There are no clinical guidelines on the management of dysplastic nevus (DN). The aims of this study were to determine the percentage of dermatologists in the center-Spain section of the Spanish Academy of Dermatology and Venereology (AEDV) who would manage a histologically confirmed DN with a watch-and-wait approach or with wider surgical margins and to investigate whether their attitudes would vary depending on whether or not the patient had a personal and/or family history of melanoma.
Material and methodsWe collected data from an anonymous survey sent to 738 dermatologists between June 15 and July 31, 2022. The independent variables were degree of dysplasia (low vs. high), margin status (positive vs. negative), and a personal or family history of melanoma (yes vs. no in both cases). The dependent variables were attitude towards management (watch-and-wait vs. re-excision with a surgical margin of 1 to 4mm or re-excision with a surgical margin of 5 to 10mm).
ResultsWe obtained 86 responses to the questionnaire. When pathology indicated a low-grade DN, 60.5% of dermatologists stated they would obtain a surgical margin of 1 to 4mm if the first margins were positive, and 97.7% would watch and wait if the report described negative margins. For high-grade DNs, 1.2% of dermatologists would watch and wait to manage DN with positive margins; 68.8% would use this approach for negative margins. A family or personal history of melanoma had no influence on most of the dermatologists’ attitudes.
ConclusionsManagement strategies for DN among dermatologists from the center-Spain section of the AEDV varied, particularly when faced with low-grade DN with positive margins and high-grade DN with negative margins. A family or personal history of melanoma did not influence clinical attitudes in most cases.
No existen guías clínicas para el manejo del nevus displásico (ND). Determinaremos el porcentaje de dermatólogos de la sección Centro de la Academia Española de Dermatología y Venereología (AEDV) que ampliarían márgenes o tendrían actitud conservadora en un ND, y si los antecedentes personales (AP) y/o familiares (AF) de melanoma modificarían la actitud tomada frente a un paciente sin antecedentes de interés.
Material y métodosSe difundió la encuesta a 738 dermatólogos y se recogieron datos de forma anónima del 15 de junio de 2022 al 31 de julio de 2022. Las variables de exposición fueron el grado de displasia (bajo/alto), los márgenes (afecto/libre) y los antecedentes de melanoma (sin antecedentes/AF/AP). Las variables dependientes (actitud) incluyeron observación/márgenes de 1-4mm /márgenes 5-10mm.
ResultadosSe recibieron 86 respuestas. Si el patólogo informase bordes afectos en un ND de bajo grado, el 60,5% ampliarían márgenes de 1 a 4mm, mientras que si los márgenes están libres el 97,7%, tendrían una actitud conservadora. Si el patólogo informara bordes afectos en un ND de alto grado, solo el 1,2% tendrían una actitud conservadora, porcentaje que se incrementa notablemente si los márgenes están libres (68,6%). El AF o el AP de melanoma no influirían en la actitud de la mayoría.
ConclusionesEl manejo del ND no es uniforme entre los dermatólogos de la sección centro de la AEDV, especialmente en el caso de ND de bajo grado con bordes afectos y ND de alto grado con bordes libres. El AF o el AP de melanoma no modifican en la mayor parte de los casos la actitud clínica.
Dysplastic nevus (DN) is classified by the World Health Organization (WHO) as a benign condition.1 We were unable to find clinical practice guidelines for DN. The WHO redefined the histopathology criteria for DN in 2018 and recommended classifying dysplasia as low- or high-grade, thus eliminating the former mild grade.1 Several surveys on the management of DN have been published by dermatologists from other countries (USA, Canada, and Australia), all before the 2018 WHO update. These mainly show a considerable difference in the management of DN with severe dysplasia and negative margins, indicating potential differences in the treatment of affected patients.2–7
We were unable to find data in the literature on current management of DN in our setting. Knowledge of management of this condition would be a first step when evaluating the need to draft a consensus document on DN in our area.
Based on data from previous publications and observations from daily clinical practice, our working hypothesis is that there is some disagreement with respect to the clinical management of DN between dermatologists from the center-Spain section of the Spanish Academy of Dermatology and Venereology (AEDV), especially in the case of high-grade dysplasia. The main objective of the present study was to determine the percentage of dermatologists from the center-Spain section of the AEDV who would adopt a watch-and-wait approach (observation only) or who would opt for re-excision on receiving a histopathology report of low- or high-grade DN with positive or negative margins. Our survey did not intend to investigate the management of clinically atypical nevus and only covers the management of melanocytic lesions that were histologically diagnosed as DN. As a secondary objective, we sought to determine whether a personal and/or family history of melanoma would affect the approach to a patient with no history of interest.
Material and MethodsWe performed a cross-sectional descriptive survey. The target population was staff dermatologists and dermatology residents practicing in the center-Spain section of the AEDV (Autonomous Community of Madrid, Castile-La Mancha, and Extremadura). The accessible population comprised all those professionals who were prepared to participate anonymously in the survey. There was no control group. We collected data online between June 15, 2022 and July 31, 2022 (both inclusive) using an online survey from Microsoft Forms. The survey was sent by email to 738 dermatologists of the center-Spain section of the AEDV, and the project was presented at the meeting of this section of the AEDV in June 2022. The minimum sample size for a margin of error of 10% with a 95% CI and a response distribution of 50% was 86. Neither the investigators nor the respondents received financial remuneration for participating in the survey. The independent variables were grade of dysplasia (low vs. high), margins (positive vs. negative), and patient history (none of interest, family history of melanoma, and personal history of melanoma). The dependent variables included observation, margins measuring 1-4mm, and margins measuring 5-10mm. The initial premise in these hypothetical clinical situations was that the melanocytic lesion had been removed using excisional biopsy, and the diagnosis of DN had been confirmed by the reference dermatopathologist at our center, without verification of the sample by a second pathologist. The survey is shown in Annex 1.
