High-grade anal intraepithelial squamous lesion is significantly prevalent among men who have sex with men and are infected with the human immunodeficiency virus (HIV). This condition—the precursor to anal cancer—significantly increases the risk of developing it. Conversely, low-grade anal intraepithelial squamous typically follow a benign course and usually regress spontaneously.
Materials and methodsTo describe a population of men who have sex with men living with HIV followed in a specialized anal cancer screening unit we conducted an observational, retrospective, and single-center study.
ResultsNinety-four patients were analyzed, with a mean age of 39±9 years, and a 87% positivity rate for high-risk human papillomavirus (HR-HPV). At the initial visit, 47% presented with low-grade squamous intraepithelial lesions. The progression rate to high-grade squamous intraepithelial lesion was 37.2 per 100,000 patients/year. None of the patients developed anal cancer. Tobacco and alcohol consumption were associated with this progression.
DiscussionIn this series, longer duration of HIV infection, tobacco and alcohol use and the presence of HR-HPV were significantly associated with the occurrence of high-grade intraepithelial lesions. A lower risk of progression was seen in patients with higher education.
ConclusionIn men who have sex with men living with HIV, the association of factors such as smoking, alcohol, the presence of HR-HPV and an increased burden of human papillomavirus disease makes these patients more susceptible to develop high-grade anal squamous lesions.
La lesión escamosa intraepitelial anal de alto grado es especialmente común en hombres que mantienen relaciones sexuales con otros hombres y viven con el virus de inmunodeficiencia humana (VIH). Esta condición, al ser la precursora del cáncer anal, aumenta significativamente el riesgo de padecerlo. Por otro lado, la lesión escamosa intraepitelial anal de bajo grado suele tener una evolución benigna e incluso a regresar espontáneamente.
Materiales y métodosCon el objetivo de describir una población de hombres que tienen sexo con hombres, que viven con el VIH, seguidos en una consulta de cribado de cáncer anal, se diseñó un estudio observacional, retrospectivo y unicéntrico.
ResultadosSe incluyeron 94 pacientes, con edad media de 39±9 años y 87% de positividad para virus del papiloma humano de alto riesgo (VPH-AR). El 47% presentaban lesión escamosa intraepitelial anal de bajo grado confirmada mediante biopsia en la primera visita. La tasa de progresión a lesión escamosa intraepitelial de alto grado fue de 37,2 por 100.000 pacientes/año. Ninguno desarrolló cáncer anal. El consumo de tabaco y alcohol se relacionó con la progresión.
DiscusiónEn esta serie, la mayor duración de la infección por VIH, el consumo de tabaco y alcohol, así como la presencia de VPH-AR se asociaron significativamente con la aparición de lesión intraepitelial de alto grado. Se observó menor riesgo de progresión en pacientes con nivel educativo superior.
ConclusiónLa asociación de factores como el tabaco, el alcohol, la presencia de VPH-AR y una mayor carga de enfermedad causada por el virus del papiloma humano aumenta la susceptibilidad de los hombres que tienen sexo con hombres y que viven con el VIH a desarrollar lesiones escamosas anales de alto grado.
Anal squamous intraepithelial lesion (SIL), is the cytological and architectural alteration of the squamous transitional epithelium of the anus, characterized by a proliferation of cells with large and irregular nuclei.1 It is categorized according to the thickness of the damaged epithelium:1,2
- •
Low-grade squamous intraepithelial lesion (LSIL), when it affects the lower third (< 33% of the thickness of the epithelium). This concept includes lesions categorized as mild dysplasia, grade I anal intraepithelial neoplasm, and condyloma acuminatum.
- •
High-grade squamous intraepithelial lesion (HSIL) is the term used for alterations > 33% of the epithelium thickness and including moderate dysplasia, severe dysplasia, carcinoma in situ, Bowen's disease, bowenoid papulosis, and grades II and III intraepithelial neoplasms.
