Recent scientific evidence and the incorporation of new drugs into the therapeutic arsenal against rosacea have made it necessary to review and update treatment criteria and strategies. To this end, a panel of 15 dermatologists, all experts in rosacea, was formed to share experiences and discuss treatment options, response criteria, and changes to treatment. Based on a critical review of the literature and a discussion of the routine practices of Spanish dermatologists, the panel proposed and debated different options, with consideration of the experience of professionals and the preferences of patients or equality criteria. Following validation of the proposals, the final recommendations were formulated and, together with the evidence from the main international guidelines and studies, used to produce this consensus document. The goal of this consensus document is to provide dermatologists with practical recommendations for the management of rosacea.
Las últimas evidencias científicas y la incorporación de nuevos fármacos al arsenal terapéutico de la rosácea hacen necesario revisar y actualizar los criterios y estrategias de tratamiento. Con este fin, un grupo de 15 dermatólogos expertos en esta enfermedad aportaron y discutieron acerca de las diferentes terapias y los criterios de respuesta y cambio de tratamiento. Partiendo de la revisión crítica de la bibliografía y de la exposición de los hábitos de los dermatólogos españoles en su práctica clínica, se formularon distintas propuestas que fueron debatidas teniendo en consideración tanto la experiencia profesional como las preferencias de los pacientes o los criterios de equidad. Una vez validadas las propuestas, se formularon las recomendaciones finales que, junto con la evidencia aportada por las principales guías y estudios internacionales, dieron lugar al presente documento. El objetivo de este consenso es ofrecer al dermatólogo un enfoque práctico para abordar la rosácea.
Rosacea is a common chronic skin disease that causes redness, papules, and pustules mainly on the face. The eyes can also become compromised and the skin may thicken and increase in volume in the phymatous form of the disease.1
Although epidemiologic statistics vary, studies in Europe and the United States estimate that the incidence ranges from less than 1% to more than 20% in different general populations.2 However, comparisons are difficult because of variations in methodology. Examples of overall prevalence rates reported are 2.2% for Germany,3 between 1.3% and 2.1% for the United States,4 and 22% for Estonia.5
Rosacea tends to appear between the ages of 30 and 50 years6 and more often in women than men,4 although men are more likely to develop the phymatous form.7 Any racial or ethnic group may be affected, but persons with pale skin have greater propensity.6
Few studies have looked at the pathogenesis of rosacea, but some evidence supports the hypothesis that a genetic predisposition plays a key role8,9 and that changes in the innate immune system are involved. There is also evidence of certain environmental and other predisposing factors, or triggers,2 among them foods, emotions, or the use of certain topical treatments.10
In spite of the availability of scientific evidence, criteria for diagnosing and treating the disease differ and are not always in accordance with clinical subtypes.4 Recent years have seen many advances in the treatment of facial erythema,11,12 underlining the need to review and update diagnostic criteria and therapeutic approaches.
This consensus statement was drafted on the basis of guidelines and systematic reviews of the evidence on rosacea, among them the ones published by the American Acne and Rosacea Society13–17 and the Cochrane study of interventions,8 which also took supplementary data from a German guideline into consideration. Thus, the present Spanish consensus brings together the latest evidence available,19 including studies related to the clinical assessment of the disease, treatment objectives, and therapies. It is meant to provide a point of reference and practice recommendations for dermatologists who treat rosacea. The statement does not include less common and complex forms of the disease, such as those caused by infestations of mites (Demodex species), granulomatous rosacea, or rosacea fulminans. Nor does it discuss the various cosmetic products often used by patients with rosacea (cleansers, moisturizers, sunscreens, etc.). Such products, even though considered necessary by the panel of experts, are not covered by this statement.
MethodsFifteen dermatologists were selected for the panel of experts on the basis of their level of knowledge and clinical and research experience (see online supplementary material, in Spanish). One of the experts (M.S.) served as coordinator; the others all participated in the discussion and validation steps.
The coordinator provided a list of topics consisting of clinically important questions that would be addressed by the panel's recommendations. She then collected and interpreted available evidence after a review of the literature and drafted a set of recommendations to submit to the panel of expert dermatologists.
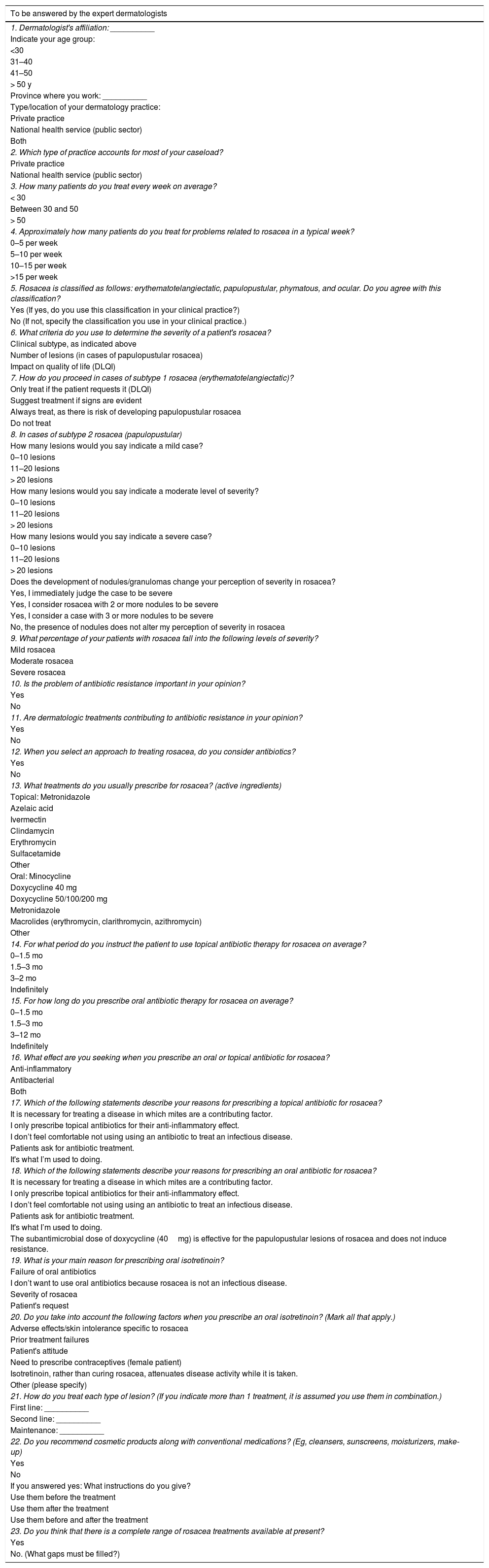
To characterize the approaches the expert panel applied in their own clinical practices, the dermatologists answered 23 questions related to their diagnosis and treatment of the disease (Table 1). (See online supplementary material, Table S1 for the most important results, in Spanish.) Based on the survey and the review of the literature, the coordinator drafted recommendations on which the panel reached consensus through discussion. Discussion focused mainly on questions about which opinions diverged or for which evidence was lacking.