The statistical analysis was performed with R, Version 4.1.1. We applied descriptive statistics and tested hypotheses to evaluate the statistical association between the grade of dysplasia and margin status, as well as the approach taken and the respondent's involvement in digital dermoscopy and/or dermatologic-oncology (Fisher exact test). Statistical significance was set at P<.05.
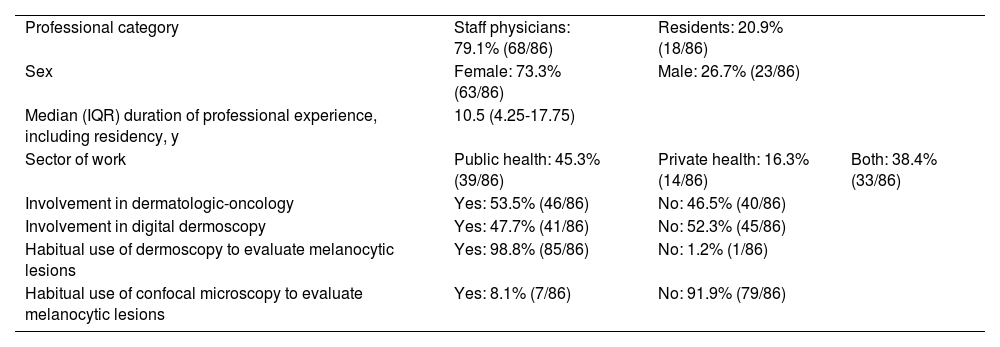
ResultsWe received 86 responses (response rate, 11.7%) (Table 1). Of these, 79.1% were staff physicians and 20.9% residents. Women accounted for 73.3% and men 26.7%, and the median professional experience was 10.5years. Almost half (45.3%) worked exclusively in the public health system. Participation was 53.5% in dermatologic-oncology and 47.7% in digital dermoscopy. Almost