All these lesions are caused by the human papillomavirus (HPV), with high-risk genotypes being more frequent in HSIL lesions, primarily HPV 16.3,4
In the 1980s, SIL was proposed as the precursor lesion to anal cancer,5 and since then, prospective and retrospective studies have suggested that screening and treatment of HSIL in at-risk populations could reduce anal cancer-related mortality.6,7 Finally, in 2022, the results of the ANCHOR (Anal Cancer/HSIL Outcomes Research) study8 were published. This randomized clinical trial evaluated the impact of monitoring and treating HSIL to prevent anal cancer in people living with HIV (PLWH). The objective of recruiting 5058 patients was not essential to demonstrate a 57% reduction in the risk of developing anal cancer in the treatment vs the monitoring arm.8,9
HPV-related cervical cancer screening programs have created a significant impact on the incidence and mortality associated with this disease.6 The ANCHOR study has provided solid evidence supporting the recommendation for screening SIL in PLWH, which is similar to cervical cancer in women.8 Men who have sex with men (MSM) have a cancer risk rate which is 100 times higher than that of the general population (100/100,000 patients/year in MSM vs 1/100,000 patients/year in the general population).10 Therefore, MSM living with HIV are the ones who benefit the most from HSIL screening.10,11
Although LSIL lesions are usually not precursors to anal cancer they do represent a risk factor for the development of HSIL. Therefore, indirectly, the presence of LSIL could contribute to an increased risk of developing anal cancer.12,13
Although condylomas are generally classified as LSIL, certain authors have decided to separate them from this group of lesions to assess the patient's risk of developing HSIL and anal cancer. Thus, in a retrospective study of MSM living with HIV, Fazendin et al.14 found that more than 80% of patients with anal condylomas and one-third of those with LSIL developed HSIL during follow-up.
Materials and methodsWe conducted an observational, retrospective, unicentric study to evaluate a cohort of MSM living with HIV, who were followed using high-resolution anoscopy (HRA) in a screening unit. In this sample, our aim was to identify factors associated with the progression to HSIL based on whether patients presented with LSIL at their first consultation in the unit.
This study was approved by Hospital Universitario La Paz ethics committee.
Patients were recruited from the specialized early screening consultation for HSIL/anal cancer at Hospital Universitario La Paz, Madrid, Spain. They had been referred from internal medicine services and infectious disease units following the pre-established and agreed criteria detailed below: HIV positive patients with anal cytology showing cytological alterations, symptoms suggestive of HPV disease (anal condylomas, perianal skin lesions, or suggestive rectal examination), or incidental detection of SIL.
From the early years of the specialized consultation, a registry of patients was established in an anonymized database, after informed consent was signed, located exclusively on the hospital servers. For this study, only records of MSM living with HIV who had consulted from January 1st, 2008 through December 30th, 2018, with normal HRA or presence of LSIL, and with 2 or more HRAs during follow-up, separated by at least 3 months, were included. Patients with a previous diagnosis of HSIL or anal carcinoma were excluded.
For the analysis, patients were categorized into 2 groups based on their progression to HSIL during follow-up visits, which were determined by the physician monitoring the patient, so the frequency was variable (3, 6, 12 months) and not determined by the observer. Examinations in the specialized consultation could include—in addition to direct observation by HRA—prior anal cytology and biopsy to confirm the diagnosis of LSIL or HSIL. Along with the anal cytology, HPV genotyping studies were conducted including 35 genotypes: high risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68A-68B), probable high risk (26, 53, 73, 82), and low risk (6, 11, 40, 42, 43, 44, 54, 61, 62, 71, 70, 72, 81, 83, 84, 85, 89). Demographic data, toxic habits, sexual habits, previous sexually transmitted infections (STIs), clinical, evolutionary, and therapeutic data were collected. Deadline for data mining was November 30th, 2020.
The analysis was conducted using SAS Enterprise 9.3 and R version 4.2.1. Frequencies and percentages were used for categorical variables, while continuous variables were expressed as mean, standard deviation, median, and range. To contrast differences between independent groups for categorical variables, the chi-square test was used. For continuous variables, the Mann-Whitney U test for independent samples or the Student's t-test was used, when appropriate.
To respond to the main objective, the variable time until the HSIL event was considered; cases in which no event occurred were considered censored, and their time was calculated up to the last available date. Inter-group comparison was evaluated using Cox regression. The per-group median and 95% confidence interval (CI 95%) for survival are presented, as well as the hazard ratio (HR) and CI 95%.
