ALM and its characteristics with the acral areas that are considered stress-bearing and non–stress-bearing areas.
Material and MethodsWe performed a retrospective observational study following the recommendations of the Strobe guidelines.9 Data were collected from patients with a diagnosis of ALM who had been evaluated in the Fundación Clínica Vida in Medellín, Colombia, the city’s referral center for skin-cancer treatment, between January 2016 and August 2020.
The data were obtained from a mixed source of information through electronic patient records and a telephone questionnaire was administered to complete the missing information. The location of the lesion was specified by means of an image sent to the patient, showing the affected extremity divided into areas so that the patient could indicate the affected area, thus allowing for an objective classification.
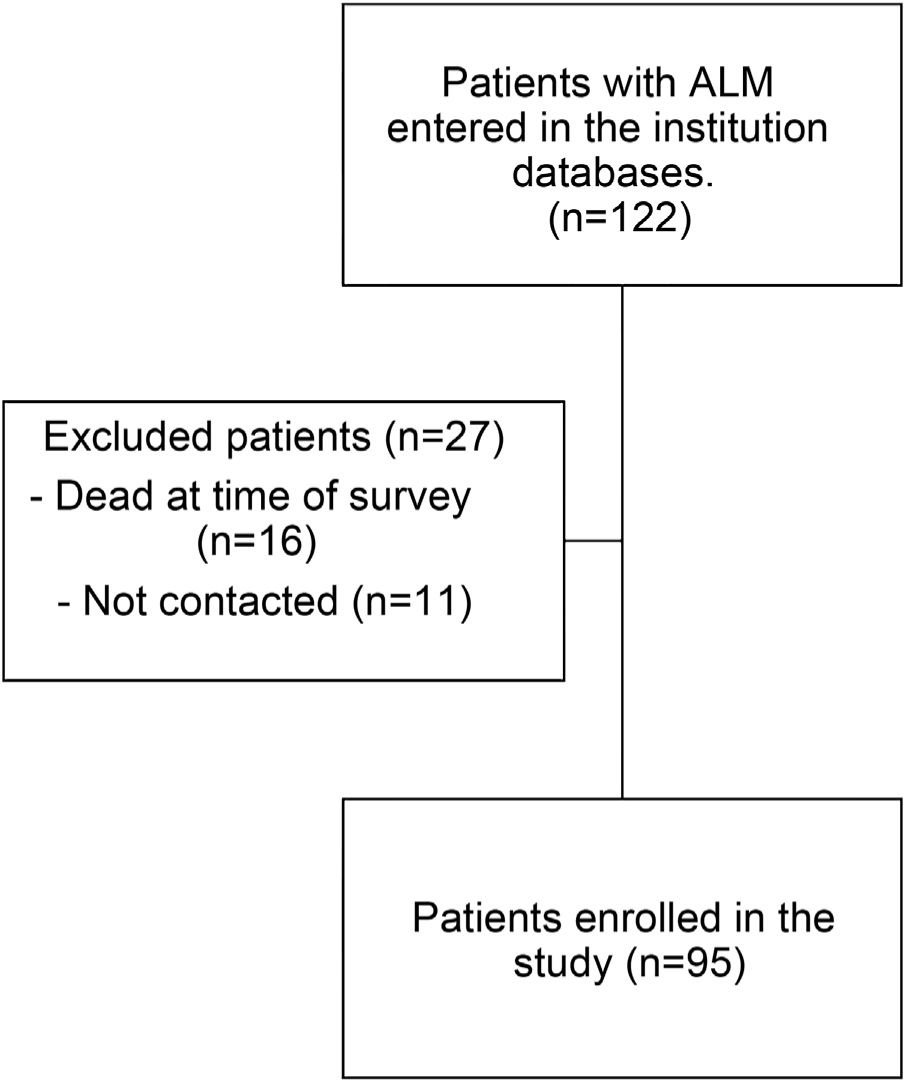
Inclusion criteria were patients with a diagnosis of ALM confirmed by histopathology, with no distant metastasis (those patients were excluded, as the event presented in 4 cases, for whom complete histiologic staging information of the primary melanoma was not available). Patients who had died at the time of the study were excluded, as were those whom it was not possible to contact to administer the telephone survey.
The study and all its procedures were approved by the ethics committee of Fundación Clínica Vida.