all the respondents (98.8%) regularly used dermoscopy to evaluate melanocytic lesions, and 8.1% reported using confocal microscopy.
Survey Responses (I), n=86.
| Professional category | Staff physicians: 79.1% (68/86) | Residents: 20.9% (18/86) | |
| Sex | Female: 73.3% (63/86) | Male: 26.7% (23/86) | |
| Median (IQR) duration of professional experience, including residency, y | 10.5 (4.25-17.75) | ||
| Sector of work | Public health: 45.3% (39/86) | Private health: 16.3% (14/86) | Both: 38.4% (33/86) |
| Involvement in dermatologic-oncology | Yes: 53.5% (46/86) | No: 46.5% (40/86) | |
| Involvement in digital dermoscopy | Yes: 47.7% (41/86) | No: 52.3% (45/86) | |
| Habitual use of dermoscopy to evaluate melanocytic lesions | Yes: 98.8% (85/86) | No: 1.2% (1/86) | |
| Habitual use of confocal microscopy to evaluate melanocytic lesions | Yes: 8.1% (7/86) | No: 91.9% (79/86) |
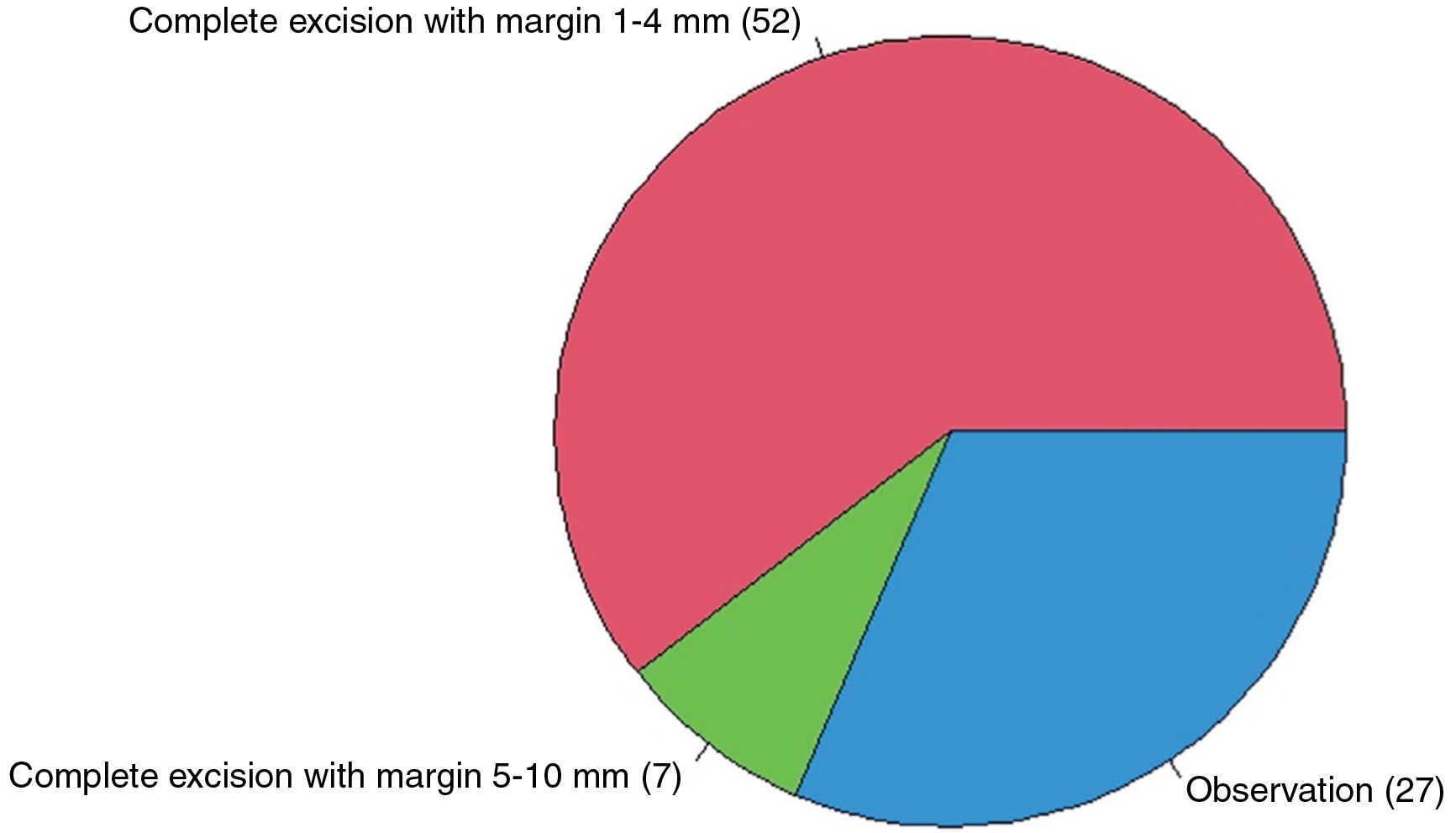
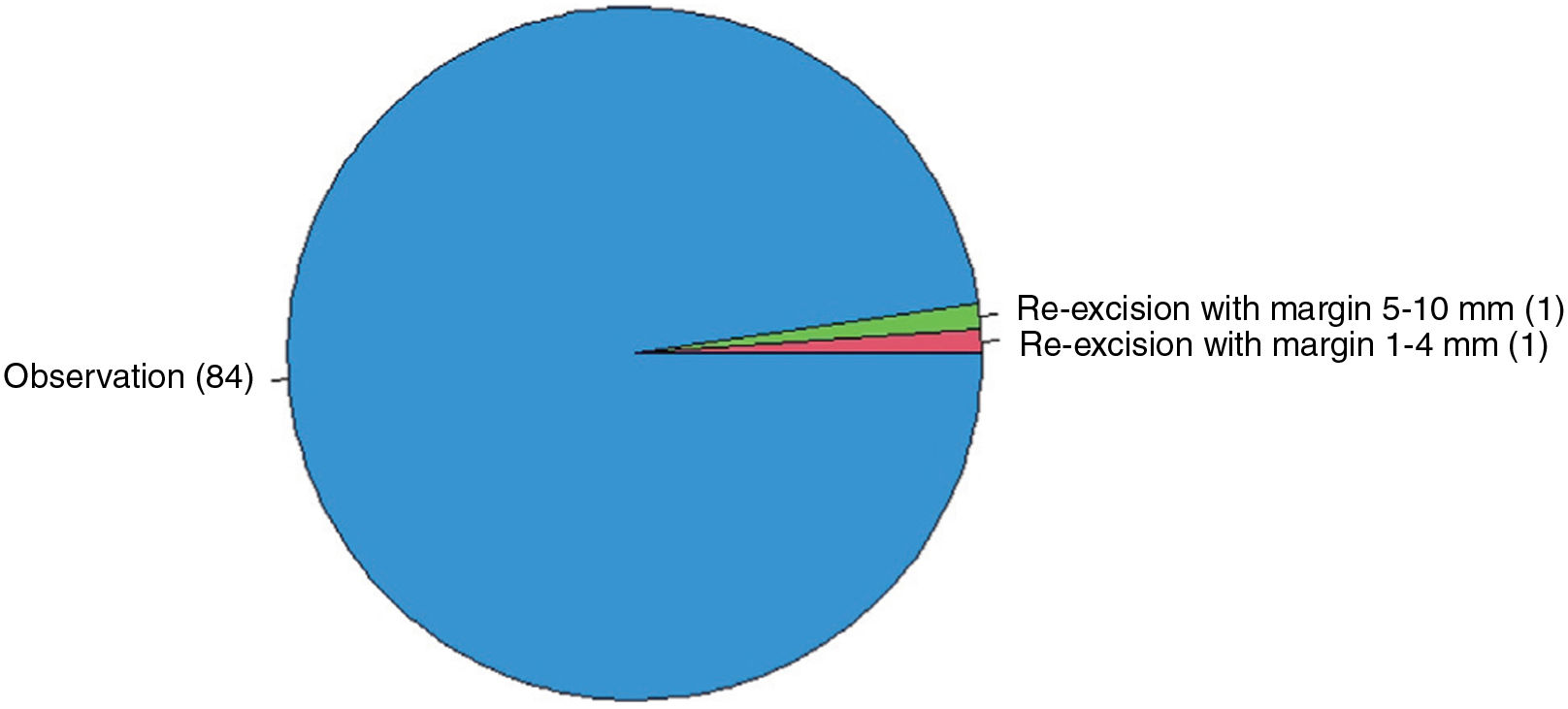
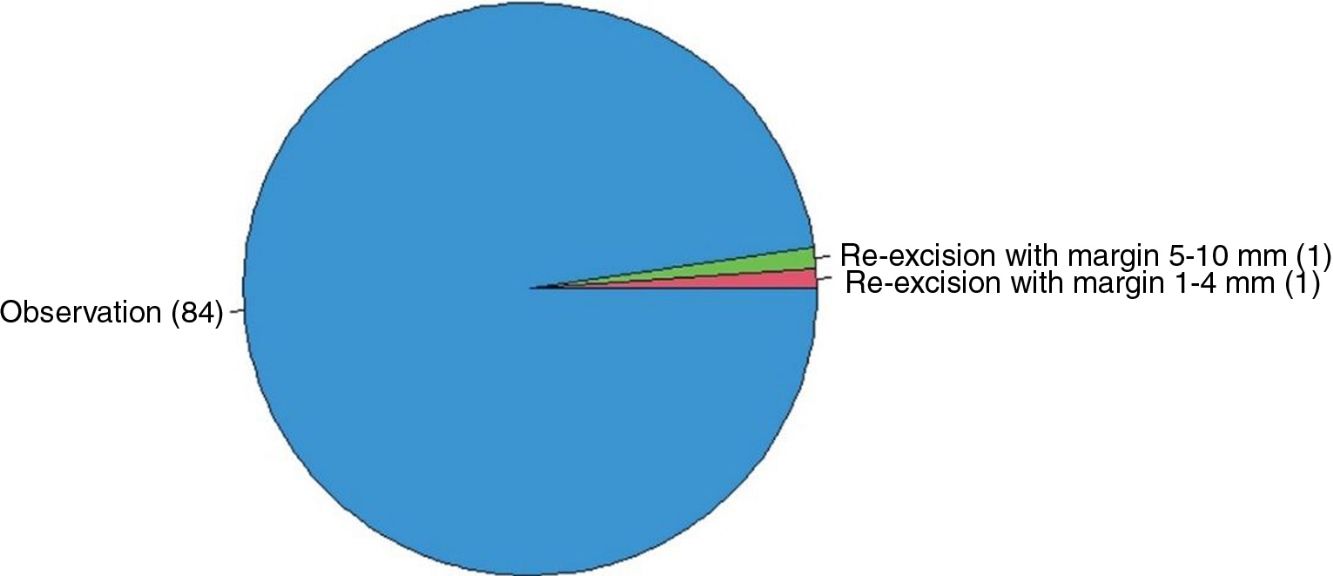
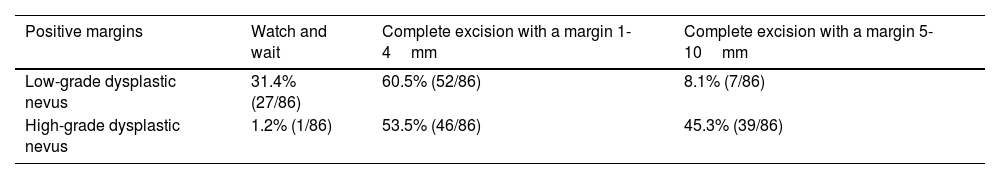
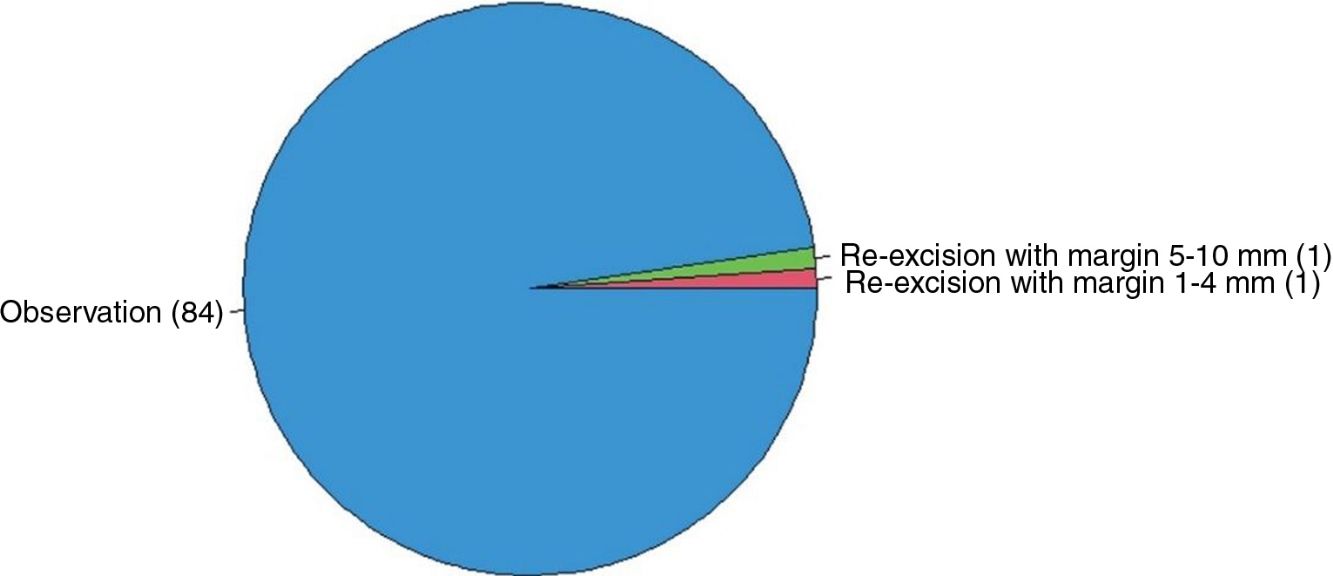
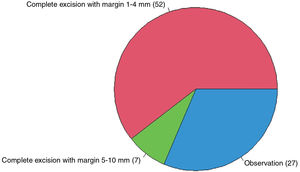
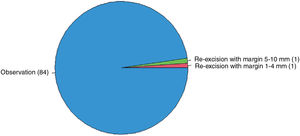
If the pathologist reported positive margins in low-grade DN in a patient with no history of interest (Fig. 1), 60.5% stated that they would opt for re-excision with a margin of 1-4mm, 31.4% would watch and wait, and 8.1% would opt for re-excision with a margin of 5-10mm. In the cases of low-grade DN with negative margins in a patient with no history of interest (Fig. 2), 97.7% would watch and wait (observation).
