Chronic hand and foot eczema (CHFE) is a recurrent inflammatory condition that affects quality of life, particularly in patients with moderate-to-severe atopic dermatitis (AD). Its impact is due to pruritus, pain, xerosis, and fissures, which impair daily and occupational activities. Constant exposure to mechanical, chemical, and environmental factors contributes to its chronicity and makes treatment challenging.
Hand eczema is one of the most common inflammatory skin diseases, with an annual prevalence of 5–10%.1–3 Up to one-third of patients do not seek medical care, underestimating its true burden. In patients with AD, palmoplantar involvement is common and often resistant to conventional therapies, increasing clinical and emotional distress.
Managing CHFE in AD is challenging, as topical and systemic treatments have limitations in both efficacy and safety. Treatment adherence may also be affected by the need for frequent applications or by adverse effects associated with immunosuppressants.
Biologic therapies have changed the treatment paradigm. Tralokinumab, a monoclonal antibody that blocks interleukin-13 (IL-13), has shown efficacy in generalized AD, but its effect on palmoplantar involvement has been scarcely studied. This retrospective study aims to evaluate its safety and efficacy profile in patients with moderate-to-severe AD, identify predictors of response, and assess its impact on quality of life, optimizing therapeutic strategies.
We conducted a retrospective, observational, multicenter study in four hospitals in Andalusia (Spain): Virgen del Rocío (Sevilla), Universitario San Cecilio (Granada), Reina Sofía (Córdoba), and Puerto Real (Cádiz). The health records of patients treated with tralokinumab for moderate-to-severe AD with palmoplantar involvement from April 2022 through January 2024 were reviewed.
Adult patients (≥18 years) diagnosed with moderate-to-severe AD according to the UK Working Party criteria4 and documented hand and foot involvement were included. Those with concomitant skin diseases or incomplete records were excluded.
Variables analyzed included demographic data (age, sex, weight, BMI, smoking status) and clinical effectiveness parameters: Eczema Area and Severity Index (EASI), Numeric Rating Scale for Pruritus (NRS), and Physician Global Assessment (PGA). Measurements were recorded at three time points: baseline, week 16, and week 52.
Statistical analysis was performed using GraphPad Prism v.9.2 with paired t tests and ANOVA for comparisons. P values <0.05 were considered statistically significant. The study was conducted in full compliance with the ethical principles outlined in the Declaration of Helsinki and approved by Hospital Universitario San Cecilio Ethics Committee (Granada) under reference code HUSC_DERM_2023_08.
The study included a total of 21 patients, of whom 38.1% were women and 61.9% men, with a mean age of 33.47±10.87 years (Table 1). The mean BMI was 25.27±5.34, and 23.8% were smokers. All patients had previously received cyclosporine; 38.1% had been treated with azathioprine, 23.8% with methotrexate, and 14.3% with mycophenolate mofetil. Nineteen percent had undergone phototherapy. Before entering the study, 38.1% had experienced therapeutic failure with dupilumab.
Baseline characteristics of the study population with AD involving hands and feet.
| Baseline characteristics (n=21) | Value |
|---|---|
| Sex, n (%) | |
| Male | 13 (61.9%) |
| Female | 8 (38.1%) |
| Mean age (range) | 33.47 (24–71) |
| BMI (SD) | 25.27 (5.34) |
| Mean EASI (SD) | 23.60 (4.44) |
| PGA-hands (SD) | 2.52 (0.87) |
| PGA-feet (SD)* | 2.00 (0.50) |
| NRS pruritus (SD) | 9.24 (0.54) |
| Previous treatments, n (%) | |
| Cyclosporine | 21 (100%) |
| Azathioprine | 8 (38.1%) |
| Dupilumab | 8 (38.1%) |
| Methotrexate | 5 (23.8%) |
| Phototherapy | 4 (19%) |
| Mycophenolate mofetil | 3 (14.3%) |
| Smoking habit, n (%) | 5 (23.8%) |
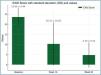
At baseline, the mean EASI score was 23.60±4.44 (Fig. 1), reflecting severe disease. The PGA indicated moderate-to-severe involvement of the hands (2.52±0.87) and feet (2±0.5) (Fig. 2). At week 16, 76.19% of patients showed improvement in hand PGA, increasing to 81.2% at week 52. For foot PGA, improvement rates were 66.6% and 71.4%, respectively.
Both EASI and NRS-pruritus improved significantly, with EASI scores dropping from 23.60±4.44 down to 10.31±10.65 at week 16 and to 4.76±6.24 at week 52. No significant differences were found based on baseline characteristics. Four patients (19.05%) discontinued treatment due to lack of efficacy; no serious adverse effects were reported.
Chronic hand eczema (CHE) is a common condition that impacts both quality of life and occupational function. Current clinical practice guidelines recommend a comprehensive strategy involving trigger avoidance, emollients, topical corticosteroids, and systemic therapy in severe cases.5 The Investigator's Global Assessment for Chronic Hand Eczema (IGA-CHE) has proven to be an effective tool for assessing severity, outperforming the HECSI in certain key aspects. It allows for a rapid and comprehensive evaluation based on clinical parameters such as erythema, scaling, and fissuring, facilitating treatment monitoring. Silverberg et al. confirmed its psychometric validity, reliability, and sensitivity to clinically significant change, which supported its use in our study.6
Among the novel therapies currently used for AD management, dupilumab has the strongest evidence for use in CHE. Riva et al.7 conducted a systematic review and meta-analysis including 374 patients, showing partial or complete resolution of CHE in 80.3% of treated patients within 4–16 weeks. In this regard, we previously published a multicenter retrospective study including 84 patients with moderate-to-severe AD and palmoplantar involvement, demonstrating significant improvements in eczema severity and patient quality of life. At week 16, 83.55% of patients achieved improvement in EASI, with pruritus reduced in 73.01% of cases.8
JAK inhibitors such as baricitinib and upadacitinib have shown rapid responses in refractory CHE.9 Abrocitinib has also demonstrated HECSI reduction at 28 weeks, although treatment discontinuations due to adverse effects were reported.10
Tralokinumab demonstrated sustained efficacy in our study, with progressive improvement up to week 52. Despite its limitations, these findings support its favorable safety profile and therapeutic relevance in CHFE, highlighting the need for further research.
Conflicts of interestThe authors declare no conflicts of interest.




 Artículo disponible en español
Artículo disponible en español