Bimekizumab is the first and only dual selective inhibitor of IL-17 A and IL-17 F that has been proven effective and safe in Phase 3 clinical trials and has been approved by the European Medicines Agency (EMA) for the treatment of hidradenitis suppurativa (HS).
ObjectivesTo assess the safety and efficacy profile of bimekizumab in patients with moderate-to-severe HS across multiple centers in Spain.
MethodsWe conducted a retrospective cohort study including 84 patients treated with bimekizumab. Efficacy was assessed using an intention-to-treat approach, with patients who discontinued treatment for any reason or were lost to follow-up considered nonresponders. Data were collected at baseline, week 16, and week 24.
ResultsThe analysis included a total of 84 patients at 16 weeks, with 43 having completed the 24-week follow-up assessment (56 men [66.67%] and 28 women [33.33%]) with a mean age of 44.17 (13.43) years and a mean baseline IHS4 of 23.75 (12.87) were included. By week 24, IHS4 scores dropped by 16.73 points (p<0.0001); a HiSCR50 of 55.95% was achieved at week 16, which was maintained with a HiSCR50 of 55.81% at week 24; DLQI scores improved by 10.67 points (p<0.0001); pain scores dropped by 3.42 points (p<0.0001); and flare counts were reduced by 1.53 (p=0.0006). Adverse events were reported in 20.24% of patients by week 16, mainly candidiasis, and dropped to 11.90% by week 24. 53.57% (45/84) of patients achieved IHS4-55 by week 16, and by week 24, 60.47% (26/43) of patients maintained or reached this response level.
ConclusionsBimekizumab is effective for the treatment of HS in real-world clinical practice, with a manageable safety profile over the 24-week period. Our findings are consistent with those reported in phase 3 clinical trials.
Hidradenitis suppurativa (HS) is a chronic immune-mediated inflammatory disease with skin signs characterized by painful recurrent nodules, abscesses, and tunnels in intertriginous areas, such as the axilla, groin, and perianal region. Flares cause increased pain and suppuration and disease progression results in tissue destruction and scarring.1 HS significantly affects the patients’ quality of life, causing physical discomfort, social embarrassment, and psychological distress. Despite its high prevalence (estimated of 0.7–1.2% in the European-US population) and debilitating nature, effective treatment options for HS are limited.2
The pathophysiology of HS involves a dysregulated immune response, characterized by an excessive release of pro-inflammatory cytokines, including interleukin (IL)-17 A and IL-17 F. These cytokines play a crucial role in recruiting neutrophils and stimulating keratinocyte proliferation, ultimately leading to the formation of HS lesions.3
Bimekizumab is the first monoclonal IgG1 antibody that selectively targets IL-17 A and IL-17 F.4 Bimekizumab is currently approved for the treatment of moderate-to-severe plaque psoriasis, psoriatic arthritis, axial spondylarthritis, and HS.5 In phase 3 clinical trials in HS, BE HEARD I and BE HEARD II, bimekizumab achieved statistically significant and clinically meaningful improvements over placebo with substantial improvements in patient's quality of life and a favorable safety profile.6
While the safety and efficacy profile of bimekizumab has been established in clinical trials, real-world evidence is limited.7,8 The objective of this study is to evaluate the safety and efficacy profile of bimekizumab for the treatment of HS in our routine clinical practice.
Materials and methodsStudy design and patientsWe conducted a retrospective observational study including adult patients with moderate-to-severe HS treated with bimekizumab in Spanish hospitals from December 2022 through April 2024. Patients were followed as per current clinical practice.
Inclusion and exclusion criteriaThe inclusion criteria were (a) patients diagnosed with HS; (b) age≥18years; (c) moderate-to-severe HS, defined by a baseline International Hidradenitis Suppurativa Severity Score System (IHS4) score9 of ≥4; (d) any baseline count of abscesses, inflammatory nodules, and draining tunnels; (e) previous failure of at least 1 cycle of oral antibiotic treatment; (f) prior contraindication, failure or adverse event with adalimumab; (g) initiated bimekizumab treatment for HS.