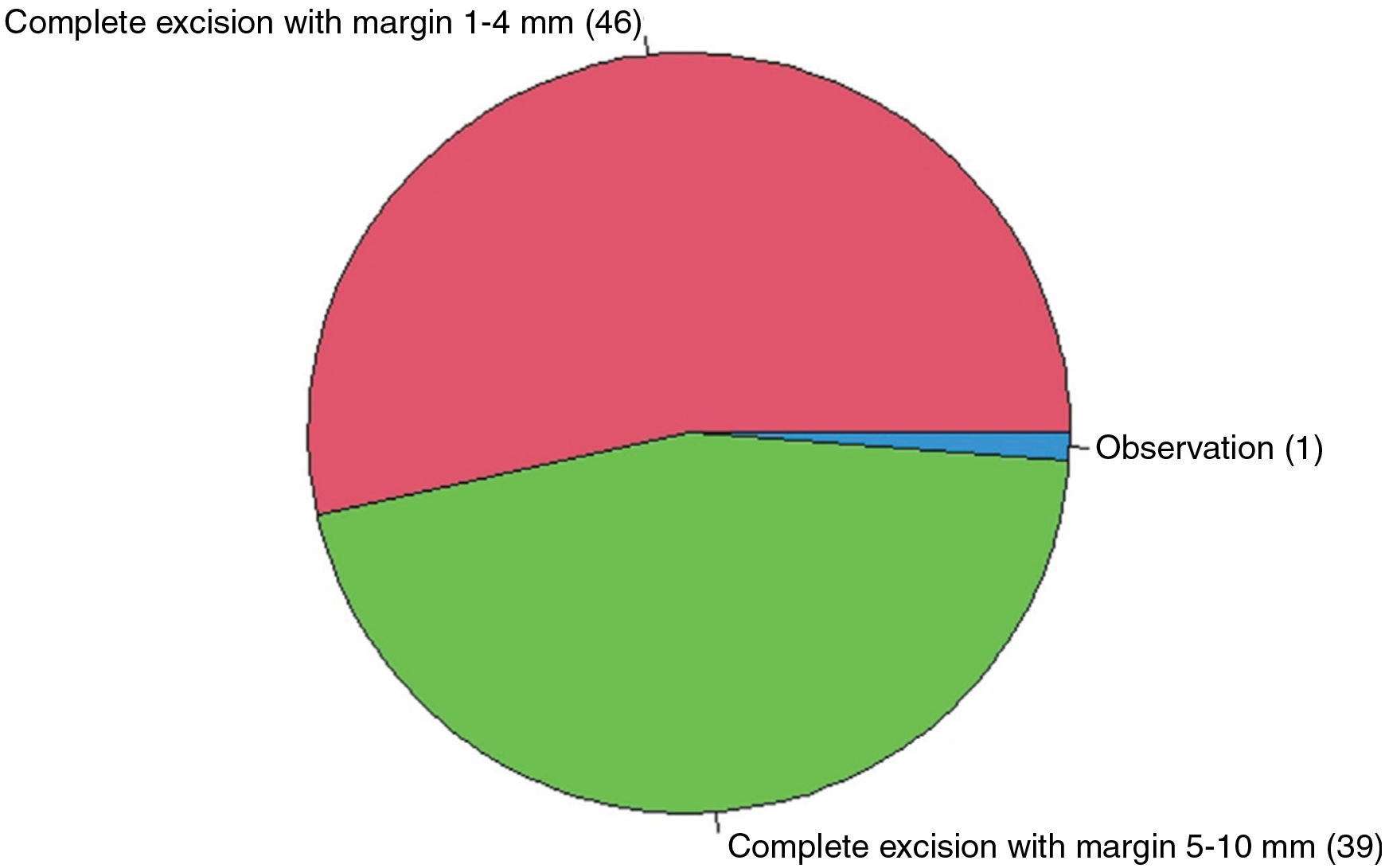
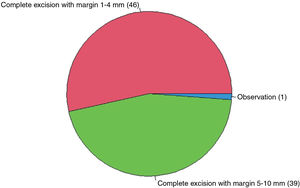
If the pathologist reported positive margins in high-grade DN in a patient with no history of interest (Fig. 3), 98.8% of the respondents said they would opt for re-excision with a margin of 1-4mm (53.5%) or with a margin of 5-10mm (45.3%).
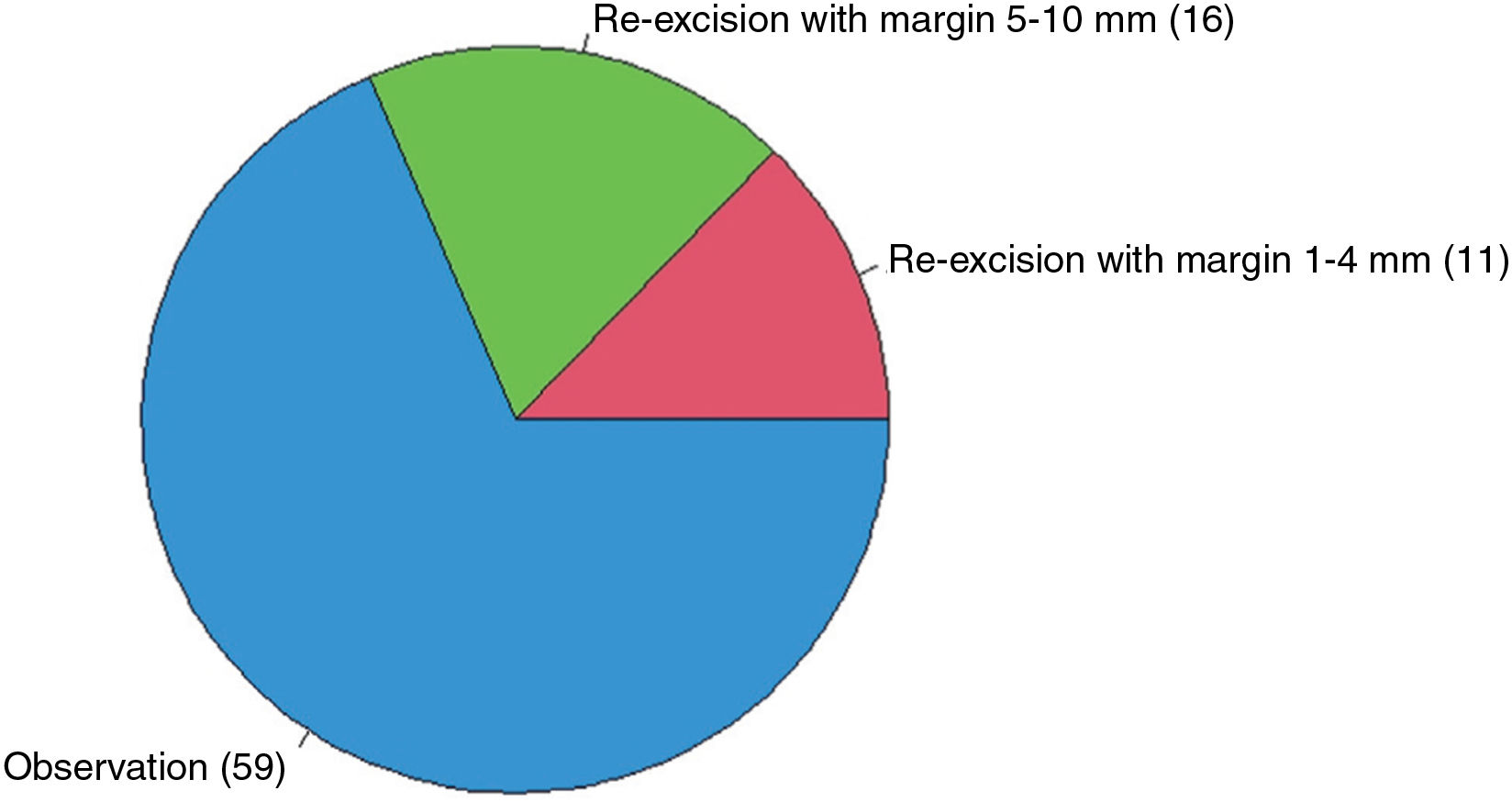
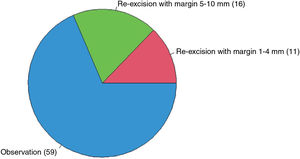
As for high-grade DN with negative margins in a patient with no history of interest (Fig. 4), 68.6% would watch and wait, 18.6% would opt for re-excision with a margin of 5-10mm, and 12.8% would do so with a margin of 1-4mm.
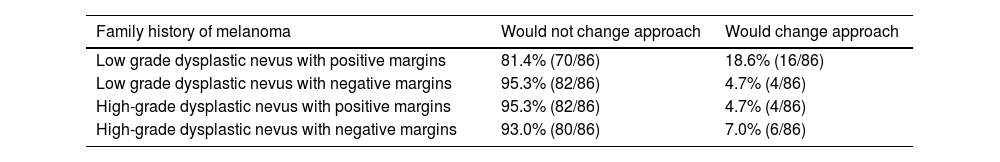
In all these clinical situations (see Table 2 for a summary), a family history or personal history of melanoma would not affect the approach taken by most of the respondents in the case of a patient with no history of interest (Table 3). As an anecdotal finding, irrespective of margin status, some free responses recommended including the patient in digital dermoscopy monitoring in the case of low-grade DN and a family or personal history of melanoma and digital dermoscopy monitoring and a genetic study in the case of high-grade DN and a family or personal history of melanoma. The respondents did not specify whether they would order a genetic study for the DN specimen or the patient.
Survey Responses (II), n=86.
| Positive margins | Watch and wait | Complete excision with a margin 1-4mm | Complete excision with a margin 5-10mm |
|---|---|---|---|
| Low-grade dysplastic nevus | 31.4% (27/86) | 60.5% (52/86) | 8.1% (7/86) |
