Concern for patient safety has always been an important issue in clinical practice, but the most recent interest in the topic dates back to the 1970s, when malpractice in the United States gave rise to a large number of lawsuits against doctors, endangering the sustainability of the health system. Today, in the second decade of the 21st century, we can no longer describe it as a silent epidemic as the issue of patient safety has been the focus of significant media attention all over the world, particularly following the publication of the US Institute of Medicine report entitled To Err Is Human: Building a Safer Health System published in 1999.1
Referring back to the findings of an earlier study on healthcare-related harm in patients, the report discusses the issue from the point of view of the healthcare system and its social and economic repercussions,2 with particular emphasis on the shocking estimate that between 48 000 and 96 000 people die in US hospitals every year as a result of medical errors. The frequency of healthcare-related errors and the effects, repercussions, and implications of such failures make patient safety a serious public health problem. This is perhaps the most important message of the present article.
Patient safety is also a concern in the field of dermatology. In fact, one of the volumes of the collection Errores Diagnósticos y Terapéuticos y maneras de evitarlos (Diagnostic and Therapeutic Errors and Their Avoidance) edited by Dr. J. Schwalbe and published in 1923 by Manuel Marin in Barcelona, dealt precisely with the subject of venereal and skin diseases: Enfermedades venéreas - Enfermedades de la piel - (especialidades enfermedades venéreas y cutáneas) by Dr. Riecke and Dr. Bettmann.
The primary goal of the physician is to do no harm to the patient, and this precept continues to occupy first place today even though its origins stretch back 2000 years to the time the Greek physician Hippocrates established the principle of “primum non nocere.” However, a great deal still needs to be done to improve the “culture of patient safety” and to transform the existing reactive and punitive culture into a proactive culture based on the participation of all healthcare professionals.
Conceptual FrameworkTwo of the meanings of the word “seguridad” (safety) in the Real Academia Española dictionary are relevant to the way we use the term in clinical practice: Calidad de seguro (the condition of being safe) and fianza u obligación de indemnidad a favor de alguien (a security or obligation to indemnify someone). The former refers to the usual meaning of “seguro” (safe), which we interpret to mean free of danger. The latter encompasses the concept of the system's responsibility to the patient to fulfill the implied contract.2,3
In the context of healthcare, particularly with respect to clinical safety, it is not possible to be categorical about safety because no one can guarantee that medical management will be totally free of all harm; our work must, rather, be guided by the essential analysis of risks and benefits undertaken to ensure that the expected result represents the greatest benefit for the patient.
