Dedicated dermoscopy units assess individuals at high risk for melanoma. Understanding the reasons for referral to these units and the epidemiological profile of referred patients can help optimize health care resources and determine who benefits most from dermoscopic evaluation. We analyzed reasons for referral and epidemiological characteristics of 413 patients with at least 1 high-risk factor for melanoma seen at a dedicated dermoscopy unit over a period of 10 years. We also analyzed the number of necessary excisions (NNE) for each melanoma diagnosed, histologic features, and associations between nonenvironmental factors and diagnosis. The main reasons for referral were a past history of melanoma (21.5%), changes detected by the patient or a relative (20%), clinical and/or dermoscopic findings suggestive of malignancy (19.4%), and a family history of melanoma (17.4%). Seventy-six of the 178 excised lesions were melanomas (NNE per melanoma detected, 2.34). Older age was the only risk factor significantly associated with the development of melanoma.
Las consultas monográficas de dermatoscopia digital están dirigidas a población con alto riesgo de melanoma. Conocer los motivos de derivación a estas consultas, así como las características epidemiológicas de los pacientes permite optimizar los recursos sanitarios y determinar qué pacientes se benefician más de esta técnica. Se analizaron los motivos de derivación y las características epidemiológicas de 413 pacientes atendidos en una consulta monográfica de dermatoscopia en un período de 10 años que presentaban al menos un criterio de alto riesgo de melanoma. También se analizó el número necesario de extirpaciones (NNE) por cada melanoma diagnosticado, sus características histológicas y qué variables no ambientales se asociaron con su diagnóstico. Los motivos de derivación más frecuentes fueron: antecedentes de melanoma previo (21,5%), cambios detectados por el paciente o su familia (20%), hallazgos clínicos y dermatoscópicos sospechosos de malignidad (19,4%) y antecedentes familiares de melanoma (17,4%); 76 de las 178 lesiones extirpadas fueron melanomas, obteniendo un NNE de 2,34. La edad avanzada fue el único factor de riesgo que se asoció de forma estadísticamente significativa con el desarrollo de melanoma.
The incidence of cutaneous melanoma in recent decades has increased at a faster rate than that of any other cancer, and not just because of an increase in early diagnoses.1,2 Although advances have been made in the treatment of disseminated melanoma, early diagnosis using techniques such as dermoscopy continues to have a major impact on prognosis.
Dermoscopy units are dedicated units that target individuals at high risk for melanoma. They analyze changes to lesions and can detect melanoma at very early stages. Understanding the reasons for referral to these units and the epidemiologic profile of patients seen is key for optimizing health care resources and identifying groups of individuals who might benefit most from dermoscopic evaluation.
Patients and MethodsWe performed a descriptive, retrospective study of patients seen at a dedicated dermoscopy unit in a tertiary care hospital between January 1, 2009 and December 31, 2019. To be included, patients had to meet at least 1 of the following criteria: a personal history of melanoma, a family history of melanoma, and the presence of more than 100 melanocytic nevi or at least 3 melanocytic nevi with clinical and/or dermoscopic atypia. They also had to have a minimum follow-up time of 5 years.
All patients provided verbal consent for their data to be used anonymously and confidentially.
Patients who did not meet the inclusion criteria (i.e., those who had no personal or family history of melanoma, had fewer than 100 nevi, and had been followed for less than 5 years) were excluded, as were patients referred for once-off evaluations or examination of other lesions, such as pigmented lesions in given locations (nails, mucosal membranes).
The variables analyzed for each patient were reason for referral, follow-up time (months), age at start of follow-up, sex, personal and family history of melanoma and dysplastic melanocytic nevus, Fitzpatrick skin type (I–IV), and approximate number of melanocytic nevi with a diameter larger than 3mm (<25, 25–50, 50–100, >100). We also analyzed the number of necessary excisions (NNEs) for each melanoma diagnosed during follow-up, histologic features of these melanomas, and associations between nonenvironmental factors and the development of melanoma.
The Pearson χ2 test was used for univariate analysis of qualitative variables. Statistical significance was set at a P value of less than .05.
ResultsOf the 1860 patients seen at the dermoscopy unit during the study period, 413 were included.