All hypothesis tests were conducted with a significance level of 5% (two-tailed). The p-value is presented for all comparisons made.
ResultsA total of 94 MSM who met the previously mentioned criteria were finally selected from a cohort of 520 patients examined via anal cytology and/or HRA in the specialized consultation (fig. 1).
Distribution of patients according to assessment with high-resolution anoscopy. A) Baseline. B) Distribution of patients during follow-up. *HRA: high-resolution anoscopies, MSM: men who have sex with men, HSIL: high-grade squamous intraepithelial lesion, HULP: Hospital Universitario La Paz.
The mean age at the start of follow-up was 39±9 years, and the mean age at HIV diagnosis was 31±7 years. A total of 97% of the patients (n=91) were on highly active antiretroviral therapy (HAART). Only 1 patient met the criteria for acquired immunodeficiency syndrome, while the others maintained adequate viro-immunological control (mean CD4 count of 681±275/mm3, median viral load of 0 copies/mL, interquartile range of 0 to 20 copies/mL).
Regarding socio-cultural level and habits, 55% had higher education. A total of 46% of the patients were smokers, 62% consumed alcohol, and more than half of these (57%, n=54) identified themselves as social drinkers, and the rest as excessive consumers (above the recommended daily dose, abuse, or dependence). The consumption of psychoactive substances in contexts unrelated to sexual activity was reported in 18 patients (19%). A total of 88% of the patients (n=83) practiced anal sex as their preferred sexual practice, and 3 patients reported being bisexual.
A total of 86% of the patients had suffered from some STI. Before starting follow-up, 46% of cases had presented with anal or genital condylomas. The baseline characteristics of the patients are summarized in Table 1.
Characteristics of the patients included in the study (n=94).
| Patients who progressed to HSIL (n=35) | Patients who did not progress to HSIL (n=59) | Total (n=94) | p | |
|---|---|---|---|---|
| Age | 39.72±SD 9.8(min 26-max 58) | 38.88±SD 9.6(min 21-max 65) | 39.20±SD 9.6(min 21-max 65) | 0.69 |
| Level of education | ||||
| Primary | 3 (9.1%) | 6 (10.5%) | 9 (10%) | 0.92 |
| Secondary | 10 (30.3%) | 19 (33.3%) | 29 (32%) | |
| Higher | 20 (60.6%) | 32 (56.1%) | 52 (58%) | |
| Tobacco | 22 (62.9%) | 21 (35.6%) | 43 (46%) | 0.02* |
| Alcohol | 26 (78.8%) | 34 (59.6%) | 60 (64%) | 0.10 |
| Drugs | 10 (16.9%) | 10 (28.5%) | 20 (21%) | 0.28 |
| Stable partner | ||||
| Yes | 15 (42.9%) | 30 (50.8%) | 45 (48%) | 0.59 |
| No | 20 (57.1%) | 29 (49.2%) | 49 (52%) | |
| Sexual relations under the influence of drugs or alcohol | ||||
| Yes | 8 (22.9%) | 15 (25.4%) | 23 (24%) | 0.97 |
| No | 27 (77.1%) | 44 (74.6%) | 71 (76%) | |
| History of STIs | ||||
| Yes | 31 (88.6%) | 50 (84.7%) | 81 (86%) | 0.83 |
| No | 4 (11.4%) | 9 (15.3%) | 13 (14%) | |
| History of condylomas | ||||
| Anal | 13 (37.1%) | 22 (37.3%) | 35 (37%) | 1 |
| Genital | 2 (5.7%) | 7 (11.9%) | 9 (10%) | 0.54 |
| Previous syphilis | 15 (42.9%) | 27 (45.8%) | 42 (45%) | 0.95 |
| Previous proctitis | 8 (22.9%) | 14 (23.7%) | 22 (23%) | 1 |
| No. HPV | 5.1±SD 2.78 | 4.08±SD 2.86 | 4.5±SD 2.9 | 0.07 |
| High-risk HPV | 32 (91.4%) | 50 (84.7%) | 82 (87%) | 0.54 |
| HPV16 | 14 (40%) | 13 (22%) | 27 (29%) | 0.10 |
