In diabetic foot syndrome, a series of complications of late-stage diabetes affect the foot. These complications, which culminate in foot amputation, include peripheral vascular disease and neuropathy, Charcot arthropathy, plantar ulceration, and osteomyelitis. In recent years, the medical community has paid greater attention to diabetic foot syndrome, and our understanding of its pathophysiology and management has advanced. Although the podiatrist is charged with caring for the diabetic foot, as dermatologists we occasionally act as consultants. This review therefore offers dermatologists an update on the causes and management of skin lesions in the diabetic foot.
El síndrome del pie diabético engloba una serie de alteraciones que pueden presentar los pies de las personas con diabetes mellitus avanzada. Estas alteraciones incluyen la vasculopatía y la neuropatía periférica, la neuroartropatía de Charcot, las úlceras plantares, la osteomielitis y la complicación final de estos procesos: la amputación del miembro inferior.
En los últimos años ha existido una mayor atención por parte de la comunidad médica al síndrome del pie diabético. Se han realizado avances en el entendimiento de su fisiopatología, así como en su manejo. Aunque el pie diabético es un campo de trabajo de los podólogos, los dermatólogos ejercemos de forma ocasional de consultores en algunos de estos casos. Por este motivo el presente artículo pretende ofrecer a los dermatólogos una herramienta de actualización en las causas y el manejo de las lesiones del pie diabético.
Diabetes is undoubtedly one of our most significant health problems, not only because of its high prevalence but also because of its considerable socioeconomic impact. One of the most feared complications of diabetes mellitus is the so-called diabetic foot. This syndrome is not an entity in itself, but rather encompasses a series of complications that may develop in the feet of patients with advanced diabetes. These complications include peripheral vascular disease and neuropathy, Charcot arthropathy, plantar ulceration, and osteomyelitis. Also included within the syndrome would be the final complication of these processes: lower-limb amputation.1
Greater attention has been focused on diabetic foot by the medical community in recent years, and there have been advances in our understanding of the pathophysiology and management of this condition. Although the podiatrist is generally charged with caring for the diabetic foot, as dermatologists we should also be able to recognize and manage it. The objective of this review, therefore, is to offer an update on everything the dermatologist needs to know when examining the feet of a diabetic patient.