Initial Questionnaire to Determine the Profiles of the Panel of Experts and Their Approaches to Rosacea
| To be answered by the expert dermatologists |
|---|
| 1. Dermatologist's affiliation: __________ |
| Indicate your age group: |
| <30 |
| 31–40 |
| 41–50 |
| > 50 y |
| Province where you work: __________ |
| Type/location of your dermatology practice: |
| Private practice |
| National health service (public sector) |
| Both |
| 2. Which type of practice accounts for most of your caseload? |
| Private practice |
| National health service (public sector) |
| 3. How many patients do you treat every week on average? |
| < 30 |
| Between 30 and 50 |
| > 50 |
| 4. Approximately how many patients do you treat for problems related to rosacea in a typical week? |
| 0–5 per week |
| 5–10 per week |
| 10–15 per week |
| >15 per week |
| 5. Rosacea is classified as follows: erythematotelangiectatic, papulopustular, phymatous, and ocular. Do you agree with this classification? |
| Yes (If yes, do you use this classification in your clinical practice?) |
| No (If not, specify the classification you use in your clinical practice.) |
| 6. What criteria do you use to determine the severity of a patient's rosacea? |
| Clinical subtype, as indicated above |
| Number of lesions (in cases of papulopustular rosacea) |
| Impact on quality of life (DLQI) |
| 7. How do you proceed in cases of subtype 1 rosacea (erythematotelangiectatic)? |
| Only treat if the patient requests it (DLQI) |
| Suggest treatment if signs are evident |
| Always treat, as there is risk of developing papulopustular rosacea |
| Do not treat |
| 8. In cases of subtype 2 rosacea (papulopustular) |
| How many lesions would you say indicate a mild case? |
| 0–10 lesions |
| 11–20 lesions |
| > 20 lesions |
| How many lesions would you say indicate a moderate level of severity? |
| 0–10 lesions |
| 11–20 lesions |
| > 20 lesions |
| How many lesions would you say indicate a severe case? |
| 0–10 lesions |
| 11–20 lesions |
| > 20 lesions |
| Does the development of nodules/granulomas change your perception of severity in rosacea? |
| Yes, I immediately judge the case to be severe |
| Yes, I consider rosacea with 2 or more nodules to be severe |
| Yes, I consider a case with 3 or more nodules to be severe |
| No, the presence of nodules does not alter my perception of severity in rosacea |
| 9. What percentage of your patients with rosacea fall into the following levels of severity? |
| Mild rosacea |
| Moderate rosacea |
| Severe rosacea |
| 10. Is the problem of antibiotic resistance important in your opinion? |
| Yes |
| No |
| 11. Are dermatologic treatments contributing to antibiotic resistance in your opinion? |
| Yes |
| No |
| 12. When you select an approach to treating rosacea, do you consider antibiotics? |
| Yes |
| No |
| 13. What treatments do you usually prescribe for rosacea? (active ingredients) |
| Topical: Metronidazole |
| Azelaic acid |
| Ivermectin |
| Clindamycin |
| Erythromycin |
| Sulfacetamide |
| Other |
| Oral: Minocycline |
| Doxycycline 40 mg |
| Doxycycline 50/100/200 mg |
| Metronidazole |
| Macrolides (erythromycin, clarithromycin, azithromycin) |
| Other |
| 14. For what period do you instruct the patient to use topical antibiotic therapy for rosacea on average? |
| 0–1.5 mo |
| 1.5–3 mo |
| 3–2 mo |
| Indefinitely |
| 15. For how long do you prescribe oral antibiotic therapy for rosacea on average? |
| 0–1.5 mo |
| 1.5–3 mo |
| 3–12 mo |
| Indefinitely |
| 16. What effect are you seeking when you prescribe an oral or topical antibiotic for rosacea? |
| Anti-inflammatory |
| Antibacterial |
| Both |
| 17. Which of the following statements describe your reasons for prescribing a topical antibiotic for rosacea? |
| It is necessary for treating a disease in which mites are a contributing factor. |
| I only prescribe topical antibiotics for their anti-inflammatory effect. |
| I don’t feel comfortable not using using an antibiotic to treat an infectious disease. |
| Patients ask for antibiotic treatment. |
| It's what I’m used to doing. |
| 18. Which of the following statements describe your reasons for prescribing an oral antibiotic for rosacea? |
| It is necessary for treating a disease in which mites are a contributing factor. |
| I only prescribe topical antibiotics for their anti-inflammatory effect. |
| I don’t feel comfortable not using using an antibiotic to treat an infectious disease. |
| Patients ask for antibiotic treatment. |
| It's what I’m used to doing. |
| The subantimicrobial dose of doxycycline (40mg) is effective for the papulopustular lesions of rosacea and does not induce resistance. |
| 19. What is your main reason for prescribing oral isotretinoin? |
| Failure of oral antibiotics |
| I don’t want to use oral antibiotics because rosacea is not an infectious disease. |
| Severity of rosacea |
| Patient's request |
| 20. Do you take into account the following factors when you prescribe an oral isotretinoin? (Mark all that apply.) |
| Adverse effects/skin intolerance specific to rosacea |
| Prior treatment failures |
| Patient's attitude |
| Need to prescribe contraceptives (female patient) |
| Isotretinoin, rather than curing rosacea, attenuates disease activity while it is taken. |
| Other (please specify) |
| 21. How do you treat each type of lesion? (If you indicate more than 1 treatment, it is assumed you use them in combination.) |
| First line: __________ |
| Second line: __________ |
| Maintenance: __________ |
| 22. Do you recommend cosmetic products along with conventional medications? (Eg, cleansers, sunscreens, moisturizers, make-up) |
| Yes |
| No |
| If you answered yes: What instructions do you give? |
| Use them before the treatment |
| Use them after the treatment |
| Use them before and after the treatment |
| 23. Do you think that there is a complete range of rosacea treatments available at present? |
| Yes |
| No. (What gaps must be filled?) |
Abbreviation: DLQI, Dermatology Quality of Life Index.
