A previously healthy 37-year-old man from southern brazil presented with painful ulcerated facial lesions that had shown progressive growth over approximately 8 years. The condition initially involved the oral mucosa and, after several years, extended to the ocular region.
He had sought medical attention in various health care centers undergoing topical therapy. No supplementary tests had been performed, and he had been repeatedly treated with topical antifungal creams without improvement. a humble patient, he had not sought additional medical opinions. He also reported shortness of breath.
Physical examinationUpon examination, he presented with extensive erythematous and crusted plaques with infiltration in the chin area, lower lip, and right periocular region, with presence of eyelid synechia and microstomia (Fig. 1). Additionally, he experienced dyspnea during the consultation (Fig. 1).
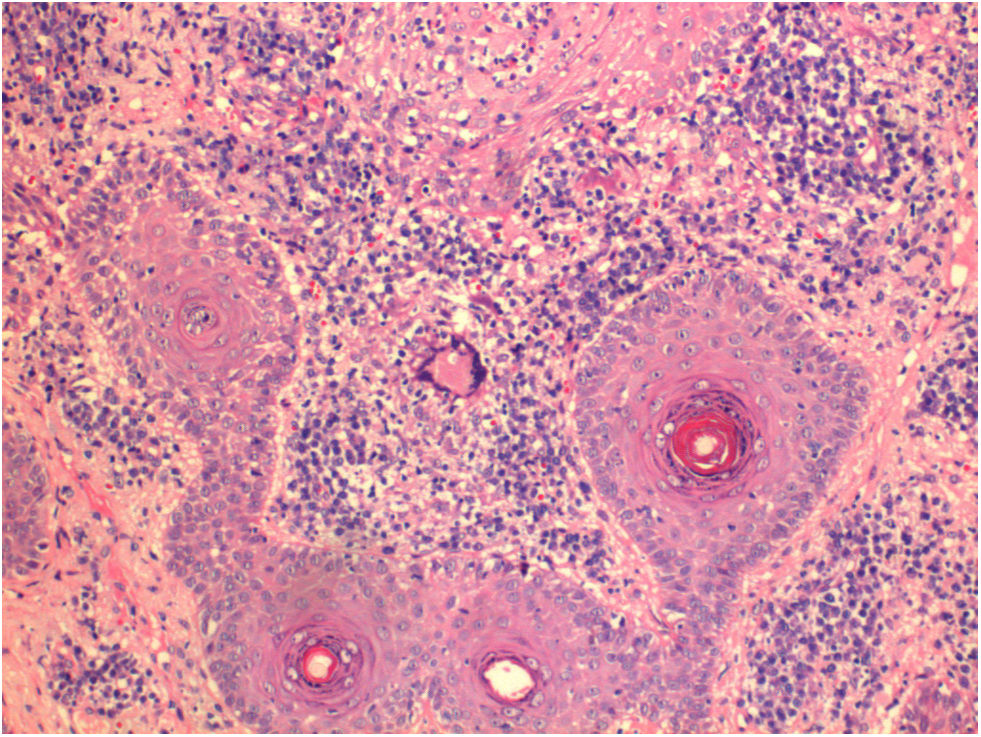
HistopathologySee Fig. 2.
Supplementary testsThe chest X-ray revealed the presence of bilateral and diffuse reticulonodular infiltrates. Serologies, liver function tests, renal function and complete blood count showed no abnormalities. The patient has not yet been evaluated by a pulmonologist, as he reported improvement in dyspnea. For now, a repeat chest X-ray has not been performed.
On the ophthalmological examination, the patient presents corneal adhesion with the skin covering the surface of the eyeball. Awaiting orbital CT scan.
What is your diagnosis?
DiagnosisParacoccidioidomycosis.
Progression and treatmentTreatment with itraconazole was initiated, with an excellent response at 3 months (Fig. 3).
DiscussionParacoccidioidomycosis is still a disease difficult to diagnose. Delayed diagnosis increases the risk of complications related to the disease, which can lead to severe and permanent sequelae. It is an endemic disease caused by dimorphic fungi of the genus Paracoccidioides and is a common condition in Brazil. The infection can affect the skin, lungs, mucous membranes, and GI tract. It can also reach systemic and fatal forms, making early recognition and diagnosis essential.1
The infection is more common in male rural workers. It can be attributed to patient exposure to soil, the natural habitat of the fungus.2 The primary route of entry is inhalation of the pathogen, leading to its establishment in the host's lungs. It is categorized into two clinical forms: an acute form, more common in children, and a chronic form, typically affecting adults older than 30 years.3
After exposure, most patients will restrain the disease, keeping it in a latent form, thus preventing the spread of the infection. However, due to loss of immune balance, the infection can progress and give rise to an advanced disease – the chronic form. Patients in whom systemic disease progresses without a latent phase present with the acute clinical form. More than 80% of cases represent the chronic form of the disease, and most of them have isolated pulmonary involvement or involvement in other systems simultaneously.3
Paracoccidioidomycosis can spread hematogenously or lymphatically, affecting any organ, including the skin, lymph nodes, and central nervous system. The head and neck regions are the most widely affected, and ulcerated lesions are more frequent.4 Diagnosis can be established through microscopic visualization of fungal elements and/or culture from clinical materials such as skin biopsy fragments or sputum. Direct microscopy using KOH provides the diagnosis in most cases.2
Spontaneous cure of the disease generally does not occur, and systemic antifungal treatment is often required. Among the options, itraconazole is the most widely prescribed treatment.5 Additionally, although trimethoprim-sulfamethoxazole may be used in some cases it requires prolonged therapy to prevent relapses.6 The duration of treatment depends on the clinical presentation but is usually 12–24 months.5 In the reported case, the patient initially underwent approximately 3 months of treatment with itraconazole, showing significant improvement evidenced in the figures.
Early recognition of this disease is of paramount importance due to the possibility of systemic dissemination if treatment is not initiated. Despite being endemic in our region, cases of late diagnosis with the presence of permanent sequelae are still common. Our patient neglected his health condition, and due to difficulty accessing high-complexity hospitals, his condition worsened dramatically. Therefore, it is necessary to highlight the existence of this disease, which is still so neglected in Brazil to be able to prevent severe cases from keep happening.
Conflicts of interestThe authors declare no conflicts of interest.