Demographic data such as age and sex were collected. Subjects were asked whether they had a history of direct trauma to the areas of the tumor and about lateral dominance (right-handedness or left-handedness). Furthermore, when the telephone survey was administered, the weight and height of the patient was recorded to calculate the body mass index (BMI), which was categorized according to the overweight and obese classification proposed by the World Health Organization (WHO) expert committee.10
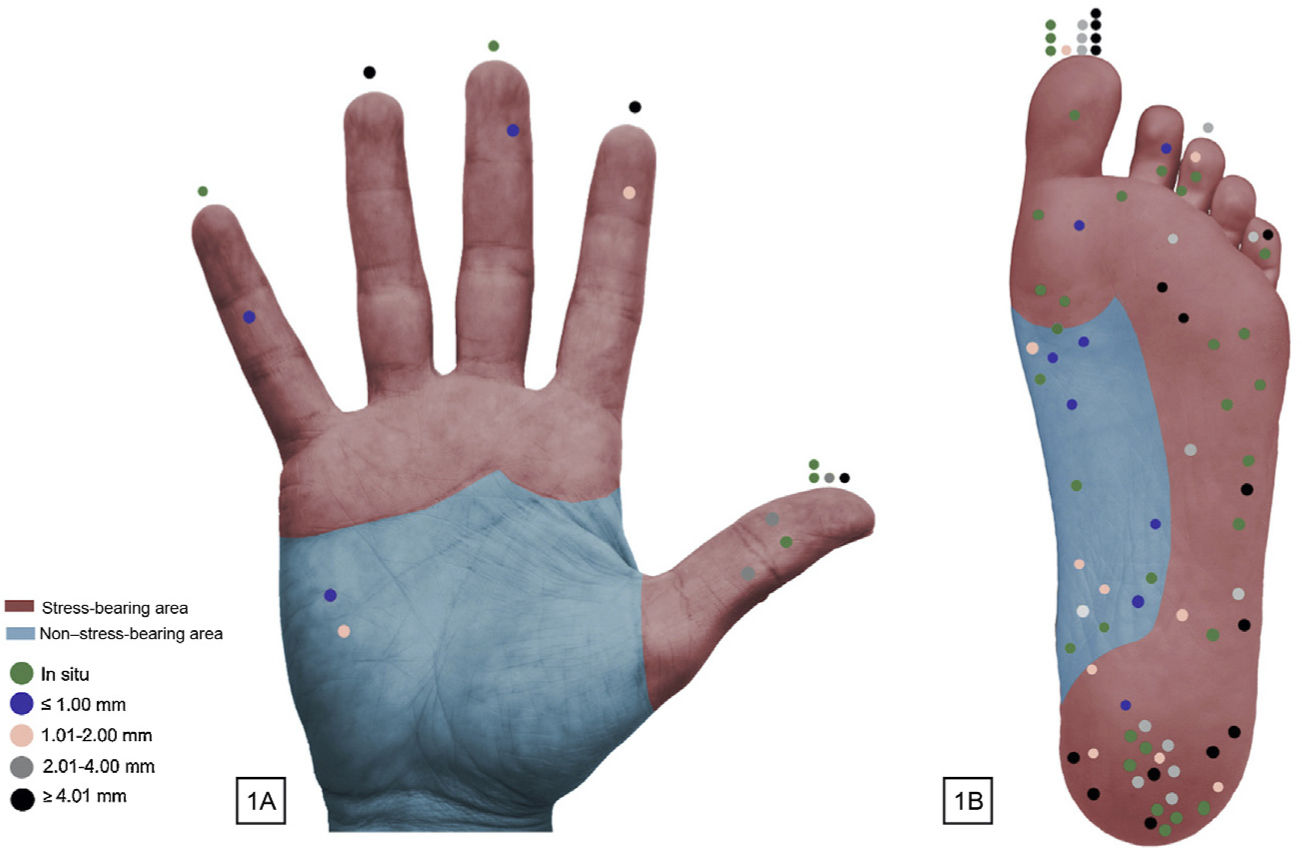
The dependent variable was location, according to whether or not it was subject to stress forces (Fig. 1). On the volar surface of the hand, stress-bearing areas were considered to be the pressure areas of the fingers and the head of the metacarpals, as those are the areas subject to the most mechanical stress with grip and where most lesions, such as calluses and blisters tend to present.8,11,12 By expert consensus, the rest of the palm was classified as a non–stress-bearing area. The nails were analyzed separately. On the plantar surface, depending on the degree of mechanical stress, the plantar surface of the toes, the forefoot, lateral midfoot, and the heel were classified as stress-bearing areas. The plantar arch was defined as a non–stress-bearing area. The nails were analyzed separately.