| HPV31 | 14 (40%) | 8 (13.6%) | 22 (23%) | < 0.01* |
| No. of sexual partners/lifetime | ||||
| 1-5 | 3 (8.5%) | 3 (5.1%) | 6 (6%) | 0.86 |
| 6-10 | 2 (5.7%) | 4 (6.9%) | 6 (6%) | |
| 11-25 | 4 (11.4%) | 7 (11.9%) | 11 (12%) | |
| 26-50 | 3 (8.6%) | 8 (13.6%) | 11 (12%) | |
| 51-100 | 6 (17.1%) | 16 (27.1%) | 22 (23%) | |
| > 100 | 10 (28.6%) | 14 (23.7%) | 24 (26%) | |
| Type of anal sex | ||||
| Insertive | 5 (14.2%) | 12 (20.3%) | 17 (18%) | 0.81 |
| Receptive | 7 (20%) | 14 (23.7%) | 21 (22%) | |
| Indifferent | 17 (48.5%) | 28 (47.5%) | 45 (48%) | |
| Use of condom | ||||
| Yes | 10 (28.5%) | 25 (42.4%) | 35 (37%) | 0.46 |
| No | 11 (31.4%) | 14 (23.7%) | 25 (27%) | |
| Sometimes | 9 (25.7%) | 15 (25.4%) | 24 (26%) | |
| Cytology | 0.62 | |||
| No cytology | 12 (34.3%) | 28 (47.5%) | 40 (43%) | |
| ASCUS | 4 (11.4%) | 7 (11.9%) | 11 (12%) | |
| High-grade dysplasia | 5 (14.3%) | 6 (10.2%) | 11 (12%) | |
| Low-grade dysplasia | 14 (40%) | 17 (28.8%) | 31 (33%) | |
| Not representative | 0 | 1 (1.7%) | 1 (1%) | |
| Baseline anoscopy | 0.34 | |||
| Normal | 19 (54.3%) | 33 (55.9%) | 52 (55%) | |
| Condyloma | 4 (11.4%) | 12 (20.3%) | 16 (17%) | |
| LSIL | 12 (34.3%) | 14 (23.7%) | 26 (28%) | |
| Treatment | ||||
| Yes | 31 (88.6%) | 25 (42.4%) | 56 (60%) | < 0.01* |
| No | 4 (11.4%) | 34 (57.6%) | 38 (40%) | |
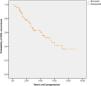
The mean duration of follow-up was 3.9±2.5 years (median of 3.2 years, minimum of 0.3 years, and maximum of 8.9 years). Regarding disease progression, 37% (n=35) of the patients developed HSIL, with a mean time of 2.4±1.73 years (median of 2.29 years). Patient distribution according to their baseline and final assessment by HRA is shown in Figure 2. Half of the patients who experienced progression did so within the first 5 years. Those who had previously experienced condylomas had shorter median times to progression to HSIL vs those who had not (4.25 vs 5.6 years), although this difference did not reach statistical significance (p=0.987).
Patients who tested positive for HPV16 (40%, n=14) exhibited a median progression of 4.25 years, while those who tested negative for this genotype had a median progression of 5.98 years, yet this was a statistically non-significant association (p=0.381). The detection of another high-risk genotype—specifically HPV31—demonstrated a significant correlation with a more accelerated progression towards HSIL in the affected patients (p=0.002), with a median survival of 2.56 years for positive patients vs 7.11 years for negative patients, and a HR (95%CI) of 2.957 (1.473-5.936).
In the univariate analysis, patients with higher education had a lower risk of progressing to HSIL. However, smokers, those with a higher viral load, and those with a longer duration of HIV infection had a higher risk.
Tobacco consumption (p=0.007), alcohol consumption (p=0.01) (fig. 3), and having received treatment during follow-up (p <0.001) were associated with progression. A total of 50% of smokers progressed within 3 years; however, only 33% of non-smokers progressed in the same timeframe (survival table: annex I).
Age, adherence to follow-up visits, total HPV, having had previous STIs, condom use during sexual relations, the number of sexual partners, and the type of anal sex practiced did not have any impact on disease progression (Table 1).
