Even after the Nuremberg code was published, research on syphilis often continued to fall far short of ethical standards. We review post-World War II research on this disease, focusing on the work carried out in Guatemala and Tuskegee. Over a thousand adults were deliberately inoculated with infectious material for syphilis, chancroid, and gonorrhea between 1946 and 1948 in Guatemala, and thousands of serologies were performed in individuals belonging to indigenous populations or sheltered in orphanages. The Tuskegee syphilis study, conducted by the US Public Health Service, took place between 1932 and 1972 with the aim of following the natural history of the disease when left untreated. The subjects belonged to a rural black population and the study was not halted when effective treatment for syphilis became available in 1945.
Incluso después de la promulgación del código de Nuremberg las investigaciones sobre sífilis continuaron alejándose en muchas ocasiones de los estándares éticos. En este artículo hemos revisado las investigaciones que sobre esta enfermedad tuvieron lugar después de la Segunda Guerra Mundial, centrándonos en los casos de Guatemala y de Tuskegee. En Guatemala durante los años 1946 a 1948 se inoculó deliberadamente a más de 1.000 adultos sífilis, chancroide y gonorrea, y se hicieron miles de serologías a poblaciones indígenas o a niños huérfanos. El experimento Tuskegee sobre sífilis fue realizado entre 1932 y 1972 por el Servicio Público de Salud de los Estados Unidos para estudiar la evolución natural de esta enfermedad en ausencia de tratamiento. Se realizó sobre un grupo de población rural de raza negra y no se interrumpió a pesar de la introducción de tratamientos eficaces para la resolución de la enfermedad durante estos años (1945).
A 2010 article in Nature drew attention to a recent discovery by Susan Reverby that doctors connected with official US public health agencies conducted syphilis experiments in Guatemala from 1946 through 1948; the research was done with the cooperation of the Guatemalan government and the assistance of local physicians.1 The information Reverby found showed that over a thousand individuals (soldiers, prisoners, psychiatric patients, and prostitutes) had been subjected to experiments for more than 2 years. During that time, 1308 adults were inoculated with syphilis, chancroid, and gonorrhea or were exposed to infected prostitutes as part of a plan to pass infections on to prisoners and soldiers.2
The Origin of the Guatemalan ExperimentsEven though researchers had shown in 1943 that penicillin was effective against syphilis and gonorrhea, there remained doubts about how the disease could be prevented and treated. Sexually transmitted diseases were recognized to be a first-order threat to the health of servicemen during World War II. Postcoital urethral lavage with a silver solution to prevent gonorrhea and genital application of a cream to prevent syphilis were methods that had been in use for decades, but they were troublesome, painful, and of slight effect.3
In the United States, doctors under the direction of John C. Cutler had begun experimenting on US prisoners,4 and after some preliminary studies they developed a more ambitious plan to expose healthy subjects to infection by prostitutes. This would be a study they knew could not be done in the United States, however, as public opinion would not have tolerated it if it came to light. In 1945, Juan Funes, a Guatemalan military doctor who had worked at the Venereal Disease Research Laboratory (VDRL) at an American prison for a year, offered to help them carry out the studies in Guatemala.5
Individuals and Groups Responsible for the ExperimentsThe US officials involved in designing and carrying out the study were affiliated with the VDRL, which operated under the US Public Health Service (USPHS), an entity that later became the Center for Disease Control and Prevention (known as the CDC). They worked in collaboration with Guatemalan researchers6 and the Pan-American Sanitary Bureau (PASB), the predecessor of the Pan American Health Organization. Cutler was in charge. Under him were 2 other doctors: Robert C. Arnold and John F. Mahoney, who were also affiliated with the VDRL and the USPHS. In Guatemala they had the help of Juan Funes, chief of the Division for Control of Venereal Diseases, which operated under the Guatemalan public health office. Staff at the Ministry of Health and other government departments were also involved, along with military personnel.
Sites Where the Experiments Were Carried OutWhy was Guatemala chosen? One factor influencing the decision was that prostitution was legal in the country and its prisons. Everything related to prostitution, contagion, and the treatment of infected patients was the responsibility of the Division for Control of Venereal Diseases, headed by Funes, who was among the investigators. An agreement was drawn up stating that once the PASB's interest in the project ended, the equipment and laboratories set up in Guatemala would be transferred to the government, becoming public facilities operated by local staff.