The following independent variables were taken into consideration. With regard to tumor characteristics, we evaluated location, laterality (right, left), histopathology data including tumor depth (Breslow: recorded as an ordinal qualitative variable with thickness intervals of T0-T4), and ulceration. We also evaluated metastatic lymph-node involvement and the tumor was classified according to the staging system proposed by the American Joint Committee on Cancer (AJCC), eighth edition.13
Categorical variables were reported using absolute and relative frequency distribution and quantitative variables were reported using measures of central tendency and dispersion. The association between independent qualitative variables and the dependent variable was evaluated using the χ2 test or Fisher’s exact test when the expected frequency was less than 5%. Statistical analysis was performed using the SPSS version 21 statistical package (IBM Corp., Armonk, NY, USA). Statistical significance was established for P < .05.
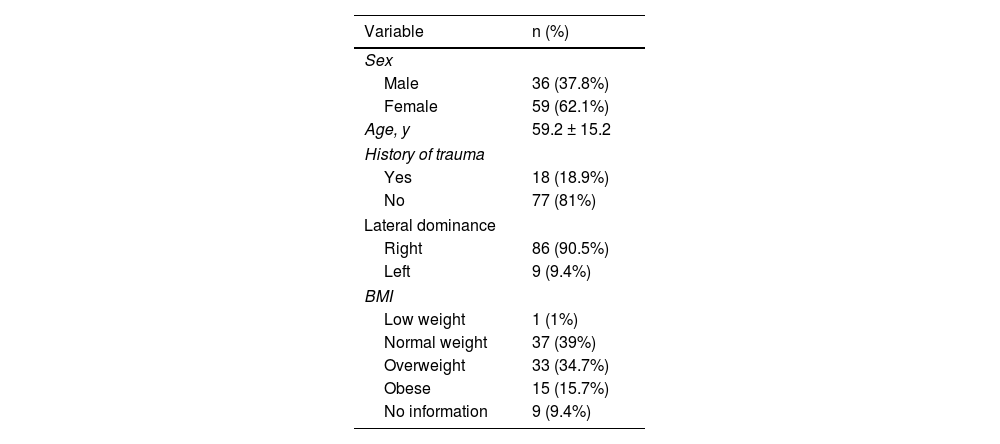
ResultsNinety-five patients with ALM were enrolled (Fig. 2), with median age (interquartile range [IQR]) of 59 years (50-70 years); of these patients, 59 (62.1%) were female. Prior direct trauma to the area where the melanoma presented was reported in 18 cases (18.9%) (Table 1).
Characteristics of Study Patients.
| Variable | n (%) |
|---|---|
| Sex | |
| Male | 36 (37.8%) |
| Female | 59 (62.1%) |
| Age, y | 59.2 ± 15.2 |
| History of trauma | |
| Yes | 18 (18.9%) |
| No | 77 (81%) |
| Lateral dominance | |
| Right | 86 (90.5%) |
| Left | 9 (9.4%) |
| BMI | |
| Low weight | 1 (1%) |
| Normal weight | 37 (39%) |
| Overweight | 33 (34.7%) |
| Obese | 15 (15.7%) |
| No information | 9 (9.4%) |
Abbreviations: BMI indicates body mass index.
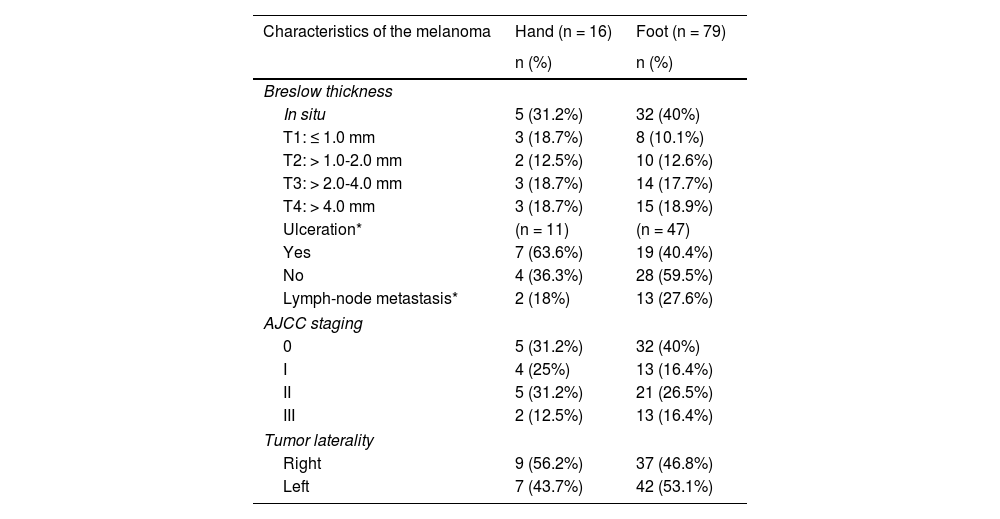
Of the lesions evaluated, 16 (16.8%) presented on the hands and 79 (83.1%) on the feet. Although a slight predominance of the right side was observed for tumors on the hand (56.2% right vs. 43.7% left), on the feet, more acral were observed on the left side (53.1% left vs. 46.8% right). Most of the lesions were in situ (37 [38.9%]) (Table 2).