The following databases were searched to locate and select articles: MEDLINE/PubMed, the Cochrane Library, and Google Scholar. The search's focus was on finding original and review articles in English or Spanish published between 2002 and 2015. Limiters related to methods were as follows: reviews; case series; prevalence, cohort or case–control studies; nonrandomized and randomized controlled trials; and meta-analyses. All original research had to include patients with rosacea. The articles located were evaluated to identify those with data useful for answering the clinical questions and make recommendations based on the highest available levels of evidence. The CASPe criteria (Critical Appraisal Skills Programme, Spanish version)20 were used to assess quality and validity. From these criteria the strength of evidence offered by each study was inferred, to determine the level of impact each would have on recommendations.
The panel then assessed the quality of evidence of the results overall and categorized the recommendations according to the GRADE system (Grading of Recommendations Assessment, Development and Evaluation),21 which provides explicit, systematic classifications. Criteria taken into account in the process of evaluating the level of evidence were methodological shortcomings, consistency of results, generalizability of conclusions, and effect size. Once the literature had been assessed, recommendations were drafted based on the best available evidence, clinical experience, and applicability. The drafted recommendations were then classified and prioritized for implementation in rounds of discussion of the questions posed to the panel of experts.
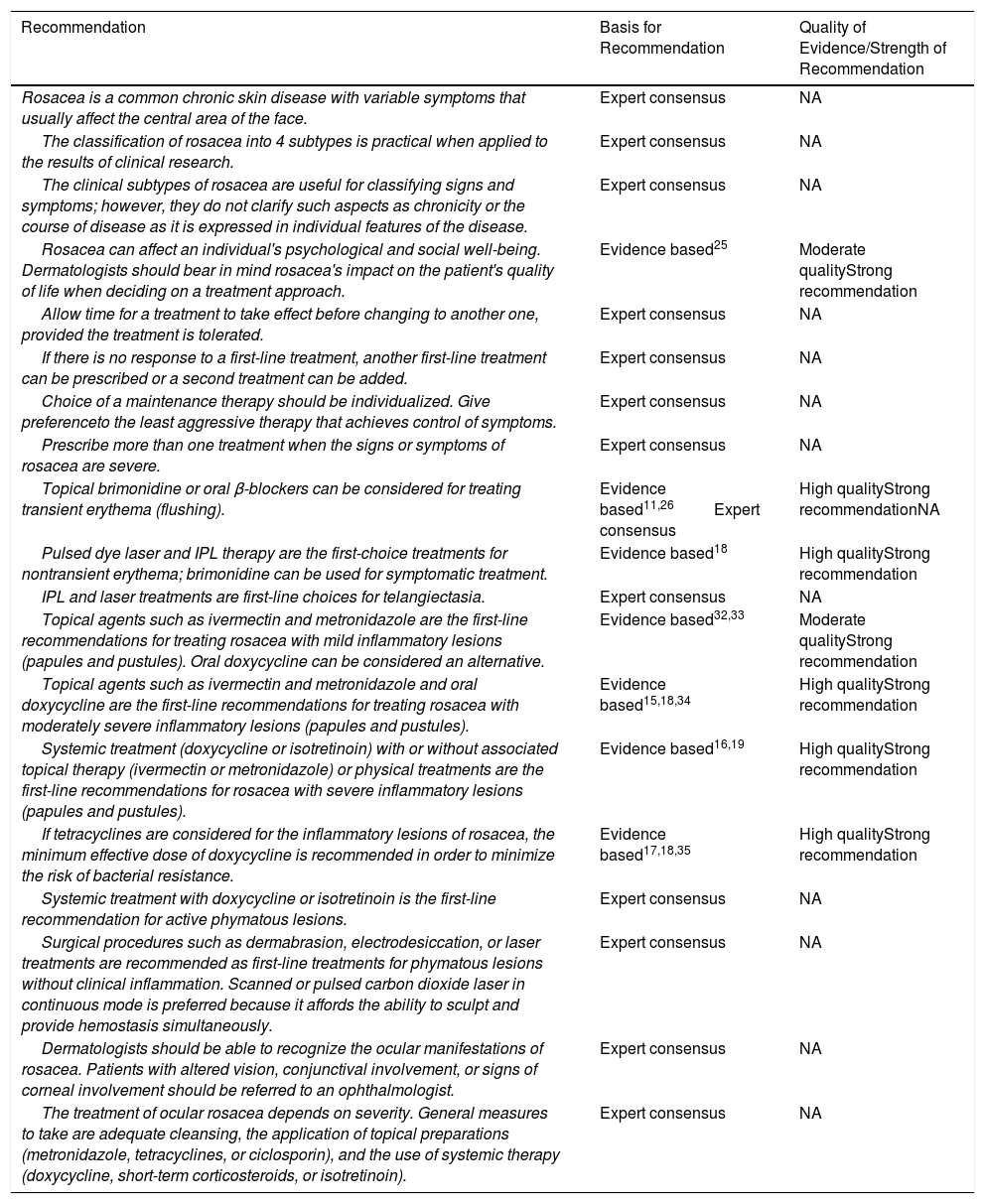
Procedures for Reaching ConsensusTwenty affirmations were grouped under 4 headings: a) definition of rosacea, b) impact on quality of life (QoL), c) therapeutic approach, and d) treatments. The panel of experts met for open discussion of all the proposed statements, debating each one individually and proposing improvements to incorporate into the final recommendations.
To facilitate the measurement of degree of consensus, the experts rated their agreement with each recommendation on a Likert scale.22 If at least 75% of them agreed or totally agreed with an item, consensus was assumed. In the first round of voting, consensus was reached on 17recommendations. On 8of them agreement was high. Two other items were validated by consensus after the second round of discussion and assessment. Thus, a total of 19recommendations and 4treatment algorithms, one for each subtype of rosacea, were approved (Fig. 1). (See Appendix BS1, online supplementary material, in Spanish.) Table 2 summarizes the consensus-based recommendations issued by the panel of experts after review of the available evidence.