Exclusion criteria were (a) age<18 years; (b) presence of medical conditions contraindicating the use of bimekizumab, such as hypersensitivity to bimekizumab, pregnancy, or lactation.
Variables of interestMain outcomesEfficacy was evaluated using an intention-to-treat approach, where patients discontinuing treatment for any reason or lost to follow-up were considered non-responders. HS activity was assessed by IHS4 and flare count (subjective referred by the patients). Pain intensity reported by patients was measured using the Visual Analog Scale (VAS), ranging from 0 (“no pain”) to 10 (“worst pain”). Patients’ quality of life was assessed using Dermatology Life Quality Index (DLQI) score.10 Data were collected at baseline, week 16 and week 24. Safety information was reported.
Other variables of interestDemographic and clinical data (age, sex, body mass index [BMI], comorbidities, toxic habits, previous treatments, HS phenotype11 and severity, and location of the lesions) were obtained from the patients’ health records.
EthicsThis study was conducted in full compliance with the principles outlined in the Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects and was approved by the institutional review board of the Research Foundation of Hospital Universitario y Politécnico La Fe (Valencia, Spain).
Statistical analysisDescriptive statistics were used to assess the characteristics of the sample. The Shapiro–Wilk test was utilized to evaluate the normality of the variables. Continuous variables are expressed as mean and standard deviation (SD), and the qualitative ones as relative and absolute frequency distributions. Nominal variables were compared using the Chi-square test or Fisher's exact test, as appropriate, whereas Student's t test or the Wilcoxon–Mann–Whitney test was used to draw comparisons between nominal and continuous data. Simple linear regression was used to explore potential associated factors for continuous variables, with the β coefficient and standard deviation (SD) used to predict the log odds of the dependent variable. Statistical significance was considered at p values<0.05 All statistical analyses were performed using JMP version 9.0.1 (SAS Institute, North Carolina, United States).
ResultsBaseline characteristics (Table 1)A total of 84 patients were included in the study (56 were men [66.67%] and 28 women [33.33%]), with a mean age of 44.17 (13.43) years and a mean body mass index (BMI) of 31.3 (9.3)kg/m2. A total of 60 patients (71.43%) were smokers and 4 (4.76%) were former smokers. A total of 25 patients (29.76%) had concomitant pilonidal sinus disease. Most patients (95.24%) had previous experience with biologics and the mean number of previous biologics was 1.80 (1.25). Most patients had Hurley stage II (28.57%) or III (69.05%). The mean number of previous surgical procedures was 1.85 (3.47). A total of 58 patients (69.05%) were Hurley stage III, 24 (28.57%) were Hurley stage II and 2 (2.38%) were Hurley stage I. The distribution of HS phenotype was 70.24% inflammatory and 29.76% follicular.
A total of 48 patients (57.14%) received the approved dose of bimekizumab for psoriasis (320mg/4 weeks until week 16 and every 8 weeks thereafter), 26 patients (30.95%) received 320mg/4 weeks, 7 patients (8.33%) received the approved dose for HS (320mg/2 weeks until week 16 and 320mg/4 weeks thereafter) and 3 patients (3.57%) received 320mg/2 weeks.
The mean baseline IHS4 score was 23.75 (12.87), pain VAS 7.32 (2.36) and DLQI 22.57 (7.81). During the previous 3 months, patients reported a mean of 2.91 (1.80) relapses. The location of the lesions was predominantly inguinal (86.91%), gluteal (73.81%) and less frequently perineal (53.57%), perianal (45.24%) and genital (40.48%) (Table 1).