Clinical Characteristics ALM Analyzed.
| Characteristics of the melanoma | Hand (n = 16) | Foot (n = 79) |
|---|---|---|
| n (%) | n (%) | |
| Breslow thickness | ||
| In situ | 5 (31.2%) | 32 (40%) |
| T1: ≤ 1.0 mm | 3 (18.7%) | 8 (10.1%) |
| T2: > 1.0-2.0 mm | 2 (12.5%) | 10 (12.6%) |
| T3: > 2.0-4.0 mm | 3 (18.7%) | 14 (17.7%) |
| T4: > 4.0 mm | 3 (18.7%) | 15 (18.9%) |
| Ulceration* | (n = 11) | (n = 47) |
| Yes | 7 (63.6%) | 19 (40.4%) |
| No | 4 (36.3%) | 28 (59.5%) |
| Lymph-node metastasis* | 2 (18%) | 13 (27.6%) |
| AJCC staging | ||
| 0 | 5 (31.2%) | 32 (40%) |
| I | 4 (25%) | 13 (16.4%) |
| II | 5 (31.2%) | 21 (26.5%) |
| III | 2 (12.5%) | 13 (16.4%) |
| Tumor laterality | ||
| Right | 9 (56.2%) | 37 (46.8%) |
| Left | 7 (43.7%) | 42 (53.1%) |
Abbreviations: AJCC indicates American Joint Committee on Cancer.
Of the 16 melanomas on the hand, half were located on the nails, 6 (37.5%) in the stress-bearing area, and 2 (12.5%) in the non–stress-bearing area (Fig. 1A). Of the 79 melanomas on the foot, the stress-bearing area was the most affected, with 52 cases (65.8%), in which the heel was the location with the greatest number of melanomas. A total of 15 of the lesions (18.9%) presented in the non–stress-bearing area and 12 (15.1%) on the nails (Fig. 1B).
A history of direct trauma to the area where the melanoma presented was more frequent in patients with lesions on the nails. The invasive melanomas had a higher Breslow thickness and a higher presence of ulceration in the stress-bearing areas and on the nails than in the non–stress-bearing areas (P = .006 and P = .018, respectively). The distribution pattern of the melanoma was not associated with the other variables evaluated (Table 3).
Association Between Tumor Characteristics and Location.