EpidemiologyDiabetes mellitus affects approximately 7.8% of the Western population, although up to one quarter of the actual cases remain undiagnosed. Its prevalence increases with age and up to 23% of those over the age of 60 years are affected.2 In Spain, 8% of women and 12% of men have diabetes.3About 4% of patients with diabetes mellitus develop lower-limb ulcers,4 and the prevalence is higher (between 5% and 7%) in patients with associated neuropathy.5,6 Thus, for diabetic patients, the cumulative risk of developing foot ulcers at some time in their lives is as high as 15%.7 More than 60% of nontraumatic lower-limb amputations occur in diabetic patients, and the amputations are preceded by ulceration in 85% of these patients.8,9 The outcome for diabetic amputees is poor: 30% die during the year following the intervention, and by 5 years later, half of patients have undergone contralateral limb amputation.10 Efforts have therefore been made to reduce the incidence of plantar ulceration in order to reduce the number of amputations. However, the results of the most recent studies have been inconsistent in demonstrating real success in the reduction of plantar ulceration.11–14
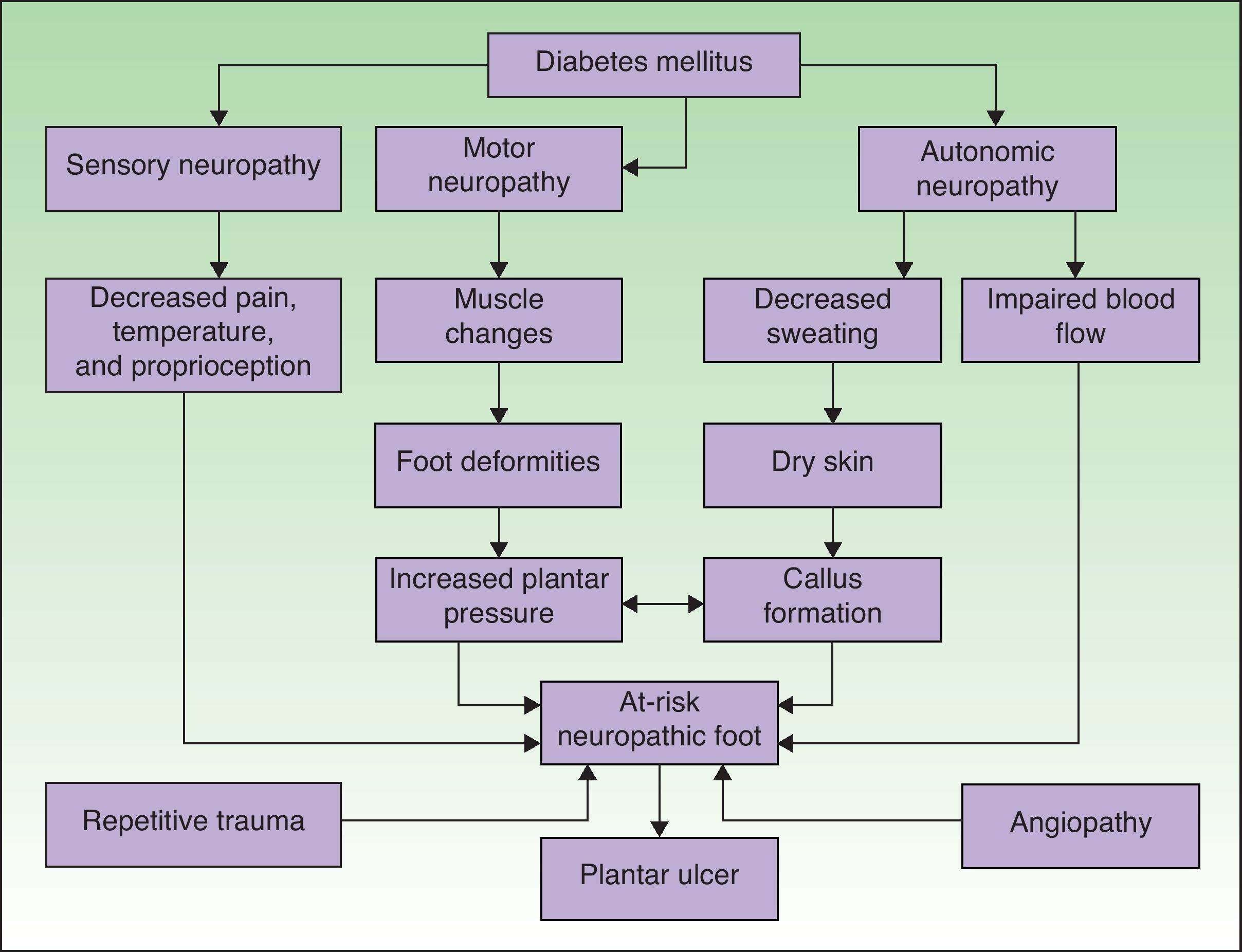
PathophysiologyAn understanding of the pathophysiology of so-called diabetic foot is essential for optimal management. There are numerous factors that may favor the development of a plantar ulcer in the diabetic patient (Fig. 1).15 Neuropathy and macroangiopathy are the 2 main causal mechanisms, while injuries are often the events that precipitate an acute lesion.16 If we can act on these factors, we can prevent the formation of a plantar ulcer or restore the skin once the ulcer has appeared.
Pathophysiological mechanisms of ulceration in the diabetic foot. Adapted from Boulton.15 Neuropathy and vascular disease are the 2 most important factors in the development of diabetic foot ulcers.
Between 60% and 70% of diabetic patients have some form of neuropathy. The most common forms are distal symmetric polyneuropathy, delayed esophageal transit, carpal tunnel syndrome, and erectile dysfunction. It appears that peripheral nerve damage in diabetic patients is due to the metabolic disorders caused by sustained hyperglycemia, while ischemia involving the vasa nervorum worsens this situation.17
Distal symmetric polyneuropathy in a stocking distribution is the type of neuropathy that most frequently predisposes to foot ulceration. The risk of developing a plantar ulcer is 7 times greater in the presence of this chronic and insidious neuropathy, whose frequency increases as diabetes progresses. In patients with distal symmetric neuropathy, autonomic, sensory, and motor nerves are affected. Small nerve fibers are the first to be damaged, producing a loss of sensitivity to pain and temperature. Subsequently, damage to the larger nerve fibers leads to a loss of vibratory and surface sensitivity. As a result of this damage, diabetics do not perceive foot lesions caused by repetitive trauma or by foreign bodies.