Baseline characteristics of the patients included in the study (N=84).
| Variable | N=84 |
|---|---|
| Age, years. Mean±SD | 44.17±13.43 |
| Gender, n (%) | |
| Male | 56 (66.67) |
| Female | 28 (33.33) |
| BMI, kg/m2. Mean±SD | 28.87±5.40 |
| Smoking habit, n (%) | |
| Smoker | 60 (71,43) |
| Non-smoker | 20 (23.81) |
| Former smoker | 4 (4.76) |
| Comorbidities, n (%) | |
| Pilonidal sinus | 25 (29.76) |
| Diabetes mellitus | 17 (20.24) |
| Rheumatological disease | 7 (8.33) |
| Pyoderma gangrenosum | 2 (2.38) |
| Previous biologics, n (%) | |
| No | 4 (4.76) |
| Yes | 80 (95.24) |
| Number of previous biologics. Mean±SD | 1.80±1.25 |
| Number of previous surgical procedures. Mean±SD | 1.85 (3.47) |
| Clinical Hurley stage, n (%) | |
| Hurley 1 | 2 (2.38) |
| Hurley 2 | 24 (28.57) |
| Hurley 3 | 58 (69.05) |
| HS phenotype, n (%) | |
| Inflammatory | 59 (70.24) |
| Follicular | 25 (29.76) |
| Baseline IHS4. Mean±SD | 23.75±12.87 |
| DLQI basal. Mean±SD | 22.57±7.81 |
| Baseline pain VAS (0–10). Mean±SD | 7.32±2.36 |
| Baseline number of flares over the past 3 months. Mean±SD | 2.91±1.80 |
| Location of the lesions, n (%) | |
| Groin | 73 (86.91) |
| Buttock | 62 (73.81) |
| Perineum | 45 (53.57) |
| Perianal | 38 (45.24) |
| Genital (scrotum/vulva) | 34 (40.48) |
| Tights | 22 (26.19) |
| Intermammary region | 22 (26.19) |
| Back | 12 (14.29) |
| Face | 10 (11.91) |
| Scalp | 5 (5.95) |
BMI, body mass index; N, number; SD, standard deviation.
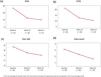
A total of 43 (51.2%) out of the 84 patients completed the 24-week follow-up assessment. By week 24, IHS4 scores dropped by 16.73 points (p<0.0001); DLQI scores improved by 10.67 points (p<0.0001); pain scores dropped by 3.42 points (p<0.0001); and flare counts dropped by 1.53 (p=0.0006) (Fig. 1). A total of 53.57% (45/84) of patients achieved IHS4-55 by week 16, and by week 24, 60.47% (26/43) of patients maintained or reached this response level. As for the HiSCR, a HiSCR50 of 55.95% was achieved at week 16, which was maintained with a HiSCR50 of 55.81% at week 24.
A total of 4 patients (4.76%) required a non-previously planned intervention upon week 24. Three cases required intralesional infiltration of corticosteroids and 1 case intramuscular administration of corticosteroids. At week 24, 11 patients (25.58%) received concomitant antibiotic therapy, and 2 patients (4.65%) underwent surgery.
Analysis of factors associated with efficacy (Table 2)Demographic and clinical characteristics, including sex, age at disease onset, smoking habits, body mass index (BMI), hidradenitis suppurativa (HS) phenotype, comorbidities, disease duration, prior surgical procedures, baseline IHS4, and baseline DLQI, did not show a statistically significant impact on achieving an IHS4-55 response at either week 16 or week 24. Although a significant negative correlation was observed between the baseline number of draining tunnels and IHS4-55 response by week 16 (p=0.046), this association was not maintained at week 24. Prior exposure to biological treatments was associated with a reduced likelihood of achieving IHS4-55 at week 16 (p=0.023), but not at week 24 (p=0.242). Similarly, a higher number of previous biologics was negatively correlated with response at week 16 (p=0.021), with no significant correlation by week 24. Significant differences in IHS4-55 response were observed across dosing regimens at both week 16 (p=0.0011) and week 24 (p=0.022), favoring induction protocols. Regarding lesion location, involvement of the groin was associated with a significantly higher response at week 16 (p=0.012), but not at week 24. Perianal (p=0.039), perineal (p=0.002), and genital (scrotum or vulva) (p=0.021) involvement were significantly associated with higher IHS4-55 response rates at week 24, with genital involvement also showing a significant association at week 16 (p=0.021). Concomitant interventions, including antibiotic therapy, intralesional corticosteroids, or surgical procedures, did not significantly impact IHS4-55 response at either time point.