Recommendations Issued by the Panel of Experts
| Recommendation | Basis for Recommendation | Quality of Evidence/Strength of Recommendation |
|---|---|---|
| Rosacea is a common chronic skin disease with variable symptoms that usually affect the central area of the face. | Expert consensus | NA |
| The classification of rosacea into 4 subtypes is practical when applied to the results of clinical research. | Expert consensus | NA |
| The clinical subtypes of rosacea are useful for classifying signs and symptoms; however, they do not clarify such aspects as chronicity or the course of disease as it is expressed in individual features of the disease. | Expert consensus | NA |
| Rosacea can affect an individual's psychological and social well-being. Dermatologists should bear in mind rosacea's impact on the patient's quality of life when deciding on a treatment approach. | Evidence based25 | Moderate qualityStrong recommendation |
| Allow time for a treatment to take effect before changing to another one, provided the treatment is tolerated. | Expert consensus | NA |
| If there is no response to a first-line treatment, another first-line treatment can be prescribed or a second treatment can be added. | Expert consensus | NA |
| Choice of a maintenance therapy should be individualized. Give preferenceto the least aggressive therapy that achieves control of symptoms. | Expert consensus | NA |
| Prescribe more than one treatment when the signs or symptoms of rosacea are severe. | Expert consensus | NA |
| Topical brimonidine or oral β-blockers can be considered for treating transient erythema (flushing). | Evidence based11,26Expert consensus | High qualityStrong recommendationNA |
| Pulsed dye laser and IPL therapy are the first-choice treatments for nontransient erythema; brimonidine can be used for symptomatic treatment. | Evidence based18 | High qualityStrong recommendation |
| IPL and laser treatments are first-line choices for telangiectasia. | Expert consensus | NA |
| Topical agents such as ivermectin and metronidazole are the first-line recommendations for treating rosacea with mild inflammatory lesions (papules and pustules). Oral doxycycline can be considered an alternative. | Evidence based32,33 | Moderate qualityStrong recommendation |
| Topical agents such as ivermectin and metronidazole and oral doxycycline are the first-line recommendations for treating rosacea with moderately severe inflammatory lesions (papules and pustules). | Evidence based15,18,34 | High qualityStrong recommendation |
| Systemic treatment (doxycycline or isotretinoin) with or without associated topical therapy (ivermectin or metronidazole) or physical treatments are the first-line recommendations for rosacea with severe inflammatory lesions (papules and pustules). | Evidence based16,19 | High qualityStrong recommendation |
| If tetracyclines are considered for the inflammatory lesions of rosacea, the minimum effective dose of doxycycline is recommended in order to minimize the risk of bacterial resistance. | Evidence based17,18,35 | High qualityStrong recommendation |
| Systemic treatment with doxycycline or isotretinoin is the first-line recommendation for active phymatous lesions. | Expert consensus | NA |
| Surgical procedures such as dermabrasion, electrodesiccation, or laser treatments are recommended as first-line treatments for phymatous lesions without clinical inflammation. Scanned or pulsed carbon dioxide laser in continuous mode is preferred because it affords the ability to sculpt and provide hemostasis simultaneously. | Expert consensus | NA |
| Dermatologists should be able to recognize the ocular manifestations of rosacea. Patients with altered vision, conjunctival involvement, or signs of corneal involvement should be referred to an ophthalmologist. | Expert consensus | NA |
| The treatment of ocular rosacea depends on severity. General measures to take are adequate cleansing, the application of topical preparations (metronidazole, tetracyclines, or ciclosporin), and the use of systemic therapy (doxycycline, short-term corticosteroids, or isotretinoin). | Expert consensus | NA |
Abbreviations: IPL, intense pulsed light; NA, not applicable.
Rosacea is a common chronic skin disease with variable symptoms that usually affect the convex areas in the center of the face (cheeks, chin, nose, and center of the forehead). This condition includes various cutaneous signs such as transient flushing, nontransient erythema, telangiectasia, edema, papules, pustules, ocular involvement, and phymatous changes. Most patients manifest only a few of these signs, but others may develop more than one manifestation of the disease simultaneously.23
Four forms, or subtypes, of rosacea are currently designated, as follows: 1, erythematotelangiectatic rosacea, 2, papulopustular rosacea, 3, ocular rosacea, and 4, phymatous rosacea. However, information about their signs and symptoms, the relations between the subtypes, and the potential for progression from one to another remains scant.24
The experts’ opinion was that although this classification system is clinically unconvincing it is practical for research.
Recommendations:
Rosacea is a common chronic skin disease with variable symptoms that usually affect the central area of the face.
The classification of rosacea into 4subtypes is practical when applied to the results of clinical research.
The clinical subtypes of rosacea are useful for classifying signs and symptoms; however, they do not clarify such aspects as chronicity or disease course in terms of individual clinical features.
Effect on QoLRosacea mainly affects the face and its impact on a patient's QoL is indisputable. All studies on QoL in rosacea have shown that patients feel embarrassment and anxiety.25 They may also experience lack of confidence, low self-esteem, a negative body image, and depression. Understanding the patient's view of QoL is extremely important for disease management and choosing an appropriate treatment. Knowledge of concomitant conditions, such as migraine or gastrointestinal disorders, will also influence choice of therapy.
It is important to bear in mind how long it will take for a treatment's active ingredient to take effect. The duration of treatment should also be taken into account. Finally, each medication's adverse effects must be watched for.1
The rosacea patient is sometimes anxious because of prior experiences with failed therapy or unsatisfactory outcomes. If the response comes slowly, the clinician must insist on waiting until a medication can take effect unless the patient cannot tolerate its adverse effects. Treating an outbreak of rosacea usually takes 6to 8weeks.
Although it is generally said that second-line treatments should only be used once first-line treatments prove insufficient, in fact there are several first-line treatments available and the expert panel found it difficult to agree on a scale of preferences for these topical therapies.
Recommendations:
Rosacea can affect an individual's psychological and social well-being. Bear in mind rosacea's impact on the patient's QoL when deciding how to approach treatment.