Motor neuropathy produces atrophy and weakness in foot muscles, with the loss of the stabilizing function of the interphalangeal and metatarsophalangeal joints. There is a dynamic contraction of the long extensors and flexors that leads to protrusion of the metatarsal heads, a condition commonly known as claw or hammer toes. In this abnormality there is an increase in plantar pressure under the toes and the metatarsal heads.18
Autonomic neuropathy involving damage to postganglionic nerve fibers that innervate the sweat glands leads to anhydrosis, which in turn often leads to extreme dryness of the foot and to the appearance of cracks or fissures that can act as a route of entry for infectious agents. Autonomic neuropathy also causes severe impairment of foot microcirculation. The regulation of arteriovenous communications depends on sympathetic innervation and neuropathy results in a permanent opening of these communications, leading to poor flow regulation.19 One of the challenges in the education of patients with diabetic foot is to convey to them that a foot that is neither painful nor cold is nevertheless a foot at risk.20 Increased plantar pressure as well as edema in the lower extremities are also usually present in diabetic patients with autonomic neuropathy.21
In clinical practice neuropathy can be evaluated using a tuning-fork (for large nerve fibers); tubes of hot or cold water, and needles (for small nerve fibers); and by assessing the Achilles tendon reflex. The method most often used to assess diabetic neuropathy is, however, the use of Semmes-Weinstein monofilaments to evaluate sensitivity to pressure.22 The technique consists of applying a 10-g monofilament to 3 points on the sole of the patient's foot —under the large toe and the heads of the first and fifth metatarsals—as well as at the edge of the ulcer or callus. The monofilament is applied on 2 occasions with enough force to bend it for 2seconds. The patients are then asked whether they feel the pressure and where they feel the contact. These applications should be alternated on occasion with a sham application, during which no pressure is applied and the patient is asked again. Protective sensation is considered to be absent, leaving the patient at risk for ulcer formation, when 2 of every 3 responses are incorrect.23
Vascular DiseaseSo-called diabetic microangiopathy is, after all, a form of atherosclerosis that affects patients with diabetes. Peripheral vascular disease is between 2.5 and 6 times more frequent in diabetic patients. It also develops at an earlier age in diabetics and its frequency increases as diabetes progresses: 45% of diabetics diagnosed 20 years earlier have this condition.24 Those patients with other risk factors for atherosclerosis (hypertension, smoking, dyslipidemia) are at still greater risk and their mortality rate is higher. Vascular disease caused by diabetes affects more distal vessels than does nondiabetic vasculopathy and has a poorer prognosis with respect to amputation and mortality.25 A multicenter study concluded that vascular disease in the form of distal arteriopathy was present in 35% of patients with plantar ulceration.16
Increase in Plantar PressureAs has been mentioned earlier, motor disorders produce deformities in the feet of diabetic patients. Hammer toes lead to an increase in plantar pressure in certain areas under the toes and metatarsal heads.18 Limited joint mobility caused by motor neuropathy also contributes to an increase in plantar pressure.
Several studies have related increased plantar pressure to the risk of developing plantar ulcers. In a prospective study in 86 diabetic patients at a mean of 17 years from diagnosis, plantar ulcers occurred in 35% of patients with increased plantar pressure, while those with normal plantar pressure had no lesions.26 Later studies have confirmed these findings, determining that the risk of developing a plantar ulcer is 4.7 times greater if plantar pressure is elevated.27,28 The areas of the skin located under the toes and the metatarsal heads are, therefore, the areas at greatest risk for ulcers (Figs. 2 and 3).