Experimentation began in the Guatemalan prisons. Contact with infected prostitutes proved to be an unreliable means of inoculation, however. Furthermore, follow-up serology data were incomplete because the prisoners objected to periodic extractions.
The study design was therefore revised so that experiments could target a different population: patients residing at a public mental health facility (Hospital Nacional de Salud Mental). The mental condition of these patients meant that they offered no resistance,7 and since the government facility had evident deficits, the US researchers were able to obtain institutional cooperation by promising needed material and offering patients cigarettes as compensation for their cooperation.8,9
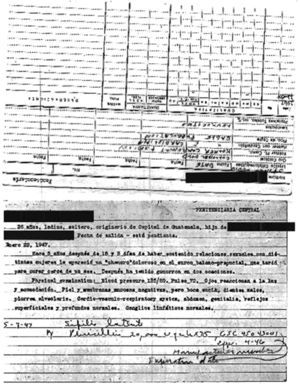
The Experimental DesignCutler arrived in Guatemala in 1946 to begin experiments that included serology and tests to confirm the true efficacy of penicillin in clinical use and evaluate the various preventive strategies10–12 (Fig. 1).
The USPHS was interested in studying so-called normal exposure. Their initial attempt at using infected prostitutes to spread gonorrhea among the soldiers and prisoners required them to first inoculate the prostitutes with germs cultured in rabbits. Statistics at the time assumed that a single prostitute could have sex with 8soldiers in 71minutes, so the potential for contagion was, in theory, enormous.13
Cutler found it was difficult to introduce infection by these naturalistic methods, however, so it was decided to resort to direct inoculation. The site of this attempt would be the Guatemalan government's mental health facility, where patients would be acquiescent. The researchers abraded the subject's penis to increase the likelihood of infection, and they injected syphilis into the spinal fluid of some.13 The bacteria they used came from other patients who were already infected or from “street strains.”14 The consent of patients or their families was, of course, never obtained. Permission was only asked of the military officers in command or administrators and doctors at the facility.15 Deaths occurred during the experiments on the psychiatric patients, but were attributed to the high rate of underlying disease.
The study ended in 1948, although some follow-up laboratory testing and other procedures, such as tissue sampling and autopsies, went on for years. Autopsies of patients on whom the experiments had been done were being practiced even as late as 1958. The study was never covered up: results were presented at the the Second Central American Venereology Conference in Guatemala City in April 1948, for example, and some were published in the journal Salubridad y Asistencia an organ of the Ministry of Public Health and Social Services (see volume II, the issue for April 4–7, 1949).9,13
Performing serologies was one of the hurdles the experimenters faced. Techniques that had been recently described were available, and studies were done in a broad spectrum of the Guatemalan population, in orphanages, and in leprosy hospitals.16 A training course given by the US scientists for their Central American colleagues was attended by participants from Guatemala, El Salvador, Costa Rica, and Panama. In the summer of 1949, all the course participants were asked to provide the trainers with blood samples from patients, and the response was very positive: 1073 were sent from Guatemala, 1007 from El Salvador, 1295 from Costa Rica, and 1899 from Panama.13
The Experiments EndThe material documenting the Guatemalan experiments, which are part of the John C. Cutler papers deposited at the University of Pittsburgh, were recently released for examination. The papers include extensive summaries describing the syphilis experiments and briefer notes about gonorrhea and chancroid studies, as well as correspondence, records, and the patients’ clinical data.17
The work in Guatemala was halted in 1948 for reasons left unclear, and it was not brought to light until Reverby's chance discovery in 2010. Once the documents were made public, they were analyzed by various investigative commissions and a fairly credible account could be reconstructed to clarify what happened and when. The physicians had taken advantage of their position to experiment with vulnerable members of society, who in this case were the mentally ill, members of indigenous groups, men who had enlisted in the military, and prostitutes.18
The Tuskegee Syphilis StudyIn 1997, then US President William J. Clinton apologized for the Tuskegee experiment, a long-running, nontherapeutic study of the natural history of syphilis. Several hundred African American men who lived in an area of Alabama were denied access to proper treatment over the course of the study.19–22 According to one commentary on the president's words, it was clear that the project had “come to symbolize racism in medicine, misconduct in human research, the arrogance of physicians, and government abuse of Black people”.23
The Tuskegee experiment, also known as the “Tuskegee study of untreated syphilis in the Negro male,” was carried out between 1932 and 1972 by the USPHS with the purpose of observing the natural course of the disease when left untreated. The subjects came from a poor, rural African American population and the study was not halted even when an effective, curative treatment (penicillin) became available around 1945.