Determinants of IHS4-55 response at weeks 16 and 24.
| Factor | Week 16 | Week 24 |
|---|---|---|
| Patient characteristics | ||
| Sex | Male 46.43% vs Female 67.86%(p=0.063) | Male 55.17% vs Female 71.43%(p=0.307) |
| Age of disease onset | β=−0.006 (SD, 0.022)(p=0.804) | β=0.053 (SD, 0.037)(p=0.152) |
| Diagnostic delay | β=0.013 (SD, 0.037)(p=0.728) | β=0.086 (SD, 0.078)(p=0.270) |
| Smoking habits | No smoker 55% vs Former smoker 25% vs Active smoker 55%(p=0.502) | No smoker 45.45% vs Former smoker 100% vs Active smoker 63.33%(p=0.294) |
| BMI | β=0.0043 (SD, 0.04)(p=0.917) | β=−0.033 (SD, 0.057)(p=0.556) |
| Comorbidities | ||
| IBD | Yes 0% vs No 53.57%(p=0.842) | Yes 60.47% vs No 39.53%(p=0.842) |
| Rheumatic disease | Yes 57.14% vs No 53.25%(p=0.843) | Yes 83.33% vs No 56.76%(p=0.212) |
| Pyoderma gangrenosum | Yes 50% vs No 53.66%(p=0.918) | Yes 50% vs No 60.96%(p=0.757) |
| Diabetes | Yes 50% vs No 53.95%(p=0.832) | Yes 66.67% vs No 60%(p=0.820) |
| Disease background | ||
| Disease duration | β=−0.004 (SD, 0.019)(p=0.823) | β=0.017 (SD, 0.026)(p=0.516) |
| HS phenotype | Follicular subtype 50% vs Inflammatory subtype 61.02% vs Mixed subtype 34.78%(p=0.109) | Follicular subtype 50% vs Inflammatory subtype 60% vs Mixed subtype 66.67%(p=0.909) |
| Prior surgical procedures | Yes 50% vs No 62.16%(p=0.572) | Yes 66.67% vs No 59.46%(p=0.738) |
| Number of prior surgical procedures | β=0.064 (SD, 0.069)(p=0.352) | β=−0.002 (SD, 0.093)(p=0.984) |
| Prior biological treatment | Yes 51.25% vs No 100%(p=0.023) | Yes 58.54% vs No 100%(p=0.242) |
| Number of previous biologics | β=−0.482 (SD, 0.209)(p=0.021) | β=−0.177 (SD, 0.240)(p=0.460) |
| Prior secukinumab | Yes 40.63% vs No 61.54%(p=0.062) | Yes 61.54% vs No 60%(p=0.925) |
| Baseline characteristics of the disease | ||
| Baseline IHS4 | β=−0.005 (SD, 0.016)(p=0.758) | β=0.0025 (SD, 0.023)(p=0.285) |
| Baseline DLQI | β=−0.043 (SD, 0.034)(p=0.199) | β=0.081 (SD, 0.052)(p=0.118) |
| Baseline inflammatory nodules | β=0.123 (SD, 0.081)(p=0.123) | β=0.176 (SD, 0.101)(p=0.082) |
| Baseline abscesses | β=−0.218 (SD, 0.165)(p=0.187) | β=−0.009 (SD, 0.194)(p=0.963) |
| Baseline non-draining tunnels | β=−0.381 (SD, 0.241)(p=0.114) | β=0.136 (SD, 0.229)(p=0.552) |
| Baseline draining tunnels | β=−0.249 (SD, 0.125)(p=0.046) | β=−0.030 (SD, 0.124)(p=0.809) |
| Baseline flare count | β=−0.201 (SD, 0.165)(p=0.229) | β=−0.155 (SD, 0.188)(p=0.411) |
| Lesion location: axillae | Yes 58.62% vs No 64.29%(p=0.722) | Yes 58.62% vs No 64.29%(p=0.722) |
| Lesion location: thighs | Yes 59.09% vs No 51.61%(p=0.546) | Yes 73.68% vs No 50%(p=0.115) |
| Lesion location: groin | Yes 58.90% vs No 18.18%(p=0.012) | Yes 62.16% vs No 50%(p=0.576) |
| Lesion location: buttock | Yes 53.23% vs No 54.44%(p=0.915) | Yes 70% vs No 38.46%(p=0.052) |