Allow time for a treatment to take effect before changing to another one, provided the treatment is tolerated.
If there is no response to a first-line treatment, another first-line treatment can be prescribed or a second-line treatment can be added.
Therapeutic approachRosacea should be treated according to subtype. When the subtype is diagnosed, a medication with appropriate active ingredients for that type should be selected. General advice for patients with rosacea includes gentle cleansing, frequent use of a moisturizer, and routine use of sunscreens with a protection factor between 30 and 50. These measures and the elimination or attenuation of aggravating factors of climate and diet, for example, are very important for managing common symptoms such as dryness, pruritus, or a burning sensation. Members of the panel of experts acknowledged them in discussion, although they were not specifically evaluated.
How is maintenance therapy approached? Is it always necessary? Is it provided only if the patient asks for it? The chronic nature of rosacea justifies the use of some type of maintenance therapy appropriate for the patient's course of disease. Some patients enter into remission and remain so for long periods, whereas others experience many relapses within short periods of time. A maintenance treatment can keep a patient free of lesions for between 1and 3years, depending on severity. Tailoring is necessary. The physician's attitude and recommendation will be relevant, but the final decision is the patient's. The goal is to reduce the likelihood of recurrence. Although a topical treatment is usually prescribed, the patient's preference must be considered.
A combination of topical and oral therapy is optimal in moderate to severe rosacea. Both the physician and patient's view of severity are relevant, along with how quickly the patient desires to see results.17)
Recommendations:
Choice of a maintenance therapy should be individualized. Give preference to the least aggressive therapy that achieves control of symptoms.
Prescribe more than one treatment when the signs or symptoms of rosacea are severe.
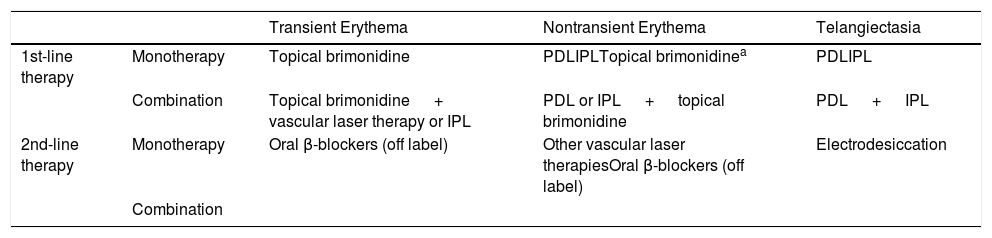
TreatmentErythema and telangiectasia: subtype 1 rosaceaFacial erythema, whether it is a constant, underlying presence (not transient) or appears occasionally either as a result of a clear trigger factor or without one (transient erythema, also known as flushing), is probably the most common feature of rosacea and one of the greatest concerns from the patient's point of view.
Erythema might respond sufficiently well to the application of topical α2 adrenergic receptor agonists, which induce the constriction of superficial vessels and attenuate underlyling erythema for several hours; however, they do not act on telangiectasia.17 Laser and other light therapies such as intense pulsed light (IPL) treatments can also be prescribed for erythema and are the main treatments for telangiectasia.17,18
Transient erythema (flushing).Topical brimonidine tartrate in a 0.5% gel formulation applied once daily in the morning has been evaluated in 2 randomized double-blind controlled trials (phase 3) that compared the active formulation to vehicle for the treatment of moderate to severe erythema in rosacea whether transient (flushing) or permanent.11,26 The trials demonstrated the formulation was effective in around 70% of patients. Onset of effect occurs about 30minutes after application. The peak effect is between 3 and 9hours later, and it decreases until it disappears at about 12hours. Brimonidine is therefore indicated to treat the facial redness of rosacea27,28 as a first-line option. However, even though it is considered the most significant advance in the treatment of transient erythema to date, it is poorly tolerated by some patients. Furthermore, it is important to note that brimonidine offers symptomatic, not definitive therapy for the disease, a point that is made in the summary of product characteristics.29
Laser and other light therapies (by themselves or in combination with brimonidine) continue to be the main options in the therapeutic arsenal against erythema,27,30 even though these physical treatments are more effective against telangiectasia and less effective against erythema. In particular, when known trigger factors are involved, light therapies only lead to partial improvement.
Flushing can also be treated with oxymetazoline 1% cream and oral clonidine, β-blockers (propranolol, carvedilol), naloxone or ondansetron. However, only limited evidence supports this use of these agents.28 The panel of experts supported the use of oral β-blockers and other antihypertensive drugs as off-label, second-line treatments for transient erythema.
Nontransient (permanent) erythema.Nontransient facial erythema in rosacea can respond to specific laser or other light therapies such as pulsed dye laser (PDL) and IPL,16 which have been shown to have similar effects.18 Brimonidine monotherapy as a symptomatic treatment for permanent erythema can also be a good choice.18 The panel of experts recommended combining PDL or IPL with brimonidine as a first line of therapy.
Some of the antihypertensive agents mentioned above can be used to treat permanent as well as transient erythema. β-blockers, which act as vasoconstrictors on cutaneous arteries by blocking the β2-adrenergic pathway, are used off label for erythema.31 The experts, who reported having only slight experience with these drugs, advised using vascular laser therapy first, saving oral β-blockers off label as a second-line option for permanent erythema.
TelangiectasiaBoth PDL and IPL treatments have beneficial effects on telangiectasia.30 These 2 types of light therapy are first-line treatment choices and can be used in combination.
The experts disagreed regarding the use of electrodesiccation on telangiectasia. If no other technique is available, it is possible to obtain good results with the electric scalpel in the right hands, although electrodesiccation is not generally considered to be a first-choice tool for this purpose. Therefore, the experts placed it among second-line treatments.
Recommendations:
Topical brimonidine or oral β-blockers can be considered for treating transient erythema (flushing).
PDL and IPL therapy are the first-choice treatments for nontransient erythema; brimonidine can be used for symptomatic treatment.
IPL and laser treatments are first-line choices for telangiectasia.
Table 3 summarizes the experts’ consensus on the treatment of erythematotelangiectatic rosacea (subtype 1).