| High-grade dysplastic nevus | 1.2% (1/86) | 53.5% (46/86) | 45.3% (39/86) |
| Negative margins | Watch and wait | Re-excision with a margin 1-4mm | Re-excision with a margin 5-10mm |
|---|---|---|---|
| Low-grade dysplastic nevus | 97.7% (84/86) | 1.2% (1/86) | 1.2% (1/86) |
| High-grade dysplastic nevus | 68.6% (59/86) | 12.8% (11/86) | 18.6% (16/86) |
Survey Responses (III), n=86.
| Family history of melanoma | Would not change approach | Would change approach |
|---|---|---|
| Low grade dysplastic nevus with positive margins | 81.4% (70/86) | 18.6% (16/86) |
| Low grade dysplastic nevus with negative margins | 95.3% (82/86) | 4.7% (4/86) |
| High-grade dysplastic nevus with positive margins | 95.3% (82/86) | 4.7% (4/86) |
| High-grade dysplastic nevus with negative margins | 93.0% (80/86) | 7.0% (6/86) |
| Personal history of melanoma | Would not change approach | Would change approach |
|---|---|---|
| Low grade dysplastic nevus with positive margins | 62.8% (54/86) | 37.2% (32/86) |
| Low grade dysplastic nevus with negative margins | 84.9% (73/86) | 15.1% (13/86) |
| High-grade dysplastic nevus with positive margins | 81.4% (70/86) | 18.6% (16/86) |
| High-grade dysplastic nevus with negative margins | 73.3% (63/86) | 26.7% (23/86) |
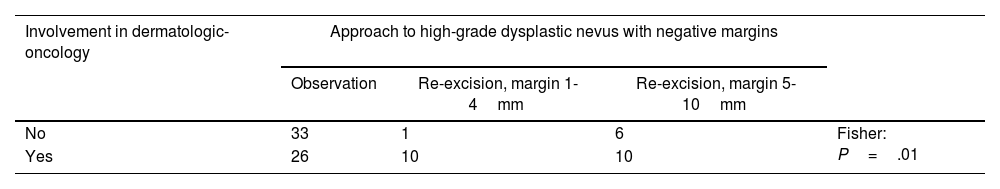
Practice in dermatology-oncology affected the management of high-grade DN with negative margins (P=.01); this difference was not observed in the cases of respondents working in digital dermoscopy (Table 4). Practice in dermatologic-oncology or digital dermoscopy did not seem to influence the management of low-grade DN with positive margins (Table 4).