| Parameter | Stress-bearing area (n = 58, 61%) | Non–stress-bearing area (n = 17, 17.8%) | Nail (n = 20, 21%) | Total (n = 95, 100%) | P |
|---|---|---|---|---|---|
| Sex | .728 | ||||
| Female | 35 (60.3%) | 12 (70.6%) | 12 (60%) | 59 (62.1%) | |
| Male | 23 (39.7%) | 5 (29.4%) | 8 (40%) | 36 (37.9%) | |
| BMI | .345 | ||||
| Low | 0 | 1 (5.9%) | 0 | 1 (1%) | |
| Normal | 20 (34.4%) | 9 (52.9%) | 8 (40%) | 37 (38.9%) | |
| Overweight | 24 (41.4%) | 4 (23.5%) | 5 (25%) | 33 (34.7%) | |
| Obese | 9 (15.5%) | 2 (11.8%) | 4 (20%) | 15 (15.8%) | |
| No information | 5 (8.6%) | 1 (5.9%) | 3 (15%) | 9 (9.5%) | |
| History of trauma | .025 | ||||
| Yes | 8 (13.8%) | 2 (11.8%) | 8 (40%) | 18 (18.9%) | |
| No | 50 (86.2%) | 15 (88.2%) | 12 (60%) | 77 (81.1%) | |
| Breslow thickness | .006 | ||||
| In situ | 24 (41.4%) | 6 (35.3%) | 7 (35%) | 37 (38.9%) | |
| ≤ 1 mm | 5 (8.6%) | 6 (35.3%) | 0 | 11 (11.6%) | |
| > 1.0-2.0 mm | 7 (12.1%) | 4 (23.5%) | 1 (5%) | 12 (12.6%) | |
| > 2.0-4.0 mm | 11 (19%) | 1 (5.9%) | 5 (25%) | 17 (17.9%) | |
| > 4.0 mm | 11 (19%) | 0 | 7 (35%) | 18 (18.9%) | |
| Ulceration* | .018 | ||||
| Yes | 12 (35.3%) | 3 (27.3%) | 10 (76.9%) | 25 (43.1%) | |
| No | 22 (64.7%) | 8 (72.7%) | 3 (23.1%) | 33 (56.9%) | |
| Lymph-node metastasis* | .470 | ||||
| Yes | 8 (23.5%) | 2 (18.2%) | 5 (38.5%) | 15 (25.9%) | |
| No | 26 (76.5%) | 9 (81.8%) | 8 (61.5%) | 43 (74.1%) | |
| Stage | .128 | ||||
| 0 | 24 (41.4%) | 6 (35.3%) | 7 (35%) | 37 (38.9%) | |
| I | 11 (19%) | 6 (35.3%) | 0 | 17 (17.9%) | |
| II | 15 (25.9%) | 3 (17.6%) | 8 (40%) | 26 (27.4%) | |
| III | 8 (13.8%) | 2 (11.8%) | 5 (25%) | 15 (15.8%) |
Abbreviations: BMI indicates body mass index.
ALM differs from melanomas in other locations by its presentation and associated risk factors.5,14 In our study, we analyzed the clinical and pathologic characteristics of ALM in 95 patients, taking into account the location of the tumors. Our analysis shows that, both on the hand and the foot, ALM is more frequent in areas subject to greater stress, which are also associated with greater tumor depth in comparison with non–stress-bearing areas. A history of direct trauma to the area where the melanoma presented was more frequent in patients with lesions on the nails, which was also the area with more frequent ulceration.
The mean age of the patients in the study was lower than that described in some Asian6,15,16 and Latin American countries.17,18 The ratio of male to female was 1:1.6, which is comparable to data from other authors,1,18,19 and unlike the study by Duarte20 in Colombia, more cases of ALM were recorded in men than in women.
The etiology of ALM continues to be unclear. Because of its location, the acral surface of the body suffers the least damage from sunlight. Indeed, one study has shown that acral melanomas have different genetic characteristics, with a lower frequency of alternations induced by UV light.21
It is also important to note that the palms and soles are more hypopigmented areas compared to other areas of the body, including in darker phenotypes. This may play a role in the cause of melanomas on volar skin because, as mentioned by Saida,22 melanin is known to act by blocking the production of free radicals.
It has also been suggested that the acral areas are subject to greater mechanical stress, especially in the front and rear of the foot, which may lead to greater damage to the skin in these areas, thus favoring the development of melanoma.5,6 Indeed, the literature reports that most acral melanomas are located on the sole of the foot,1,23,24 which may be explained by the greater mechanical stress that occurs in this region, in comparison with the palm of the hand.8 In line with these data, most of the tumors in our series were located on the feet. Nevertheless, some studies have reported that subungular melanomas present with greater frequency on the fingers than on the toes,1,25 unlike in our study, where subungular melanomas were also more frequent on the foot, principally the big toe. The thumb nail was also the most frequently affected on the hand (data not shown in tables), which is in line with the information reported to date.15,26 Möhrle and Häfner27 suggest that acute or chronic trauma may be associated with the pathogenesis of acral melanoma, as the thumb and big toe are the digits most commonly affected by trauma and are those that most frequently present melanoma.
In our patients, the percentage with a history of prior direct trauma at the site of the tumor was greater than that published in other studies.15,25 Similar to that reported by Holman,28 we found that a history of trauma was more frequent in lesions of the nails than lesion in other acral areas.