Changes in the biomechanics of foot function produce increased pressure on certain areas and friction on walking that can eventually lead to the formation of a corn or callus. A callus is a hyperkeratotic skin lesion of uniform thickness with a wide base that has lost its physiological capacity to protect the foot, thus increasing problems related to neuropathy, such as a decrease in nociceptive sensation.29
Callus formation is related to increased plantar pressure and is therefore also associated with higher risk of developing an ulcer. The callus itself, however, also raises plantar pressure30 and is a point of vulnerability in the diabetic foot. As the callus lacks elasticity and is subjected to significant pressure, it can easily erode and blister, furthering the likelihood of ulcer formation. The relative risk of ulceration beneath a callus is 11 times greater than in other areas of the foot, and if there had already been an ulcer at the site, the risk rises to more than 50-fold. The formation of the callus depends not only on the presence or absence of neuropathy; other factors such as the age of the patient and the type of footwear used are also very important.31
If the excessive pressure on the callus is eliminated, it can heal. However, patients with neuropathy often fail to discover the callus at an early stage because they do not feel the pain; this makes healing much more difficult. Regular foot care and the elimination of calluses have been shown to reduce plantar pressure and the risk of ulcer formation.32
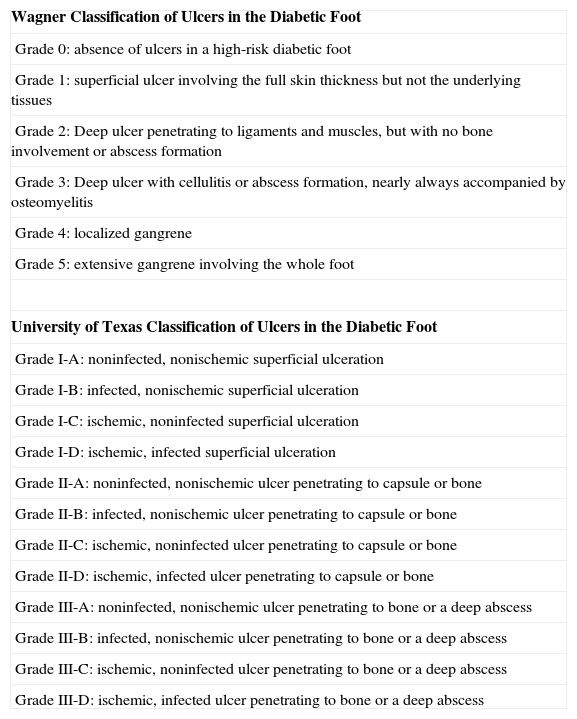
Ulcers in the Diabetic FootClassificationIt is difficult to manage ulcers in the diabetic foot without a standardized classification system. There are numerous existing classifications, but none is universally accepted. At present, all classifications consider only the state of the foot, without taking into account other factors with clear prognostic implications, such as the patient's age, time since the onset of diabetes, or the comorbidities the patient might present.
The Wagner system, which classifies an ulcer according to its depth and the extent of gangrene, is perhaps the most widely used.33 The University of Texas classification system takes into account the depth of the ulcer, as well as the presence or absence of infection and ischemia, but does not assess the diameter of the lesion or the presence of neuropathy.34,35 The details of these 2 classification systems are shown in Table 1. The classification system known as SAD considers 5 different aspects of each lesion encompassing size (depth and area), sepsis (presence or absence), arteriopathy, and neuropathy.36 These same aspects are evaluated in the PEDIS system proposed by the international Working Group of the Diabetic Foot.37
Wagner and University of Texas Classification Systems for Diabetic Foot Ulcers.
| Wagner Classification of Ulcers in the Diabetic Foot |
| Grade 0: absence of ulcers in a high-risk diabetic foot |
| Grade 1: superficial ulcer involving the full skin thickness but not the underlying tissues |
| Grade 2: Deep ulcer penetrating to ligaments and muscles, but with no bone involvement or abscess formation |
| Grade 3: Deep ulcer with cellulitis or abscess formation, nearly always accompanied by osteomyelitis |
| Grade 4: localized gangrene |
| Grade 5: extensive gangrene involving the whole foot |
| University of Texas Classification of Ulcers in the Diabetic Foot |
| Grade I-A: noninfected, nonischemic superficial ulceration |
| Grade I-B: infected, nonischemic superficial ulceration |
| Grade I-C: ischemic, noninfected superficial ulceration |
| Grade I-D: ischemic, infected superficial ulceration |
| Grade II-A: noninfected, nonischemic ulcer penetrating to capsule or bone |
| Grade II-B: infected, nonischemic ulcer penetrating to capsule or bone |
| Grade II-C: ischemic, noninfected ulcer penetrating to capsule or bone |
| Grade II-D: ischemic, infected ulcer penetrating to capsule or bone |
| Grade III-A: noninfected, nonischemic ulcer penetrating to bone or a deep abscess |
| Grade III-B: infected, nonischemic ulcer penetrating to bone or a deep abscess |
| Grade III-C: ischemic, noninfected ulcer penetrating to bone or a deep abscess |
| Grade III-D: ischemic, infected ulcer penetrating to bone or a deep abscess |
To date, there have been no large randomized clinical trials that can provide a solid scientific basis for managing ulcers in the diabetic foot.38 As a result, the approach to management varies from one hospital to another and is determined by the health care professional's own preferences and the availability of some techniques.39 Nevertheless, all the protocols share the common points described below.