Analysis of Survey Responses (I): Contingency Tables.
| Involvement in dermatologic-oncology | Approach to high-grade dysplastic nevus with negative margins | |||
|---|---|---|---|---|
| Observation | Re-excision, margin 1-4mm | Re-excision, margin 5-10mm | ||
| No | 33 | 1 | 6 | Fisher: P=.01 |
| Yes | 26 | 10 | 10 | |
| Involvement in digital dermoscopy | Approach to high-grade dysplastic nevus with negative margins | |||
|---|---|---|---|---|
| Observation | Re-excision, margin 1-4mm | Re-excision, margin 5-10mm | ||
| No | 31 | 4 | 10 | Fisher: P=.45 |
| Yes | 28 | 7 | 6 | |
| Involvement in dermatologic-oncology | Approach to low-grade dysplastic nevus with positive margins | |||
|---|---|---|---|---|
| Observation | Complete excision, margin 1-4mm | Complete excision, margin 5-10mm | ||
| No | 13 | 23 | 4 | Fisher: P=.84 |
| Yes | 14 | 29 | 3 | |
| Involvement in digital dermoscopy | Approach to low-grade dysplastic nevus with positive margins | |||
|---|---|---|---|---|
| Observation | Complete excision, margin 1-4mm | Complete excision, margin 5-10mm | ||
| No | 10 | 31 | 4 | Fisher: P=.15 |
| Yes | 17 | 21 | 3 | |
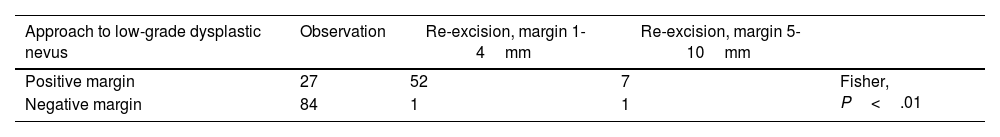
The approach to low- or high-grade DN varies according to margin status (positive or negative) (P<.01) and the grade of dysplasia (P<.01) (Table 5).
Analysis of Survey Responses (II): Contingency Tables.
| Approach to low-grade dysplastic nevus | Observation | Re-excision, margin 1-4mm | Re-excision, margin 5-10mm | |
|---|---|---|---|---|
| Positive margin | 27 | 52 | 7 | Fisher, P<.01 |
| Negative margin | 84 | 1 | 1 |
| Approach to high-grade dysplastic nevus | Observation | Re-excision, margin 1-4mm | Re-excision, margin 5-10mm | |
|---|---|---|---|---|
| Positive margin | 1 | 46 | 39 | Fisher: P<.01 |
| Negative margin | 59 | 11 | 16 |
| Approach to dysplastic nevus with positive margins | Observation | Re-excision, margin 1-4mm | Re-excision, margin 5-10mm | |
|---|---|---|---|---|
| Low-grade dysplasia | 27 | 52 | 7 | Fisher: P<.01 |
| High-grade dysplasia | 1 | 46 | 39 |
| Approach to dysplastic nevus with negative margins | Observation | Re-excision, margin 1-4mm | Re-excision, margin 5-10mm | |
|---|---|---|---|---|
| Low-grade dysplasia | 84 | 1 | 1 | Fisher: P<.01 |
| High-grade dysplasia | 59 | 11 | 16 |
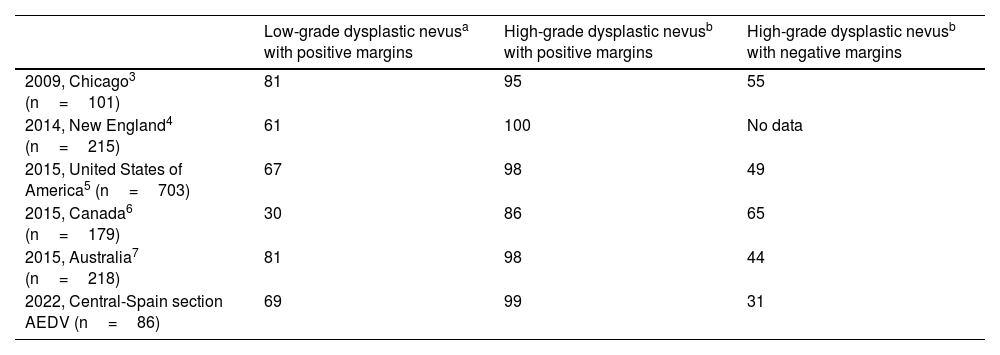
DN has been considered a controversial condition for some years, and its management has been inconsistent among dermatologists owing to the lack of clinical practice guidelines.2–9 Clinically atypical melanocytic lesions should be addressed by means of excisional biopsy, as proposed in our survey. Incisional biopsy should be avoided where possible given the possibility of an erroneous diagnosis.8,10–12 The percentage of survey respondents who would re-excise low-grade DN with positive margins and high-grade DN with positive margins is similar to those reported in surveys published in 2015 and previously (Table 6).2–7 We found that, even today, 68.6% of dermatologists would opt for re-excision in a low-grade DN that had been excised and for which histology revealed margin involvement, despite the 2015 recommendations of the National Institutes of Health and recent reviews, which support the possibility of watch and wait in moderate-grade DN (currently low-grade) if the lesion was completely and clinically removed.1,8,10,13,14 We believe that a possible reason for this high percentage could be the wish to avoid the diagnostic difficulty that arises when differentiating between persistent nevus and melanoma if the scar tissue is pigmented.13 The fourth edition of the WHO Classification of Skin Tumours (in force at the time of our survey) makes no direct recommendation for this clinical supposition. However, the fifth edition, which was published online in 2023, states that re-excision could be considered in low-grade DN with positive margins, although this may not be necessary, especially if the patient is to be followed up.15
Comparisons With Previous Surveys: Percentage of Respondents Who Would Re-excise the Lesion.