DiscussionIn the analysis of risk markers for progression to HSIL in MSM living with HIV, the relevance of tobacco and alcohol consumption stands out, as these variables are significantly associated with a higher probability of progression.15 This underscores the need for specific interventions to mitigate these risk factors within the population of MSM living with HIV.
In this study patients had a high incidence of high-risk HPV (HR-HPV) (87%); however, only the presence of HPV31 was significantly associated with disease progression. Infection due to HR-HPV facilitates the onset of HSIL and anal cancer. Although the genotype commonly involved in the development of HSIL and anal cancer is primarily HPV16,16 this relationship could not be demonstrated in the studied population, likely due to the limited sample size. The detection of HR-HPV represents a relevant indicator of the rate of progression towards HSIL17,18; the fact that HPV31 is a HR-HPV reinforces the importance of close monitoring in individuals with these genotypes, allowing for earlier and more effective intervention.
The study addresses the relationship between the presence of LSIL and the detection of HSIL, evidencing that although they are not direct precursors, LSIL acts as a risk marker.18,19 This underscores the necessity of considering the complete medical history when assessing the risk of progression in MSM living with HIV, particularly those who have or have had LSIL.
Univariate analysis reveals that patients with higher education exhibited a lower risk of progression to HSIL, highlighting the importance of education in disease control and prevention. We believe that a higher level of education favors the understanding of the disease, adherence to check-ups, necessary habit changes to reduce the risk of progression, and the correct and complete use of prescribed treatments. Similarly, it was confirmed that smoking patients, those with higher viral loads, and those with longer durations of HIV infection had a greater risk of progressing to HSIL, suggesting that these subpopulations require special attention when considering follow-up.20–22
Finally, it has been reported that patients who received treatment showed a greater likelihood of progressing to HSIL. We consider that treatment is not a progression factor, but an indirect measure of disease burden. This statement is supported by the fact that patients with a higher number of lesions tend to be more symptomatic, which would favor the indication for treatment to alleviate the discomfort caused by these lesions. Additionally, the presence of multiple condylomas may mask underlying synchronous HSIL lesions. Finally, this study was not designed to evaluate a single treatment; rather, it observes the routine clinical practice of a specialized consultation.
The inherent limitations of this study deserve special consideration. As it is a single-center study, the small sample size complicates conducting a detailed subgroup analysis to determine the baseline status that could promote progression to HSIL. In contrast, data come from a center with experience in the field, which favors homogeneity in data mining, systematic management, and protocol adherence when it comes to categorizing and treating patients.
The retrospective nature of the study is inevitable linked to a risk of information bias. The exclusive inclusion of patients from the multidisciplinary unit limits the generalization of findings to patients outside this unit, thereby introducing selection bias. However, data were meticulously collected by dermatologists specialized in the field, and the few missing data points were prospectively collected by reviewing the medical histories of patients still in follow-up. Of note that tolerance to the HRA may not be good, so it is common to have losses to follow-up, which may ultimately have reduced the number of included patients and their follow-up time.
In conclusion, this study contributes to understanding the risk factors and progression of HSIL in MSM living with HIV. Results support the implementation of strategies for prevention, early detection, and treatment in this high-risk population, which is consistent with the latest scientific evidence and offers new perspectives on the clinical management of anal lesions such as SIL.
The presence of HSIL in the squamous transitional epithelium of the anus has significant implications for the health of vulnerable populations such as PLWH, and especially MSM. In the context of this observational, retrospective study, the previously described association between SIL and HPV is noted, highlighting the predominant presence of high-risk genotypes.17,23,24 This finding supports the importance of monitoring and early detecting precursor lesions, especially in higher-risk populations, such as PLWH.
ConclusionsThe presence of condylomas or LSIL is a well-known risk marker for the development of anal cancer. Since these lesions have a low potential for malignancy, the approach to these patients is usually conservative. However, this study supports previous evidence that MSM living with HIV with associated risk factors (tobacco, alcohol, HR-HPV) and a higher disease burden from HPV (LSIL/condyloma) have an increased risk of developing HSIL. These patients should, at least, be closely monitored, considering active management of lesions or performing new biopsies in the presence of lesions suggestive of HSIL. This management will be individualized and adjusted based on symptoms and treatment response, should it ultimately be initiated.
Conflicts of interestNone declared.