Neurosarcoidosis is an uncommon but potentially serious disease of the central nervous system that can cause major sequelae. We analyzed the presence and diagnostic usefulness of specific cutaneous lesions in 58 patients with neurosarcoidosis. Sixteen patients (27.6%) had specific cutaneous lesions (14 men and 2 women; mean age, 50 years [range, 20-84 years]). Twenty-four types of neurological lesions were observed: cranial neuropathy (n=7), parenchymal lesions (n=4), meningeal lesions (n=3), myelopathy (n=3), pituitary lesions (n=1), hydrocephalus (n=2), and peripheral neuropathy (n=4). Twenty types of specific cutaneous lesions were observed: maculopapular lesions (n=6), plaques (n=9), lupus pernio (n=1), and scar sarcoidosis (n=4). These last lesions coexisted with maculopapular lesions in 2 patients and plaques in another 2. Specific cutaneous lesions were present at diagnosis of neurosarcoidosis in 13 patients. Recognition of specific cutaneous lesions in a patient with suspected neurosarcoidosis is important as biopsy can accelerate diagnosis.
La sarcoidosis del sistema nervioso (neurosarcoidosis [NS]) es poco frecuente, pero puede ser grave y producir secuelas importantes. Analizamos los tipos de lesión cutánea específica en pacientes con NS y su utilidad para el diagnóstico de la enfermedad. De un total de 58, 16 presentaron lesiones cutáneas específicas (27,6%). De ellos, 14 eran mujeres y dos varones (edad mediana 50 años [rango 20-84]), que presentaron 24 tipos de lesiones neurológicas (siete neuropatía craneal, cuatro parenquimatosa, tres meníngea, tres mielopatía, uno hipofisaria, dos hidrocefalia y cuatro neuropatía periférica) y 20 lesiones cutáneas específicas (seis máculo-pápulas, nueve placas, uno lupus pernio y cuatro sarcoidosis de las cicatrices [dos pacientes con máculo-pápulas y dos con placas presentaron también sarcoidosis de las cicatrices]. Las lesiones cutáneas estaban presentes al diagnóstico de la NS en 13 casos. Ante la sospecha de esta enfermedad hay que descartar la presencia de lesiones cutáneas específicas cuya biopsia puede acelerar el diagnóstico.
Sarcoidosis is a multisystemic granulomatous disease that more often affects the lungs, eyes, and skin. Specific (granulomatous) skin lesions occur in 9% to 37% of the patients. They are often categorized as maculopapular, plaques, lupus pernio, subcutaneous sarcoidosis, and scar sarcoidosis, and provide information on the prognosis of systemic disease.1 Nervous system involvement or neurosarcoidosis (NS) is less common, but it can become more severe and result in significant complications.2–5 The diagnosis of sarcoidosis is often challenging due to how difficult it is to perform biopsies on the nervous system. However, the presence of specific skin lesions in patients with NS can facilitate it and provide prognostic information.
Our objective was to analyze the different types of specific skin lesions that exist in patients with NS, as well as their diagnostic utility.
Patients and methodsWe selected patients with NS diagnosed in our center from 1980 through 2022 with specific skin lesions. Ours is a tertiary referral teaching hospital that provides health care to a population of nearly 1 million people. Histopathological confirmation of granulomatous skin occurred in all cases. The diagnosis of systemic sarcoidosis was established based on classical criteria: clinical and radiological presentation consistent with the disease; histopathological demonstration of noncaseating granulomas involving one or more tissues, or a positive Kveim test, and the exclusion of other granulomatous diseases.
All patients with sarcoidosis were followed prospectively. Investigations included the patients’ past medical history, physical and ophthalmological examinations, thoracic x-rays, standard hematological and biochemical profiles (including serum calcium level, liver enzymes, renal function tests, and serum angiotensin-converting enzyme [ACE] level), tuberculin skin test, and pulmonary function tests (forced vital capacity and carbon monoxide diffusion capacity). The patients were monitored through clinical evaluation and thoracic x-rays every 3 months until the disease became inactive, and then annually.
Specific skin lesions were categorized as maculopapular, plaques, lupus pernio, scar sarcoidosis, and subcutaneous sarcoidosis.