| Lesion location: perianal area | Yes 52.63% vs No 54.35%(p=0.875) | Yes 76.19% vs No 45.45%(p=0.039) |
| Lesion location: perineum | Yes 53.57% vs No 56.41%(p=0.627) | Yes 80% vs No 33.33%(p=0.002) |
| Lesion location: genital area (scrotum/vulva) | Yes 73.53% vs No 40%(p=0.021) | Yes 77.27% vs No 42.86%(p=0.021) |
| Lesion location: scalp | Yes 60% vs No 53.16%(p=0.767) | Yes 100% vs No 57.5%(p=0.147) |
| Lesion location: lateral trunk | Yes 27.27% vs No 57.53%(p=0.06) | Yes 40% vs No 63.16%(p=0.319) |
| Lesion location: intermammary area | Yes 50% vs No 54.84%(p=0.696) | Yes 69.23% vs No 56.67%(p=0.439) |
| Lesion location: face | Yes 50% vs No 54.05%(p=0.809) | Yes 80% vs No 57.89%(p=0.342) |
| Lesion location: back | Yes 50% vs No 54.17%(p=0.789) | Yes 50% vs No 62.16%(p=0.580) |
| Dosage and concomitant treatments | ||
| Dosing regime | 320mg day 0 and 7 followed by 320mg every 2 weeks 33.33% vs 320mg day 0 and 7 followed by 320mg every 4 weeks 57.14% vs 320mg day 0, 7, 14 and 21 followed by 320mg every 8 weeks 70,83% vs 320mg day 0 followed by 320mg every 4 weeks 23.08%(p=0.0011) | 320mg day 0 and 7 followed by 320mg every 2 weeks 0% vs 320mg day 0 and 7 followed by 320mg every 4 weeks 75% vs 320mg day 0, 7, 14 and 21 followed by 320mg every 8 weeks 70.97% vs 320mg day 0 followed by 320mg every 4 weeks 16.67%(p=0.022) |
| Concomitant antibiotic treatment | Yes 66.67% vs No 46.30%(p=0.072) | Yes 58.82% vs No 61.54%(p=0.858) |
| Concomitant intralesional corticosteroid | Yes 60% vs No 52.70%(p=0.664) | Yes 50% vs No 48.31%(p=0.794) |
| Concomitant surgical procedures | Yes 37.50% vs No 55.26%(p=0.338) | Yes 50% vs No 62.16%(p=0.572) |
BMI, body mass index; DLQI, dermatology life quality index; IBD, inflammatory bowel disease; IHS4, International Hidradenitis Suppurativa Severity Score System; SD, standard deviation. Data are presented as proportions (A% vs B%) or as β values (mean±standard deviation). p-Values<0.05 are highlighted in bold.
Bimekizumab was well tolerated, there were no discontinuations for safety reasons, and no new safety alerts were identified. Adverse events were reported in 20.24% of patients by week 16, mainly oral candidiasis, and dropped down to 11.90% by week 24.
DiscussionBimekizumab is the first and only dual selective inhibitor of both isoforms A and F of IL-17 approved for the treatment of HS.5 Bimekizumab has shown rapid and substantial clinical improvements in HS clinical trials, including reduction of inflammatory nodules, abscess and draining tunnels, disease severity, pain scores, and impact on patients’ quality of life as early as at week 16 and maintained 1 year into therapy.6 Our real-world patient series confirms these findings, demonstrating that bimekizumab could emerge as an effective treatment option for HS.
