A 52-year-old woman who had undergone a hysterectomy at the age of 35 due to uterine myomas, presented with an extremely painful nodule on her right shoulder of 1 year duration.
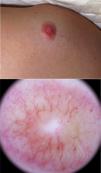
Physical examinationAn erythematous and tender nodule of 20 mm on the right scapular region (Fig. 1) was observed. Dermoscopy revealed a white central area with a peripheral crown of serpiginous vessels over a red-yellowish background.
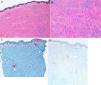
Diagnostic testsA punch skin biopsy was performed and histologic study (Fig. 2A–B) and immunohistochemistry (Fig. 2C. Desmin; 2D. S100; 2E. Ki67) was carried out.
What is your diagnosis?
DiagnosisPilar leiomyoma, multiple cutaneous and uterine leiomyomatosis (or Reed syndrome).
Evolution and treatmentThe lesion was excised. Histopathological study showed an ill-defined proliferation of intermingled smooth muscle bands without atypia. No mitotic activity or necrosis was observed in the dermis. On immunohistochemistry, the tumor was positive for desmin, weakly positive for actin and Ki67, and negative for CD34 and S-100 (Fig. 2A–E). A diagnosis of pilar leiomyoma was made. On further questioning, the patient revealed a family history of multiple cutaneous leiomyomas (mother, brother and sister) and uterine leiomyomatosis (mother and sister). The patient fulfilled the clinical diagnostic criteria for multiple cutaneous and uterine leiomyomatosis (MCUL) or Reed Syndrome1. A renovesical ultrasound was performed, in order to rule out an associated renal neoplasm, showing a radiologically benign lesion (angiomyolipoma). Ultrasonographic follow-up every 6 months was then indicated and the patient, referred to the Urology and the Genetic department. The patient was lost to follow-up.
DiscussionPilar leiomyomas (PL) are infrequent benign smooth muscle tumors arising from the arrector pili muscle of hair follicles. Within the group of cutaneous leiomyomas, PL constitute the most common subtype. PL usually present as painful erythematous-brownish papulonodules and can present as solitary or multiple lesions (myomatosis cutis miliaris)2. Almost 50% of the PL cause a sharp or burning pain. On dermoscopy, PL can present with a delicate pink-brown pigmented network and irregular crypts with white cloud-like areas and peripheral branching vessels3, although unfocused arborizing telangiectasias have been described in more than 10% of tumors4.
PL have been reported in association with multiple disorders such as esophageal leiomyomas, chronic lymphocytic leukemia and HIV. PL can also be secondary to an autosomal dominant inherited familial syndrome: MCUL or Reed syndrome. Main characteristics of MCUL are the presence of cutaneous leiomyomas (mainly PL), uterine leiomyomas in women (73–100%) and renal cell carcinoma (20–34%). Clinical diagnostic criteria include multiple cutaneous leiomyoma (with histologic confirmation of one of the lesions) or a biopsy-proven solitary cutaneous leiomyoma plus family history of Reed syndrome1. MCUL is caused by a heterozygous mutation (1q42.3-q43) in the fumarate hydratase gene (FH), a Krebs cycle enzyme, but may also act as a tumor suppressor5. PL present in patients with MCUL by the age of 40, and generally constitute the first manifestation of the syndrome and their most sensitive and specific clinical marker6. Uterine leiomyomas are developed earlier than in healthy individuals, usually requiring hysterectomy.
The most worrying association of MCUL is with renal cell carcinoma (RCC), which occurs in up to 30% of patients. RCC in this context tend to be aggressive, with early nodal dissemination and metastases. Abdominal MRI is recommended every 6–12 months, since small tumors could not be detected by ultrasound and can have a high dissemination potential7. Genetic testing should be offered, if available, in order to avoid unnecessary imaging in case of negative results.
PL can be associated with MCUL and RCC. Dermatologists should be aware of the potentially life-threatening consequences of a delayed diagnosis.