Treatments for Erythema/Telangiectasia
| Transient Erythema | Nontransient Erythema | Telangiectasia | ||
|---|---|---|---|---|
| 1st-line therapy | Monotherapy | Topical brimonidine | PDLIPLTopical brimonidinea | PDLIPL |
| Combination | Topical brimonidine + vascular laser therapy or IPL | PDL or IPL + topical brimonidine | PDL + IPL | |
| 2nd-line therapy | Monotherapy | Oral β-blockers (off label) | Other vascular laser therapiesOral β-blockers (off label) | Electrodesiccation |
| Combination |
Abbreviations: IPL, intense pulsed light; PDL, pulsed dye laser.
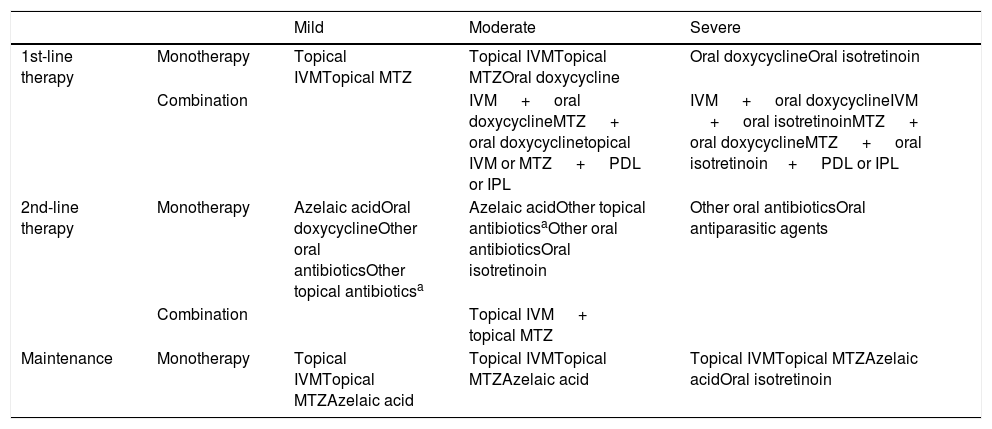
First-line treatments for mild inflammatory papulopustular lesions include topical ivermectin or metronidazole and oral doxycycline, although their efficacy is not exactly the same in this clinical setting.1
European and other international consensus statements include azelaic acid as a first-line treatment,17,18 but the expert panel reported that surveys of Spanish practitioners indicate that few of them consider this option first. Instead, they use it as a complementary therapy or a maintenance treatment between exacerbations. Therefore, they choose mainly between metronidazole and ivermectin.14,32 Sulfacetamide in association with a bisulfite is also routinely used in some countries, such as the United States, but these products are not available in Spain.
Dermatologists routinely use metronidazole and ivermectin based on their clinical experience and patient characteristics such as adherence to prescription, socioeconomic level, and health care coverage. One randomized investigator-blinded trial (phase2) with 960 patients found that ivermectin1% cream once daily was superior to metronidazole0.75% cream twice daily after 16weeks of treatment (83.0%vs 73.3%, P<.001) and that ivermectin's efficacy tended to improve with time, even in patients with more severe disease.32 Ivermectin's safety and tolerance profile was also superior to that of metronidazole in that study.
Stein Gold et al12 compared the safety of long-term use of ivermectin 1% cream and azelaic acid15% gel as maintenance treatments for papulopustular rosacea in 40-week investigator-blinded extensions of 2 prior phase-3 trials. They reported that more outcomes were recorded as “clear or almost clear” (investigator's global assessment) in the ivermectin group than in the azelaic acid group. Safety and tolerance during follow-up were also better in the ivermectin group.
Topical therapy is usually adequate for treating mild papulopustular rosacea. However, moderate to severe disease usually requires the addition of systemic therapy.17,19 Ivermectin, metronidazole, and azelaic acid were once again the first-line choices for papulopustular lesions and moderately intense perilesional erythema.17 Tetracyclines were also first-line options.
Some studies have evaluated metronidazole or azelaic acid in combination with oral doxycycline, finding that combined topical and systemic therapy is more effective than topical therapy alone, without causing a rise in adverse effects.14 Likewise, phase-3 studies have shown that an anti-inflammatory (subantimicrobial) doxycycline dose (40mg/d) can be used as a first-line treatment in monotherapy for papulopustular rosacea.34 In fact US and German guidelines recommend this approach for treating this subtype of the disease.15,18
Del Rosso et al17 compared the safety and efficacy of an anti-inflammatory dose of a slow-release formulation of doxycycline (40mg) versus an antimicriobial dose (100mg/d) over a period of 16weeks. The prospective, randomized controlled multicenter trial enrolled 96 patients and led to the conclusion that both doses were equally effective in treating severe rosacea, although an advantage of the lower dose was that it was associated with fewer adverse effects and did not contribute to the development of resistance.35 A US consensus report also concluded that resistance was avoided by prescribing the 40-mg dose.17
Controversy over antibiotic use in rosaceaThe controversy surrounding the use of antimicrobial doses (50–200mg) of tetracyclines versus an anti-inflammatory dose (40mg) was fully discussed during the consensus meeting.
Anti-inflammatory treatment is considered the most appropriate choice for managing rosacea, particularly the papulopustular form, given that rosacea is an inflammatory disease, not an infectious one. However, the panel of experts recognized that clinicians routinely continue to prescribe antibiotics at antimicrobial doses. Oral doxycycline (50–200mg/d) is still the most common prescription in cases that respond poorly to a reasonable trial period of topical treatment. Only occasionally is a subantimicrobial dose of doxycycline (40mg/d) prescribed.17 Minocycline (100mg/d) is another tetracycline that is widely used and has been shown to be effective in papulopustular rosacea.18 Other tetracyclines are also used in countries where they are available.
Patients who are allergic, intolerant, or resistant to tetracyclines or who have contraindications for their use (pregnancy or age under 10 years) can take macrolides such as erythromycin, clarithromycin, or azithromycin. Oral erythromycin at a dose of 250to 1000mg/d is considered highly effective, although due to adverse effects it is not usually recommended.18 Other macrolides are preferred.
Although international consensus tends to frown on the use of antimicrobial doses of antibiotics for rosacea,17,18 given that antibiotics are of interest solely for their anti-inflammatory effect, which can be achieved with a low dose (40mg in the case of doxycycline), this panel of experts insisted that a dose of 100mg was more effective in their experience and that the ideal approach would probably be to prescribe high doses of tetracyclines at the start of treatment and a low dose (40mg/d) for maintenance. Fewer adverse effects (such as candidiasis or the development of resistance) are associated with the lower dose. The experts indicated that although this approach was the most recommendable, it did not always coincide with clinical practice.