Health records were retrospectively reviewed to obtain the following data: gender, race, age at the time of diagnosis of specific skin lesions, types of specific skin lesions (maculopapular, plaques, lupus pernio, scar sarcoidosis, and subcutaneous sarcoidosis), and type of neurological involvement (parenchymal, cranial nerves [CN], meningeal, pituitary, myelopathy, and peripheral neuropathy).
ResultsFifty-eight (8%) out of a total of 728 patients with systemic sarcoidosis diagnosed in our hospital had NS. Of these, 16 had histopathologically confirmed specific skin lesions (27.6%) and were included in the study. There were 14 women and 2 men with ages ranging from 20 to 84 (median age, 50 years). A total of 24 types of different neurological lesions were detected among these patients: CN involvement in 7 cases, parenchymal in 4, meningeal in 3, myelopathy in 3, pituitary in 1, hydrocephalus in 2, and peripheral neuropathic involvement in 4.
The 16 patients included in the study had a total of 20 specific skin lesions: 6 maculopapular lesions, 9 plaques, 1 lupus pernio, and 4 scar sarcoidosis (2 with maculopapular lesions and 2 with plaques simultaneously). In 13 cases, skin lesions were present at the onset of NS, thus contributing to its diagnosis.
In 7 patients, specific skin lesions and NS clinically manifested simultaneously, in 6 cases, the skin lesions appeared prior to the skin lesions (between 6 months and 10 years earlier), and only in 3 cases did NS manifest prior to the skin lesions (between 1 and 8 years earlier).
Figure 1 shows clinical images of some of the skin lesions and images of NS lesions obtained through nuclear magnetic resonance imaging.
Clinical images of some skin lesions in patients with NS, and images of NS lesions obtained through nuclear magnetic resonance imaging. a) Infiltrated plaque on the nose. b) Infiltrated plaque on the neck lateral side. c) Annular plaque on the buttock. d) Erythematous-violaceous plaques on the buttocks. e) Lupus pernio lesions on the nasal window. f) Papular sarcoidosis on the knees. g) Nuclear magnetic resonance imaging: Transverse FLAIR sequence showing bilateral mesencephalic hyperintense areas and in the hypothalamus. h) Nuclear magnetic resonance imaging: T1-weighted sequence with gadolinium showing diffuse meningeal enhancement. i) Magnetic resonance imaging: STIR sequence of the spinal cord with hyperintensity of the spinal cord consistent with longitudinally extensive transverse myelitis.
FLAIR, fluid attenuated inversion recovery; NS, neurosarcoidosis; STIR, short-tau inversion-recovery.
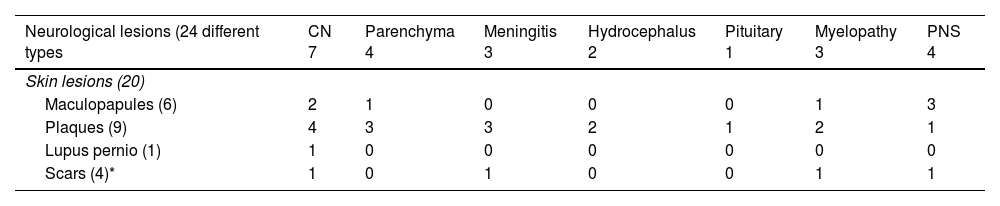
Table 1 illustrates the skin lesions associated with each type of neurological involvement.
Clinical characteristics of patients and skin lesions associated with each type of neurological involvement.
| Neurological lesions (24 different types | CN 7 | Parenchyma 4 | Meningitis 3 | Hydrocephalus 2 | Pituitary 1 | Myelopathy 3 | PNS 4 |
|---|---|---|---|---|---|---|---|
| Skin lesions (20) | |||||||
| Maculopapules (6) | 2 | 1 | 0 | 0 | 0 | 1 | 3 |
| Plaques (9) | 4 | 3 | 3 | 2 | 1 | 2 | 1 |
| Lupus pernio (1) | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Scars (4)* | 1 | 0 | 1 | 0 | 0 | 1 | 1 |
CN, cranial nerves; PNS, peripheral nervous system.