Initial Evaluation of the PatientThe initial evaluation of the diabetic patient with a foot ulcer includes a manual blood count, coagulation tests, biochemistry with lipid and liver function profiles, determination of glycated hemoglobin levels,40 erythrocyte sedimentation rate, thyroid stimulating hormone levels, and prealbumin levels in the blood. Microalbumin levels in urine are also determined.
The evaluation of vascular disease is performed by palpating the dorsalis pedis pulses. In patients in whom these pulses cannot be palpated, the ankle-brachial index is determined noninvasively41 by dividing the systolic blood pressure of the ankle by that of the arm. A normal value approaches 1 (>0.90). An index less than 0.5 is considered indicative of severe arterial disease and the patient should be referred to a vascular surgeon.
Smokers are advised to quit because smoking reduces the supply of oxygen to the ulcer and delays healing.42
Assessing the Presence of InfectionWhile infections are not the cause of plantar ulcers, they can often make management more difficult and delay healing.43 An ulcer should therefore always be evaluated for infection before treatment is initiated.
The solution of continuity of the skin of an ulcer provides a point of entry for microorganisms. In addition, the impaired qualitative and quantitative white blood cell response in the diabetic patient facilitates the progression of the infection.44
From a clinical standpoint, infections can be classified as follows40,45:
- •
Mild infections are those that do not represent a threat to the extremity. Signs of systemic infection are absent. This category includes superficial infections and cellulitis with an extension of less than 2cm.
- •
Moderate or severe infections represent a risk to the affected extremity. They include larger cellulitis infections and deep ulcers that are generally accompanied by osteomyelitis. These infections require hospitalization and systemic treatment.
- •
Very severe infections have systemic effects, including hemodynamic instability. This category includes massive cellulitis, necrotizing fasciitis, and myonecrosis. Such infections require emergency surgery.
Cellulitis infections in a well-perfused extremity can be easily recognized by the considerable inflammation present, but their diagnosis can be more difficult in an ischemic limb. Osteomyelitis, which is present in 10% to 20% of mild infections and 50% to 60% of severe infections, is produced by direct contiguity as the soft-tissue infection penetrates the structures. Magnetic resonance imaging is currently the best technique for the diagnosis of osteomyelitis.46
The microorganisms that cause infections in the diabetic foot come from the patient's own skin and intestinal flora. Mild and superficial diabetic foot infections are usually caused by Staphylococcus aureus and Streptococcus pyogenes, whereas deep ones are polymicrobial, involving gram-positive cocci (S areus and S pyogenes), enterobacteria, and anaerobes (Peptostreptococcus species and Bacteroides species). In ulcers previously treated with antibiotics or in hospitalized patients, it is common to find methicillin-resistant S aureus or enterobacteria that produce extended-spectrum β-lactamase.
Offloading the ExtremityResting the affected extremity and reducing pressure on the foot when walking are perhaps the most important interventions to promote the healing of ulcers in the diabetic foot. In this way it is possible to avoid recommending the technically impossible immobilization of the foot long enough for the ulcer to heal. Moreover, immobilization would also entail certain risks, such as thrombosis, muscle atrophy, depression, and the formation of ulcers in other locations. For this reason, various orthopedic devices have been designed to allow the patient to maintain a certain degree of activity while offloading the extremity. The scientific evidence showing that offloading facilitates the healing of a foot ulcer has been obtained mainly from studies of uninfected neuropathic ulcers in which braces were used for complete offloading.47,48 However, these devices tend to be uncomfortable and for this reason many patients do not use them, especially while at home.49 Devices that the patient cannot remove, although less comfortable, have been shown to be more effective.50
DebridementAnother essential measure in the treatment of diabetic foot ulcers is the surgical removal of nonviable tissue. This procedure reduces the bacterial load in the wound as well as the proinflammatory products generated. A multicenter study demonstrated that periodic debridement increases the rate of healing in diabetic patients.51 Although debridement techniques vary from one center to another, it seems clear that adequate debridement must include all the necrotic tissue, the infected tissue, and the surrounding callus area, until an edge of healthy and well-vascularized tissue is achieved.52,53 The procedure should be performed with extreme care, especially in patients with ischemic feet, and should be done before any dressing is applied. Debridement causes the activation of the platelets that will control bleeding and release growth factors that initiate healing.54
Local Wound CareAfter debridement, the wound should be kept moist to facilitate angiogenesis and the synthesis of connective tissue.55 In recent years many new types of dressings have been developed. The choice of dressing depends on the location of the ulcer, its depth, the amount of exudate, the presence of bacterial contamination, etc, and should be reassessed regularly given that wound characteristics will change over time.