The USPHS, in collaboration with the Tuskegee Institute, initiated the study in 1932 and it continued under different directors until 1972.24 Over that long span of 40 years, many subjects died from syphilis and children were born with the congenital form while the researchers observed with therapeutic indifference and kept the experiment running. The Tuskegee syphilis experiment has been widely scrutinized,25,26 it has been described as “arguably the most infamous biomedical research study in US history,26” it led directly to the Belmont report on bioethics,27 and it has continued to draw criticism in the years since its closure.
Background and Initial Planning of the StudyIn the first third of the 20th century the medical literature often contained the claim that syphilis tended to have greater impact on the nervous system in Caucasian populations, whereas the cardiovascular system was more vulnerable in persons of black African descent. However in a study of hundreds of untreated cases in white men in Oslo, published by E. Bruusgard in 1928, the authors found the rate of cardiovascular involvement to be higher and they uncovered very few cases of neurosyphilis.28,29 A similar prospective study was then planned in the United States. It was to be carried out in an area of Alabama with a high prevalence of syphilis, where 35% to 40% of the population was seropositive. Taliaferro Clark seems to have proposed the idea of observing untreated syphilis for 6 to 8 months, after which the patients would be treated with the standard resources of the day, including Salvarsan30 and bismuth.31 This once common regimen was effective, although it was also fairly toxic.
The researchers enrolled 600 African American men in Macon County, Alabama (Fig. 2); 399 of them had previously contracted syphilis and 201 were healthy controls. The participants were largely illiterate and they were offered free medical care, a meal every day, and a $50 burial policy for funeral expenses. The men were not told they had syphilis, nor were they treated. The cost of their health care was covered by the Julius Rosenwald Fund32 until events related to the crash of 1929 forced the fund to withdraw support.
A Long-Running Study in Human Guinea PigsThe Tuskegee study kept going, however; it seems that some researchers wished to have a longer period of observation. Dr. Clark disagreed with the change of plan and withdrew the same year his study had commenced.
The subjects were never properly informed, but the researchers also resorted to deception to win cooperation. To ensure the men would come for spinal taps, one of the supervisors, Raymond A. Vonderlehr, sent each man an untruthful letter with the phrase “Remember This Is Your Last Chance For Special Free Treatment.” Furthermore, permission for autopy was obtained by making the burial policy contingent upon agreeing to it. The researchers were obsessed with obtaining data for science above any ethical considerations.33 The study was never kept secret: a great deal of information and many articles were published while it was under way.33–37
Development of Nontreponemal TestsThe greatest contribution connected with Tuskegee was the development and standardization of diagnostic serum tests for syphilis. Publications began to appear in 193438 and 1935.39 When the first study comparing treated and untreated men with syphilis was published a year later, nontreponemal diagnostic tests were already in use.40 The 1936 paper specifically emphasized the incidence of cardiovascular involvement in the Tuskegee population. Starting in 1942, the USPHS used sera from Tuskegee to develop the VDRL test.41
The Tuskegee techniques were instrumental in establishing the USPHS's position in international health organizations. Research on serologic techniques and the lucrative commercialization of diagnostic tests allowed the service to occupy a place beside German research programs, which had pioneered this field, and to occupy a respected position in the World Health Organization.