Severe cases of rosacea, or refractory ones after a trial of standard therapy, can be treated with oral isotretinoin, whose efficacy in severe rosacea has been demonstrated.19 Once poor adherence to other therapies has been ruled out in patients with papulopustular rosacea refractory to treatment, oral isotretinoin can be prescribed17 at lower doses (0.25mg/kg/d) than those indicated for acne. A difference, however, is that isotretinoin attenuates rosacea activity while it is being taken but does not cure the condition as it does acne.
Finally, laser therapies (eg, with PDL and neodymium-YAG [yttrium-aluminum-garnet]) and IPL treatments are effective in severely and persistently dilated superficial blood vessels that do not respond to medications used to treat papules and pustules.16 This approach addresses both linear telangiectasia and more confluent networks of vessels.
Recommendations:
Topical agents such as ivermectin and metronidazole are the first-line recommendations for treating rosacea with mild inflammatory lesions (papules and pustules). Oral doxycycline can be considered an alternative.
Topical agents such as ivermectin and metronidazole and oral doxycycline are the first-line recommendations for treating rosacea with moderately severe inflammatory lesions (papules and pustules).
Systemic treatment (doxycycline or isotretinoin) with or without associated topical therapy (ivermectin or metronidazole) or physical treatments are the first-line recommendations for rosacea with severe inflammatory lesions (papules and pustules).
If tetracyclines are considered for the inflammatory lesions of rosacea, the minimum effective dose of doxycycline is recommended in order to minimize the risk of bacterial resistance.
Table 4 summarizes the experts’ consensus on the treatment of papulopustular rosacea (subtype 2).
Treatments for Papulopustular Rosacea
| Mild | Moderate | Severe | ||
|---|---|---|---|---|
| 1st-line therapy | Monotherapy | Topical IVMTopical MTZ | Topical IVMTopical MTZOral doxycycline | Oral doxycyclineOral isotretinoin |
| Combination | IVM + oral doxycyclineMTZ + oral doxycyclinetopical IVM or MTZ + PDL or IPL | IVM + oral doxycyclineIVM + oral isotretinoinMTZ + oral doxycyclineMTZ + oral isotretinoin+ PDL or IPL | ||
| 2nd-line therapy | Monotherapy | Azelaic acidOral doxycyclineOther oral antibioticsOther topical antibioticsa | Azelaic acidOther topical antibioticsaOther oral antibioticsOral isotretinoin | Other oral antibioticsOral antiparasitic agents |
| Combination | Topical IVM + topical MTZ | |||
| Maintenance | Monotherapy | Topical IVMTopical MTZAzelaic acid | Topical IVMTopical MTZAzelaic acid | Topical IVMTopical MTZAzelaic acidOral isotretinoin |
Abbreviations: IPL, intense pulsed light; IVM, ivermectin; MTZ, metronidazole; PDL, pulsed dye laser.
Active phymatous lesions (with inflammation)
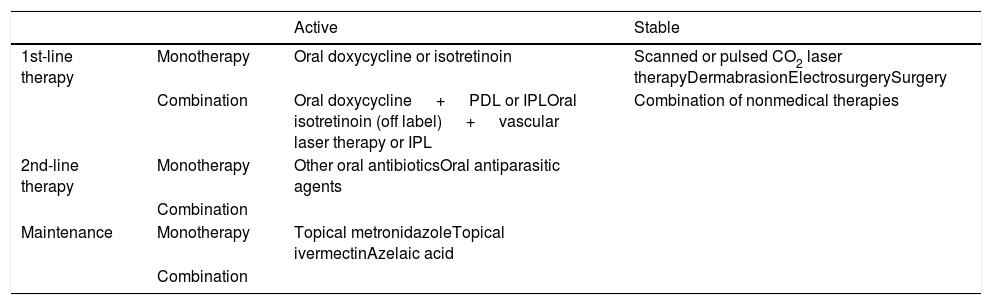
Both doxycycline and isotretinoin have proven effective in the treatment of active phymatous rosacea.15,19 Isotretinoin is prescribed at low doses (0.1–0.5mg/kg/d) for 6to 8months19,36 and has been shown to have the potential to slow phymatous progression.37 Some of these cited authors have thought that combinations of laser vascular surgery, doxycycline, and isotretinoin can be beneficial when more than one subtype of rosacea is present. Good results have also been reported for IPL therapy in clinical trials according to one update.30
The panel of experts recommended combining vascular laser or IPL treatments with oral doxycycline or isotretinoin (off label) in patients with active phymatous rosacea. Other oral antibiotics or antiparasitic agents (metronidazole and others) are second-line treatments, according to the experts.
A maintenance regimen should be prescribed to prevent the reemergence of symptoms. The panel of experts advised using topical agents such as ivermectin, metronidazole, and azelaic acid.
Stable or inactive phymatous rosacea.The evidence suggests that phymatous changes should be treated with physical (surgical or laser) therapies.16,18 No definitively effective medical treatment is available for fully developed phymatous changes in rosacea. However, this form of the disease is routinely managed with the aforementioned therapies, which are sometimes used in combination with tangential excision and dermabrasion. Certain options — such as the electric scalpel and electrosurgery, laser ablation, and scissor sculpting — have been abandoned.16,18
Recommendations:
Systemic treatment with doxycycline or isotretinoin is the first-line recommendation for active phymatous lesions.
Surgical procedures such as dermabrasion, electrodesiccation, or laser treatments are recommended as first-line treatments for phymatous lesions without clinical inflammation. Scanned or pulsed carbon dioxide laser in continuous mode is preferred because sculpting and hemostasis can be accomplished simultaneously.
Table 5 summarizes the experts’ consensus on the treatment of phymatous rosacea (subtype 3).