In torpid ulcers that fail to respond to the usual therapies, other treatments, such as negative pressure wound therapy56 or the topical application of growth factors, can be used.57
The important roles played by various endogenous growth factors (such as platelet-derived growth factor, transforming growth factor-β, basic fibroblast growth factor, epidermal growth factor, and granulocyte macrophage colony-stimulating factor) are well established. Recombinant factors that imitate the activity of these growth factors have been developed for topical application to diabetic ulcers. Becaplermin, a recombinant human platelet-derived growth factor, available as a 0.01% gel, has been approved in Spain for application to diabetic foot ulcers with a baseline surface less than 5cm2. Nevertheless, conflicting results in phase 4 clinical trials prevent us from recommending it as a first-line therapeutic option.58,59
RevascularizationThe theoretical benefits of revascularization of a diseased limb are clear. However, despite the many advances in the various techniques employed and their increased use, they have had only a limited impact on amputation rates.60 Revascularization options include angioplasty, thrombolysis, and bypass procedures.61
PreventionProlonged hyperglycemia is the main cause of neuropathy, which in turn represents the most important risk factor for the development of diabetic foot. The most important preventive measure is thus to maintain normal glucose levels.
The importance of regular inspection of both the feet and footwear of diabetic patients has been demonstrated by several studies.62,63 The aim of such examination is the early diagnosis of plantar ulcers and of the skin lesions that can favor their development.
Charcot ArthropathyWhile Carchot arthropathy was originally described in patients with tabes dorsalis due to syphilis, today diabetes mellitus is the main cause. Charcot arthropathy is a disorder of the joint in which destruction, fragmentation, and remodeling of bone and joints are present simultaneously.64,65 This condition is common, affecting up to a quarter of patients with diabetic foot.66
It would appear that peripheral neuropathy, whether somatic or autonomic, is a prerequisite for the development of Charcot arthropathy. In these circumstances the joints lack defense mechanisms against overload or trauma. To explain the pathogenesis of Charcot arthropathy a neurotraumatic theory and a neurovascular theory have been advanced. The neurotraumatic theory posits that repeated small insults to the midfoot joints lead to subchondral fractures. Moreover, because of insensitivity to pain, fractures may fail to be discovered and treated in time and midfoot joints may eventually become fragmented or dislocated.
The neurovascular theory, on the other hand, suggests that autonomic neuropathy leads to peripheral vasodilatation that stimulates bone resorption and predisposes bones to fractures.67 At any rate, it seems clear that faulty balance between bone formation and resorption is key to the development of Charcot arthropathy. In the initial stages increased bone resorption leads to the disruption of the plantar arch, while in advanced stages osteogenesis increases and there is fusion between the joints.68
Edema, erythema, and a rise in local temperature in a single foot appear to characterize the initial stages of Charcot arthropathy. In advanced stages, the destruction of the tarsal and tarsometatarsal joints leads to the loss of the plantar vault, anterior-posterior shortening of the foot, and the loss of medial concavity (Fig. 4). This deformity is also an important risk factor for the development of plantar ulcers (Fig. 5).
The basic problem is that Charcot arthropathy tends to be diagnosed in advanced stages, when bone destruction can no longer be corrected. Such signs as the absence of sweating and an increase in temperature in the diabetic foot require that Charcot arthropathy be ruled out.
In recent years, limb offloading and endovenous pamidronate have been shown to be effective in the treatment of acute Charcot arthropathy.69
ConclusionsDiabetic foot is clearly a major health problem because of its very high prevalence and the multiple complications it can generate. Dermatologists should not consider knowledge of this condition to lie outside their scope. We are routinely consulted about many foot conditions and should play an important role in guiding the initial diagnosis and treatment of skin diseases associated with diabetes mellitus and also diabetic foot lesions.
Conflicts of InterestThe author declares that he has no conflicts of interest.
I am grateful to Enric Giralt and Elena de Planell of the School of Podiatry of the University of Barcelona for kindly permitting the use of their clinical photographs and to my fellow dermatologists who read and improved the text.
Please cite this article as: Boada A. Lesiones cutáneas en el pie diabético. Actas Dermosifiliogr.2012;103:348-56.