Chronic forms of specific skin lesions (plaques and lupus pernio) were the most frequently observed. Plaques were the most common specific skin lesions in patients with central nervous system involvement (parenchymal, CN, meningeal, and hydrocephalus), while maculopapular lesions were the most widely reported skin lesions in patients with peripheral nervous system (PNS) involvement.
DiscussionBetween 5% and 10% of the patients with sarcoidosis show clinically recognizable neurological involvement.2,3 NS can affect the brain parenchyma, CN, meninges, spinal cord, the hypothalamic-pituitary axis, and the PNS.2,4,5 Parenchymal lesions account for 30% to 50% of the cases of NS and can clinically show as seizures, encephalopathy, or focal neurological deficits.2,6,7 Imaging modalities may reveal single or multiple nodular intraparenchymal lesions with surrounding edema that can mimic malignancy.8 They are more common in the hypothalamus, brainstem, and cerebral hemispheres.9 CN can be affected by granulomatous infiltration, adjacent meningeal disease, or be the result of increased intracranial pressure.5,7 Unilateral or bilateral facial nerve paralysis accounts for up to 65% of cranial neuropathies.2,10 Vestibulocochlear nerve involvement leads to hearing loss, tinnitus, and vertigo in 6% to 17% of the patients with NS.11,12 Trigeminal neuropathy occurs in 12% of the cases of NS and presents with facial pain and/or numbness.13 Diplopia due to lesions involving CN III, IV, or VI occurs in 9% of the cases of NS.13 Optic neuropathy is seen in one third of the patients with NS and can be difficult to distinguish from optic neuritis due to multiple sclerosis.14 Symptomatic meningitis occurs in 10% to 20% of the cases of NS and presents clinically with headaches that may be accompanied by other signs of meningeal irritation.2,11 However, the MRI can detect meningeal lesions in 46% to 67% of the patients.2,7 Between 15% and 20% of the patients with NS develop myelopathy. Diagnosis is often delayed due to misdiagnosis as compressive myelopathy or idiopathic transverse myelitis.14 Hypothalamic-pituitary involvement occurs in 6% to 9% of the patients with NS and results in hormonal abnormalities such as hypothyroidism, hypogonadism, syndrome of inappropriate antidiuretic hormone secretion, and central diabetes insipidus.2,7,15,16 PNS is involved in 14% to 21% of the cases of NS, being the most common pattern a distal sensory-motor axonal polyneuropathy with glove-and-stocking pain and paresthesias.2,12
NS often manifests in the 4th decade of life and is slightly more common in women (50% to 55%).2,6–8 According to these data from the medical literature, our patients also predominantly included women (14 out of 16 cases, 7:1), being the median age, 50 years.
Regarding the prognostic significance of specific skin lesions in sarcoidosis, maculopapules and subcutaneous sarcoidosis tend to occur in patients with acute forms of systemic sarcoidosis, while plaques and lupus pernio are associated with chronic forms, indicating a worse prognosis.17 The prognostic significance of scar sarcoidosis is not well-established.17 Chronic forms of specific skin lesions (plaques and lupus pernio) were seen more often in our patients with NS (10 cases), while acute forms (maculopapules) were a less common finding (6 cases). When their relationship with the type of neurological lesion was studied, plaques were the most common skin lesions in patients with central nervous system involvement, whereas maculopapules were the most common skin lesions in those with PNS involvement.
We should mention that skin lesions contributed to the diagnosis of the disease in 13 out of 16 patients (81.3%), with skin lesions preceding neurological signs in 6 cases and occurring simultaneously with neurological symptoms in 7 cases, thus contributing to achieve diagnosis.
Limitations of our study include its retrospective nature and the limited number of patients included.
Patients with NS may present specific skin lesions, predominantly in women aged between 40 and 60 years. Overall, plaques were the most common specific skin lesions reported, especially in those with central nervous system damage, while maculopapules were the most common specific skin lesions in those with PNS involvement. When NS is suspected, the skin should be examined to detect the potential presence of specific skin lesions, whose biopsy can expedite the diagnostic process, thus allowing for early treatment and prevention of potential complications.
Conflicts of interestNone declared.