Our study included a patient population with significantly severe disease features, notably higher than those in BE HEARD clinical trials. Our cohort presented a higher proportion of patients at the Hurley III stage (69% vs 44% in BE HEARD trials), and most patients presented previous exposure to biologic drugs (95% vs 19% in BE HEARD trials).6 Despite these challenges, motivated in large part by the fact that most patients started treatment on a compassionate off-label basis, the observed efficacy of bimekizumab in our sample is remarkable. Our cohort of patients experienced rapid and sustained symptom remission with statistically significant differences between baseline and week 16/24 in all activity scores and patient-reported outcomes, resulting in a significant improvement in their overall quality of life. Both in clinical trials and in real-world, bimekizumab treatment offers the potential for deep HS remission and reduced disease recurrence, even in those patients with more severe forms.
Despite the small sample size limiting subgroup analyses, we aimed to identify potential predictors of response. Most demographic and clinical characteristics did not have an impact on IH4-55 response rates at week 16/24 (sex, age, smoking habits, BMI, HS phenotype, comorbidities, disease duration, prior surgical procedures, baseline IHS4 and DLQI), reinforcing bimekizumab robustness observed in clinical trials.6 Still, we identified a positive correlation between the baseline count of draining tunnels and flares and IHS4-55. Although IL-17F is a weaker inducer of proinflammatory cytokine than IL-17A, it is more abundant in HS lesions.12–14 In addition, cells that expressed either IL-17A or IL-17F are observed in early HS lesions whereas IL-17F-producing cells can localize to IL-1-expressing cells in chronic lesions,14 which suggests that inhibition of IL-17F could have a key role in managing persistent lesions, such as draining tunnels.
Prior biological treatment was linked to lower probability of achieving IHS4-55 at week 16 but not at week 24, suggesting that previous exposure to biologics may translate into a slower onset of action. Significant differences in IHS4-55 response were observed between different dosing regimens at both time points, highlighting the importance of induction dosing for maximizing bimekizumab outcomes. Lesion location played a role in response rates, with groin lesions linked to higher IHS4-55 rates at week 16 and genital lesions showing higher rates at both week 16 and 24. This is particularly important due to the high prevalence of lesions in these areas and its high impact in patient's quality of life. Notably, neither concomitant interventions nor antibiotic therapy affected IHS4-55 response rates, indicating that the efficacy of bimekizumab is robust across varying treatment contexts. Of note, in this study we used the IHS4 scale for the subanalysis of the data, rather than the HiSCR based on the fact that IHS4 may be a more global scale that can capture improvement in the three elementary types of HS lesions (abscesses, inflammatory nodules and draining tunnels). In contrast, the HiSCR only assesses changes in abscesses and inflammatory nodules, while bimekizumab has shown potential to reduce the number of draining tunnels.
Throughout its clinical development, bimekizumab has consistently shown a favorable safety profile with no new safety signals emerging.6 In our study, bimekizumab was well tolerated, and no remarkable adverse events were observed. The most common adverse event was oral candidiasis, which were successfully managed with antifungal standard therapy without requiring discontinuation of treatment.
Inhibition of IL-17F in addition to IL-17A may offer significant advantages leading to consistently better clinical outcomes, as has been shown in other immune-mediated inflammatory diseases. This was demonstrated in the head-to-head BE RADIANT clinical trial in psoriasis, which showed superiority of bimekizumab over secukinumab in all measured endpoints.15 Our observations in the HS setting may support this notion, although the potential superiority of bimekizumab using dual targeting of IL-17A and IL-17F remains to be validated.
This study has limitations, including its retrospective design, lack of a control group, limited follow-up duration, and small sample size from a single geographic region. A longer follow-up period could provide more comprehensive insights.
In conclusion, our real-world patient series adds to the limited evidence of bimekizumab's usefulness in HS, highlighting its potential efficacy, significant clinical improvements, and enhanced quality of life. By targeting IL-17A and IL-17F, bimekizumab shows promising thorough and lasting disease remission, supporting its potential to improve HS management.
Conflict of interestThe authors declare that they have no conflict of interest.