Safety is an indispensable component of quality healthcare: first, do no harm, while accepting that healthcare will always be associated with a minimum inevitable but acceptable level of risk. The World Health Organization (WHO) recommendations define patient safety as “the reduction of the risk of unnecessary healthcare-related harm to an acceptable minimum.”4
Patient safety is, therefore, a result of the interaction between the many actions of the health system and health professionals and the balance achieved. Risk is an inherent component of all care or medical management, and it is expressed in different ways; it may be a result of whether or not the patient is affected, of the patient's vulnerability, of human errors, or of system failures. At this point, it is necessary to include a brief account of the main events that have led us to this concern for patient safety.
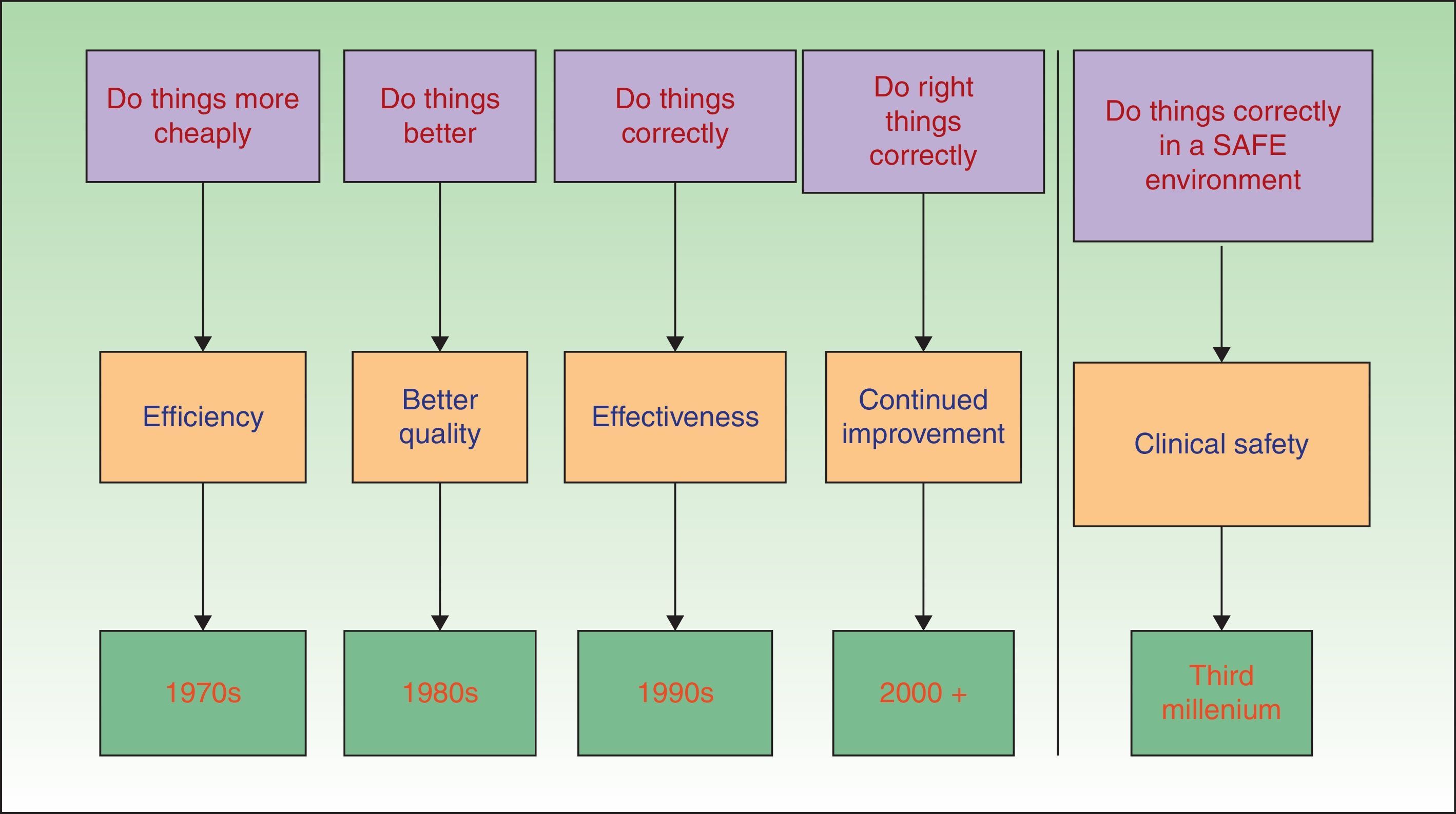
In the 1970s, the main focus of the pursuit of excellence in healthcare was on improving the scientific and technical aspects of care. The 1980s and 1990s were characterized by a growing interest in ways of ensuring the appropriate use of healthcare resources and of improving patient satisfaction.5 In this century, the subject of real interest in healthcare, and the area on which the major international organizations are now focusing their attention, is the further improvement of quality by enhancing patient safety—the foremost concern of all medical management (Fig. 1). Using the glossary developed by the WHO,4 we can identify the different elements that play a major role in patient safety:
- -
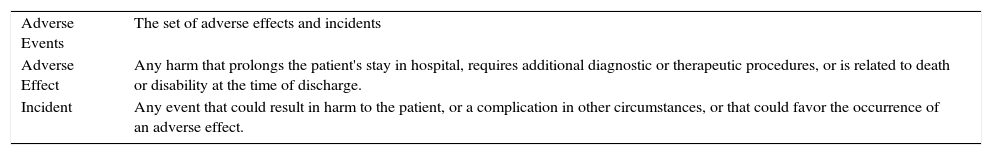
Patient safety incident: an event or circumstance that could have resulted, or did result, in unnecessary harm to a patient. In practice, incidents that have resulted in harm to the patient are called adverse effects (Table 1).6
Table 1.Working definitions of adverse events.
Adverse Events The set of adverse effects and incidents Adverse Effect Any harm that prolongs the patient's stay in hospital, requires additional diagnostic or therapeutic procedures, or is related to death or disability at the time of discharge. Incident Any event that could result in harm to the patient, or a complication in other circumstances, or that could favor the occurrence of an adverse effect. - -
Contributing factor: A circumstance, action or influence which is thought to have played a part in the origin or development of an incident or to increase the risk of an incident.
- -
Contributing factors are classified as human errors, system failures, or patient characteristics.
- -
Patient outcomes
- •
Harm implies impairment of structure or function of the body and/or any deleterious effects arising therefrom.
- •
Disease is a physiological or psychological dysfunction.
- •
Injury is damage to tissues caused by an agent or event.
- •
Suffering is the experience of anything subjectively unpleasant.
- •
Disability implies any type of impairment of body structure or function, activity limitation and/or restriction of participation in society, associated with past or present harm.