Treatments for Phymatous Rosacea.
| Active | Stable | ||
|---|---|---|---|
| 1st-line therapy | Monotherapy | Oral doxycycline or isotretinoin | Scanned or pulsed CO2 laser therapyDermabrasionElectrosurgerySurgery |
| Combination | Oral doxycycline + PDL or IPLOral isotretinoin (off label) + vascular laser therapy or IPL | Combination of nonmedical therapies | |
| 2nd-line therapy | Monotherapy | Other oral antibioticsOral antiparasitic agents | |
| Combination | |||
| Maintenance | Monotherapy | Topical metronidazoleTopical ivermectinAzelaic acid | |
| Combination |
Abbreviations: IPL, intense pulsed light; PDL, pulsed dye laser.
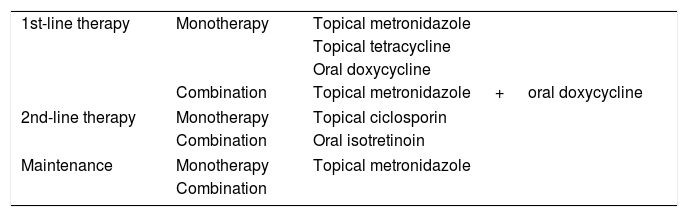
Ocular involvement develops in 30% to 50% of patients with rosacea. Local ophthalmologic treatment may be sufficient in mild cases. Cleansing the edges of the eyelids is an option, as is the use of artificial tears containing lipids.18
Some agents (topical corticosteroids, metronidazole 0.75%, and ciclosporin 0.05% twice daily) have proven effective in reducing local ocular inflammation in this type of rosacea.18 When eye symptoms persist, doxycycline (50–100mg, twice daily or at an anti-inflammatory dose of 40mg/d) have given good results.15,18 Low-dose isotretinoin (10mg/d) also improves ocular symptoms.19
According to the panel of experts, neither ciclosporin nor short-term corticosteroid regimens are much used to treat ocular rosacea in Spain. The specialists preferred topical metronidazole and tetracyclines or oral tetracyclines.
The dermatologists thought that they might enter into conflict with ophthalmologists in the treatment of ocular rosacea, and meetings between the 2 types of specialists could be advisable. Patients with mild ocular rosacea are currently treated by dermatologists, whereas those with moderate to severe symptoms are referred to ophthalmologists.
Recommendations:
Dermatologists should be able to recognize the ocular manifestations of rosacea. Patients with altered vision, conjunctival involvement, or signs of corneal involvement should be referred to an ophthalmologist.
The treatment of ocular rosacea depends on severity. General measures to take are adequate cleansing, the application of topical metronidazole, tetracyclines, or ciclosporin), and systemic therapy (doxycycline, short-term corticosteroids, or isotretinoin).
Table 6 summarizes the experts’ consensus on the treatment of ocular rosacea (subtype 4).
Treatments for Ocular Involvement in Rosaceaa
| 1st-line therapy | Monotherapy | Topical metronidazole |
| Topical tetracycline | ||
| Oral doxycycline | ||
| Combination | Topical metronidazole + oral doxycycline | |
| 2nd-line therapy | Monotherapy | Topical ciclosporin |
| Combination | Oral isotretinoin | |
| Maintenance | Monotherapy | Topical metronidazole |
| Combination | ||
A general limitation of the Delphi method is that consensus about various clinical scenarios can be biased by participants’ experience in medical practices where they work. However, the subjective opinion of a panel of experts will always offer higher quality guidance than the opinion of a single specialist, given that the group can pool more information. The literature search to find available evidence for this report was not systematic. Rather it was directed by the clinical questions proposed by the coordinator. Furthermore, articles published after 2016 were not included. Therefore, it is possible that new studies may have changed some of the therapeutic suggestions for rosacea.
ConclusionsRosacea is treated according to the severity of the clinical presentation (signs and symptoms), in which the features of different subtypes of the disease are often found in combination. Along with general measures for cleansing and hydrating the skin, the dermatologist usually offers a combination of pharmacologically active agents, as described in this paper. Specialists are increasingly more aware of the impact of rosacea on quality of life, leading them to involve the patient in therapeutic decision-making.
FundingGalderma helped to fund the meeting of the panel of experts. This pharmaceutical laboratory did not participate in the writing of the article.
Conflicts of InterestMonserrat Salleras has worked with Galderma to coordinate and participate in meetings to reach consensus on the treatment of rosacea. She was also a speaker during the launch of brimonidine and has given talks to provide updated information on rosacea for dermatology teams at Hospital Universitario Sagrat-Cor. She has also received funding for travel to and registration for dermatology conferences. Regarding the preparation of this article, she declares that she has no conflicts of interest related to the treatments proposed, which she defends exclusively based on her clinical experience. Marta Alegre has been a speaker for Galderma twice; she has also served on 2 Galderma advisory boards. Vicent Alonso Usero, Pablo Boixeda, and Jesús Domínguez Silva declare that they have no conflicts of interest related to Galderma. Jesús Fernández Herrera has been a speaker for Galderma; he declares that he has no other conflicts of interest. He has not participated in clinical trials or received funding for travel to or registration for dermatology conferences; nor has he received research grants. Xavier García Navarro declares that he has no conflicts of interest related to Galderma. Natalia Jiménez declares that she served on 2 Galderma advisory boards. Mar Llamas has been a speaker for Galderma on occasion. She has no other conflicts of interest to declare in relation to the rosacea treatments discussed in this consensus paper. She has not participated in clinical trials for Galderma or received funding for travel to or registration for dermatology conferences; nor has she received research grants. Cristina Nadal spoke at a meeting organized by Galderma and served on an advisory board to reach consensus regarding rosacea. Jesús del Pozo Losada declares that he has no conflicts of interest. Ignacio Querol and Irene Salgüero declare that they have no conflicts of interest in relation to Galderma. Martin Schaller has served on advisory boards organized by Bayer, Galderma, and Marpinion within the last 2years. He has also received speaker's fees from AbbVie, Bayer Healthcare, Galderma, and La Roche-Posay. Jorge Soto de Delás has been a speaker for Galderma; he declares that he has not participated in trials of Galderma's products. Nor has he received funding for travel to or registration for dermatology conferences or been awarded research grants.
Please cite this article as: Salleras M, Alegre M, Alonso-Usero V, Boixeda P, Domínguez-Silva J, Fernández-Herrera J, et al. Documento de consenso español para el algoritmo de tratamiento de la rosácea. Actas Dermosifiliogr. 2019;110:533–545.