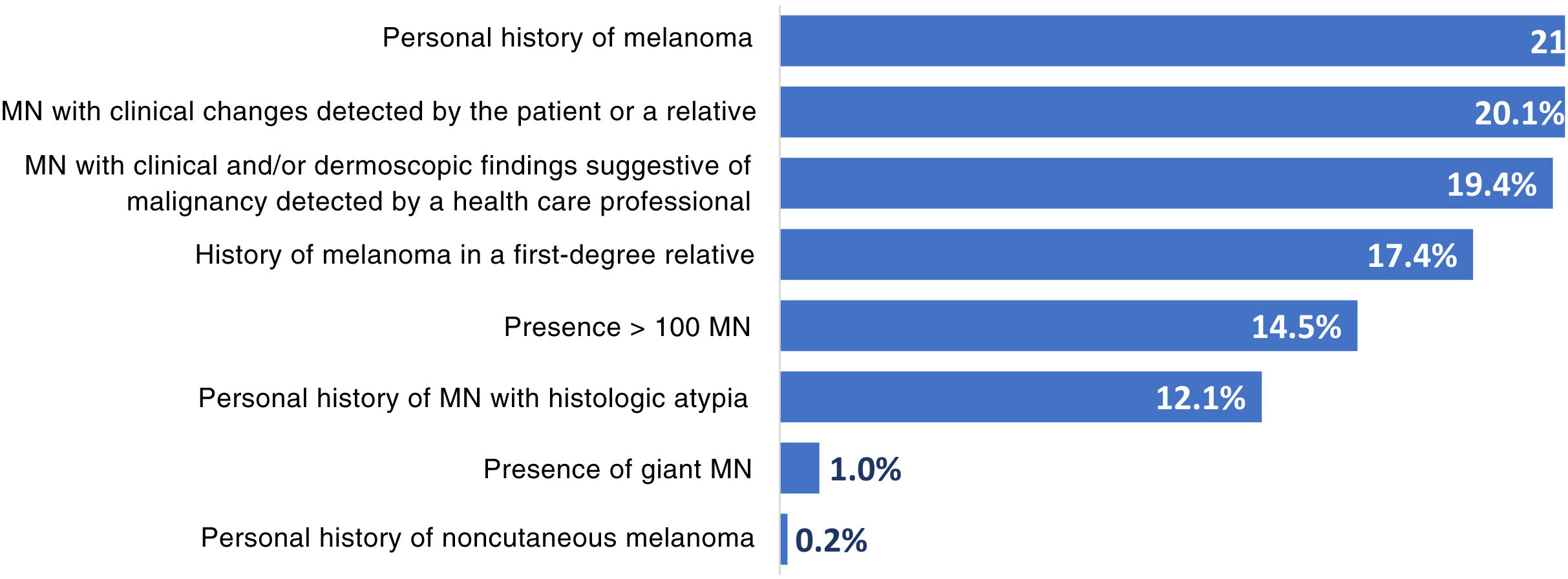
The reasons for referral are summarized in Fig. 1. The main reasons were a personal history of melanoma (21.5%), changes to lesions detected by the patient or a relative (20.1%), and clinical and/or dermoscopic features suggestive of malignancy detected by a health care professional (19.4%). Other reasons were a family history of melanoma (in a first-degree relative) (17.4%), presence of more than 100 melanocytic nevi (14.5%), a personal history of melanocytic nevi with histologic atypia (12.1%), presence of a giant melanocytic nevus (1.0%), and a personal history of noncutaneous melanoma (0.2%). Fifty-nine patients (14.3%) had more than 1 reason for referral.
The epidemiologic characteristics are shown in Table 1. Mean age at the start of follow-up was 40.3 years and mean follow-up time was 85.3 months. Overall, 96.9% of patients had Fitzpatrick skin type II or III. Most patients (85.5%) had fewer than 100 melanocytic nevi, and within this group, the largest category was 25 to 50 lesions. A personal and family history of melanoma was observed in 21.5% and 17.4% of patients, respectively.
Characteristics of Patients at High Risk for Melanoma.