We found that ALM presented more frequently in stress-bearing areas of the feet, mainly on the heel, which is in line with the information published in different populations.6,16,29 In a study performed at the Mayo Clinic, no significant differences were found between the distribution of the acral lesions, by stress-bearing and non–stress-bearing area. However, the study found that approximately half of patients with melanomas on the arch of the foot were obese, which may be associated with flattening of the plantar arch. The authors therefore excluded these cases from the analysis and found a reduction in the P value (P = .39 vs. P = .11), although without reaching statistical significance.30 Our study found no association between BMI and tumor location, unlike Costello et al,30 who assume that obese patients (BMI > 30) present flattening and subsequent loss of the plantar arch. Our study did not determine this outcome and it was not therefore possible to reach this conclusion.
Nishiguchi et al8 evaluated the difference in distribution between nevus and melanoma of the palm and fingers and found that nevus presents on the area proximal to the distal transversal fold of the palm, whereas melanoma presents on the pads and distal to the transversal distal arch of the palm—areas associated with greater mechanical stress. In our study, melanoma of the hand also presented predominantly on the volar surface of the fingers and on the nails. Only 2 cases were found on the hypothenar eminence. These findings support the fact that it is useful to use location to guide a suspected diagnosis of malignancy when the lesion presents in the more distal areas, especially on the digits and nails. Nevertheless, the fact that the lesion presents in a non–stress-bearing or more proximal area cannot rule out a diagnosis of melanoma, as shown in our study.
Given that the behavior of melanomas on the nails has been reported to be different in some respects in comparison to other acral melanomas,25,28 in our study, we analyzed subungual melanomas separately and found that invasive melanomas tended to present greater tumor depth, greater presence of ulceration, and a higher percentage of metastasis in the lymph nodes compared to other acral locations. This was in contrast to the study by Moon et al,31 who found that the nails presented less ulceration than lesions on the digits, palms, and soles.
In terms of the histopathologic characteristics of the tumor, in our series, most of the lesions, on both hands and feet, were in situ, unlike the studies by Barrera Jácome et al18 and Costello et al,30 in which cases of noninvasive acral melanoma correspond to low rates of 8.3%. Among invasive melanoma, we found that the highest percentage presented a Breslow thickness of greater than 4 mm, comparable with that reported in populations such as Korea25 but higher than that found in the US23,30 and Taiwan.6
Unlike studies published by other authors, who found no link between tumor location and Breslow thickness or the presence of ulceration,6,25,30 our study did find a significant difference between the presence of ulceration, Breslow thickness, and a history of trauma when comparing melanomas located in stress-bearing areas, non–stress-bearing areas, and the nails. It is interesting to see how the percentage among invasive melanomas increased as the Breslow thickness increased in lesions located in stress-bearing areas, unlike non–stress-bearing areas, where the percentage of lesions decreased as depth increased. No association was found, however, between location of ALM and sex, BMI, metastasis in lymph nodes, or tumor stage.
The limitations of our study include the fact that some data were obtained from secondary sources. The BMI variable was calculated based on the weight of the patient at the time of the telephone survey, as the clinical records did not contain weight and height at the time of diagnosis; patients may, therefore, have had different body weight at the time the melanoma was diagnosed. Moreover, the number of lesions on the hand was low and it was difficult to classify the palm into stress-bearing and non–stress-bearing areas, as this may be affected by the activity carried out by the patient, which makes it hard to derive conclusions regarding the melanomas located in this area. As the cases were recent, it was not possible to evaluate survival at 5 years in these patients, data that would make an interesting comparison with other populations.
The findings of our study show that the acral areas considered stress-bearing areas and those with greater predisposition to direct trauma, such as the nail of the big toe and the thumb are associated with ALM, which also suggests that both acute and chronic stress may be associated with developing this subtype of melanoma. Although in our study, location of the lesion was associated significantly with the Breslow thickness, no link was found with tumor stage, which may indicate that location does not affect outcome in these patients. Nevertheless, studies are required that include a greater number of cases, especially on the hand, to analyze the differences between location and survival in these patients. It is also important to investigate the work performed by the patients, which may involve greater mechanical stress in the acral areas, in order to link those activities with ALM.
In conclusion, the predominant location of ALM in stress-bearing areas, consistent with the findings of other studies, supports the hypothesis that mechanical stress may play a role in the pathogenesis of this type of tumor.
FundingThis study has not received funding of any kind.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors would like to thank Dr. Sergio Lozano Gómez and María Adelaida Piedrahita.
Please cite this article as: Arango Abisaad J, Arciniegas Grisales V, Londoño García Á, Vasquez Trespalacios EM, Jiménez Calfat G, Cuello López JM. Características del melanoma lentiginoso acral según su relación con la presión. Estudio retrospectivo de 95 pacientes. Actas Dermosifiliogr. 2022;113:134–140.