Introduction of Penicillin in the Treatment of SyphilisFleming's initial discovery of penicillin had been made in 1928, and American military doctors were already using it to treat servicemen for syphilis in the Pacific in 1943.42 Penicillin was evidently effective, and by 1947 it had become the gold standard treatment for the disease. This new drug was so successful that by the mid-1950s the incidence of syphilis had plummeted and many believed it might be eradicated entirely.43 The Tuskegee experiment nonetheless pushed on. The subjects enrolled were neither given penicillin nor told of this treatment so that the researchers could continue to watch how the disease progressed and killed. Treatment was deliberately denied to many and they were also specifically warned to avoid taking penicillin.
Even as the US government sponsored public health campaigns that aimed at eradicating syphilis, the Tuskegee men were carefully shielded from information. During World War II, 250 men drafted into the armed forces were diagnosed. Their military doctors recommended treatment, but by order of the USPHS, the recommendations never reached the men. In 1951, public health authorities still insisted that the Tuskegee experiment constituted a “unique opportunity”29 (p. 179).
The Development of Research Ethics GuidelinesThe Nuremberg Code of 1947, the Catholic Church's position expressed by Pope Pius XII in 1952, and the Declaration of Helsinki of 1964 all insisted that researchers must hold the well-being of the individual before any interests of medical experimentation, that participation in research must be voluntary, and that subjects must be fully informed before consent can be given.44 None of these voices deterred the Tuskegee researchers, who pushed on relentlessly, unaffected by all ethical decrees and the maturing conscience of both science and society with respect to moral issues.
The Study EndsWhen the lay press focused attention on Tuskegee in 1972, the authorities were finally moved to close down the Tuskegee experiment. Voices had begun to warn of unethical practices in the study, which was now in its final phase. The CDC reiterated its position that work should continue until all the patients had passed on so that autopsies could be performed.
It was Peter Buxtun (sometimes Buxton) who first approached the press with concerns about Tuskegee in the early 1970s; the story was published in The Washington Star on July 25, 1972, and a day later it made the front page of The New York Times. The scandal moved Senator Edward Kennedy to organize Congressional hearings. Strong public protest followed and an advisory group determined that the study was medically unjustified and ordered it shut down. The Tuskegee experiment had lasted 40 years and only 74 men were still alive. Twenty-eight of the 399 subjects had already died of syphilis and 100 had died of complications. Forty women, partners of men in the study, had been infected and 19 children had been born with congenital syphilis.
Conclusions and Reflections on Research EthicsFor centuries syphilis was singled out for special attention from researchers because of its means of contagion, its clinical course, and the ineffectiveness of treatments.
In the light of our current views of research ethics, we are repulsed by aspects of some of the experiments carried out in the past, even if we remember that those living in any period of history are working within a particular frame of reference. The views and behaviors of human beings are formed by social, cultural, hierarchical, biological, and anthropological factors that come together to provide such frames of reference, which will change over the course of history and from culture to culture.45
Progress has undoubtedly been made through the development of explicit codes of research ethics and follow-up legislation to regulate it. Unfortunately, such codes have always emerged only after civil society has reacted to abhorrent research practices, such as those of the Nazis in concentration camps or the experiments carried out in populations at risk of exploitation (prisoners, patients, prostitutes, indigenous peoples). Groups that must be considered particularly vulnerable by researchers designing experiments are women, especially if pregnant46; ethnic minorities47; the poor48; the disabled49; children50; and prisoners, soldiers, or students.51
Yet in spite of international law and ethics guidelines, researchers continue to propose questionable experiments involving human subjects. It is important for us to be aware of historical events in order to avoid repeating the mistakes of our past. Many dermatologists and scientists who conducted experiments that seem terrible to us today were convinced they were serving science and the common good, but they also took advantage of their position for personal gain of a professional, scientific, or financial nature.
The experiments on syphilis provide us with suitable examples for study, showing why we must insist on educating physicians on the values we all hold dear.
Ethical DisclosuresProtection of human and animal subjectsThe authors state that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their hospitals concerning the publication of patient data and that all the patients included in this study were appropriately informed and gave their written informed consent.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Cuerda-Galindo E, Sierra-Valenti X, González-López E, López-Muñoz F. La sífilis y la experimentación en humanos: perspectiva histórica y reflexiones éticas. De la Segunda Guerra Mundial a la actualidad. Actas Dermosifiliogr. 2014;105:847–853.