| Total | Development of melanoma during follow-up | |||||
|---|---|---|---|---|---|---|
| Yes | No | P valuea | ||||
| Sex | ||||||
| Male | 222 (53.8%) | 29 | (13.1%) | 193 | (86.9%) | .54 |
| Female | 191 (46.2%) | 29 | (15.2%) | 162 | (84.8%) | |
| Fitzpatrick skin type | ||||||
| I | 8 (1.9%) | 0 | (0.0%) | 8 | (100.0%) | .42 |
| II | 222 (53.8%) | 35 | (15.8%) | 187 | (84.2%) | |
| III | 178 (43.1%) | 23 | (12.9%) | 155 | (87.1%) | |
| IV | 5 (1.2%) | 0 | (0.0%) | 5 | (100.0%) | |
| Age | ||||||
| <40 | 228 (55.2%) | 14 | (6.1%) | 214 | (93.9%) | .00 |
| 40–65 | 163 (39.5%) | 32 | (19.6%) | 131 | (80.4%) | |
| >65 | 22 (5.3%) | 12 | (54.5%) | 10 | (45.5%) | |
| No. of nevi | ||||||
| <25 | 92 (22.3%) | 18 | (19.6%) | 74 | (80.4%) | .34 |
| 25–50 | 178 (43.1%) | 21 | (11.8%) | 157 | (88.2%) | |
| 50–100 | 83 (20.1%) | 12 | (14.5%) | 71 | (85.5%) | |
| >100 | 60 (14.5%) | 7 | (11.7%) | 53 | (88.3%) | |
| Personal history of melanoma | ||||||
| Yes | 89 (21.5%) | 9 | (10.1%) | 80 | (89.9%) | .23 |
| No | 324 (78.5%) | 49 | (15.1%) | 275 | (84.9%) | |
| Family history of melanoma | ||||||
| Yes | 72 (17.4%) | 9 | (12.5%) | 63 | (87.5%) | .68 |
| No | 341 (82.6%) | 49 | (14.4%) | 292 | (85.6%) | |
A total of 178 lesions suspicious for melanoma were excised during follow-up. The diagnosis was confirmed in 76 lesions (58 patients [14%]), giving an NNE of 2.34 per melanoma. Twenty-eight melanomas (36.8%) were intraepidermal melanomas and 64 (84.2%) had a thickness of 1mm or less (median, 0.40mm). Sixteen melanomas (21%) were associated with melanocytic nevi. Most of the melanomas (70.7%) had been excised following dermoscopic observation of changes. The rest (29.3%) had been excised following detection of clinical changes by the patient or a health care professional.
The associations observed between high-risk factors and development of melanoma during follow-up are shown in Table 1. Older age was the only significant factor. More than half of the patients aged over 65 years of age (54.5%) developed at least 1 melanoma during follow-up, compared with 19.6% of patients aged between 40 and 65 years and 6.1% of those younger than 40 years.
DiscussionWe have described the reasons for referral to a dedicated dermoscopy unit, epidemiologic characteristics of patients at high risk for melanoma, and factors associated with the development of melanoma. We also analyzed the NNE per melanoma diagnosed.
Dedicated dermoscopy units offer clear benefits for both the health care system and patients at high risk for melanoma as they improve diagnostic accuracy and reduce the number of benign lesions removed.3–6 Several classification systems are available for assessing individual melanoma risk, including those developed by Riegel and Kraemer, which analyze number of melanocytic nevi and personal and family history of melanoma and/or dysplastic melanocytic nevi. The association between the number of melanocytic nevi and melanoma risk is complex.7–9 Several studies have shown that melanoma, and in particular nevus-associated melanoma, is more common in patients with high nevus counts.10 The risk seems to increase with the number and size of nevi and also appears to be higher for patients with nevi (especially atypical nevi) located in certain parts of the body, such as the arms.11 Other authors, however, have observed that most patients with melanoma have few melanocytic nevi.12 Dermoscopic follow-up does not appear to offer additional benefits to patients who have multiple nevi without other risk factors.11 Accordingly, a high nevus count without additional risk factors should probably not be one of the main factors considered when deciding on the need for dermoscopic follow-up.
Our results confirm that age is a significant risk factor for the development of melanoma.13 Age is also a strong independent prognostic risk factor in melanoma. Indeed, the increasing age of the population is a primary reason why melanoma death rates are not declining.14 Older patients thus would probably benefit most from follow-up at a dedicated dermoscopy unit, particularly if they have additional risk factors.
A personal history of melanoma has been linked to an estimated 9 to 13-fold increased risk of developing melanoma,15–17 and was the main reason for referral in our series. Although no significant differences were observed between patients with and without a personal history of melanoma, we believe that patients with a past history of melanoma should undergo regular examination at a dedicated dermoscopy unit.
A family history of melanoma is also a common reason for referral to dedicated dermoscopy units. When assessing risk in this setting, one should consider not only the number of relatives with a history of melanoma but also the number of melanomas in a given relative, as the risk in families with 2 or more first-degree relatives with a history of melanoma appears to be similar to that of families with just 1 first-degree relative with a history of melanoma involving 2 or 3 lesions.17
The NNE for each melanoma diagnosed in our study is lower than previously reported numbers, although differences could be due to study designs. Argenziano et al.18 studied 600 lesions in 405 patients with atypical pigmented lesions, Menzies et al.19 analyzed the results of 63 primary care physicians trained in dermoscopy, and Tromme et al.20 compared the findings of 46 dermatologists divided into 3 groups. In any case, our study confirms that dedicated dermoscopy units can benefit patients and help optimize health care resources.
ConclusionsThe main reasons for referral to a dedicated dermoscopy unit at a tertiary care hospital were a personal or family history of melanoma, detection of changes to a lesion, and the presence of clinically or dermoscopically atypical lesions. Older age was also associated with an increased risk of melanoma. Older patients, and particularly those with additional risk factors, would probably benefit most from follow-up at one of these units.
Conflicts of InterestThe authors declare that they have no conflicts of interest.