| Low-grade dysplastic nevusa with positive margins | High-grade dysplastic nevusb with positive margins | High-grade dysplastic nevusb with negative margins | |
|---|---|---|---|
| 2009, Chicago3 (n=101) | 81 | 95 | 55 |
| 2014, New England4 (n=215) | 61 | 100 | No data |
| 2015, United States of America5 (n=703) | 67 | 98 | 49 |
| 2015, Canada6 (n=179) | 30 | 86 | 65 |
| 2015, Australia7 (n=218) | 81 | 98 | 44 |
| 2022, Central-Spain section AEDV (n=86) | 69 | 99 | 31 |
Abbreviation: AEDV, Academia Española de Dermatología y Venereología (Spanish Academy of Dermatology and Venereology).
Almost all the respondents would opt for re-excision of a high-grade DN with margin involvement, in line with previously published results (Table 6) and with the explicit recommendation in the fifth edition of the WHO Classification of Skin Tumours, owing to overlapping diagnostic criteria between high-grade DN and melanoma and the possibility—albeit low—of progression to melanoma.2–7,11,15
The percentage of dermatologists who would re-excise a high-grade DN with negative margins is the lowest to date (Table 6), perhaps owing to the influence of the publication in 2018 of the fourth edition of the WHO Classification of Skin Tumours, in which it was inferred that once a DN is completely removed, there is no need to re-excise the scar.1–7,13 Retrospective studies suggest that DN with severe dysplasia (currently high-grade) that has been completely removed with negative margins would not have to be re-excised, although other authors highlight the need for prospective studies before making such a recommendation, especially if the margin is narrow.10,14–17 The fifth edition of the WHO Classification of Skin Tumours only refers to management of high-grade DN with margin involvement (see above); therefore, once again, we infer that if the tumor has been removed with negative margins, re-excision would not be necessary. Future surveys should analyze whether the new WHO recommendations would reduce the percentage of dermatologists who would re-excise a low-grade DN with positive margins or a high-grade DN with negative margins.
Consistent with the findings of Duffy et al.3 in 2009, our findings show that the clinician's decision to re-excise or observe lesions diagnosed as DN is affected by both the grade of dysplasia and margin status.
The respondents who were involved in dermatologic-oncology took a more aggressive approach to treatment of high-grade DN with negative margins (with statistically significant differences) (Table 4), thus leading us to believe that their management of DN could be, in part, biased by the malignant diseases they usually treat in the clinic.
As for the change in clinical approach depending on whether the patient had a family or personal history of melanoma, most of the respondents stated that they would not modify their approach. While we did not find similar questions in other published surveys, Sapra et al.6 reported in 2015 that half of dermatologists would agree to closer follow-up of patients with a family history of melanoma. In our survey, we did not ask directly about patient follow-up, although some dermatologists did make reference to closer follow-up with digital dermoscopy in the case of DN and a family or personal history of melanoma, probably owing to the importance of DN as a marker of the risk of developing melanoma.1,9,15
We wish to highlight the role of dermoscopy as an essential tool for routine assessment of melanocytic lesions among almost all the respondents (98.8% vs. 23% in an American survey from 20012). Furthermore, more modern, noninvasive diagnostic techniques, such as reflectance confocal microscopy, are now routinely used by 8.1% of respondents in our survey. This percentage seems likely to increase in the future, with more extended use of the technique by dermatologists.9
Of course, real-world management of DN must be agreed with the patient, whose decisions are affected by the information we provide them with. In this sense, in their 2020 study, Batchelder et al.18 stressed the importance of the words we use and the way in which we transmit information on the risk or absence of risk of DN when patients decide on whether to undergo surgery and recommended avoidance of terms such as premelanoma or precancer.
Our study is limited by the fact that it was a nonvalidated survey with a low response rate, indicating a potential response bias. In addition, as the survey was anonymous, with no identifying data (e.g., national identity number, email address), we could not ensure that a single person completed the survey several times or that dermatologists not belonging to the center-Spain section of the AEDV completed the survey if they were able to obtain the weblink. Moreover, the survey is a simplified version of daily practice, in which it is not possible to include factors such as the nuances of the workplace and patient characteristics. We must also bear in mind that the survey parted from the premise of biopsy-confirmed DN, in which, according to Aydin Ulgen et al.,19 interobserver variability among histopathologists has improved with the diagnostic criteria of the fourth edition of the WHO criteria for DN (κfree, 0.40). One of the strengths of our study is that it is the first survey in Spanish to evaluate management of DN by dermatologists in our setting: all previous surveys were in English, with data from other countries that may not be wholly generalizable to our practice.2–7 The survey was simple and short (only a few minutes to complete) and was available only online (paper-free). We believe this made it easier to participate and limited the effect on the environment.
ConclusionsManagement of DN differs widely between dermatologists from the center-Spain section of the AEDV, especially in the case of low-grade DN with positive margins and high-grade DN with negative margins. In most cases, a personal or family history of melanoma did not modify the clinician's approach. The recent recommendations of the fifth edition of the WHO Classification of Skin Tumours are adapted to the management of high-grade DN with positive margins. Future prospective studies and the drafting of clinical practice guidelines will probably help to homogenize management of DN.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We are grateful to Dr. Teresa Estrach (Mentorship Program in Dermatologic Research, AEDV) and to Dr. Ignacio García Doval (Research Unit, AEDV) for their help and collaboration in this project.