- •
- -
Organizational outcomes
- •
Ameliorating action. This is an action taken or circumstance altered to make better or compensate any harm after an incident. The aim of such actions is to recuperate the patient's clinical situation and to deal with the repercussions of the event on the organization. An example of the former would be hydration of a patient presenting with nausea and vomiting due to medication.
- •
Actions taken to reduce risk. These are actions taken to reduce, manage, or control the harm or probability of harm associated with an incident. Such actions may be directly related to incidents or contributing factors, or may be informed by detection, mitigating factors or ameliorating actions. They can be proactive (before an incident occurs) or reactive (based on knowledge learned from observation of an incident).
- •
System barriers. These are the measures in place aimed at reducing the frequency of incidents or increasing the system's capacity to detect them. The set of measures that aim to mitigate the impact of an adverse effect on the patient or intended to remedy it include what are termed contingency plans.
- •
Resilience. This term refers to the degree to which a system continuously prevents, detects, mitigates, or ameliorates hazards or incidents.
- •
The many dimensions of patient safety include ensuring the safety of the environment and equipment, the prevention of healthcare-related infections, the safe use of medicines, safety in clinical procedures and practice, and effective communication on every level.
It is, therefore, a concept that encompasses actions aimed at eliminating, reducing, and mitigating preventable adverse events resulting from a healthcare process, in our case dermatological. It also includes the promotion of practices that have been shown to be safer and favoring a cultural shift away from the reactive culture that seeks to blame professionals for errors.
In short, patient safety is a area that requires a shared effort on the part of managers, healthcare professionals, and patients. It is an issue that all dermatologists should be concerned with and an area in which we should all work to improve.
Patient Safety vs Risk Management: The International FrameworkIt is interesting to note that a revolution has been occurring in the area of patient safely over the last 10 years. In May 2004, the 57th World Health Assembly approved the creation of the World Alliance for Patient Safety (WAPS) (http://www.who.int/patientsafety/en), a body that was launched in October 2004. WAPS was created to provide leadership for the international initiative involving countries, international organizations, and other stakeholders, and its objective is to facilitate and promote the implementation of programs aimed at improving the safety of healthcare worldwide.
The WAPS has, to date, launched 10 programs related to priority action areas:
- 1
The aim of the Global Patient Safety Challenges is to identify priority actions that can eliminate significant risks to patients relevant to member countries. The actions carried out include the following:
- •
From 2005 to 2006, the topic chosen was nosocomial infections under the banner “Clean care is safer care.” The program proposed hand hygiene as the simplest and most effective method for preventing healthcare-associated infections.
- •
The topic chosen for the 2007-2008 program was safe surgery, under the banner “Safe surgery saves lives.” The goal was to reduce deaths due to complications following surgery by establishing safe standards of practice, developing and distributing clinical practice guidelines, and defining and implementing safety measures.
- •
- 2.
Patients for patient safety. The aim of this campaign is to bring the voices of patients to the forefront of the worldwide movement working to improve patient safety. The program is building a global network of patients and patient organizations to facilitate their involvement in all patient safety initiatives.
- 3.
Reporting and learning. The aim of this initiative is to promote the development of adverse event reporting systems that will facilitate analysis of the available data and the detection of the causes of such events. The ultimate goal is to make recommendations aimed at preventing the recurrence of future incidences.
- 4.
Taxonomy. The aim of the International Classification for Patient Safety is to harmonize the concepts involved in patient safety and to create an internationally agreed classification that will promote more effective learning.
- 5.
Research. Research for patient safety undertakes international studies on patient safety to achieve safer healthcare in all member countries.
- 6.
Solutions for patient safety. In collaboration with the Joint Commission International (www.jointcommissioninternational.org), this program designs interventions of proven efficacy aimed at preventing or minimizing healthcare-associated harm to the patient. In 2007, the executive committee of this organization's collaborating center approved aide memoirs on the so-called “9 patient safety solutions.”
- 7.
Safety in action. The aim of this program is to promote good practices in healthcare organizations to improve patient safety.
- 8.
Technology and education for patient safety. The focus of this program is to find ways to harness new technologies to improve safety; for example, the use of simulation methods, robotic systems, and automation to reduce risks to patients.
- 9.
Patient safety and the care of critically ill patients. The purpose of this initiative is to identify priority actions that will improve the care of patients in critical condition.
- 10.
Exemplary hospitals. The aim of this program is to promote learning of best practice in patient safety in hospitals around the world.
In July 2004, the European Commission (http://ec.europa.eu/) established a High Level Group on health services and medical care. This was a platform for expert cooperation including a working group specifically on patient safety issues (Patient Safety Working Group), which brought together representatives of the 27 member states, professional organizations, patients, and the major international organizations involved in patient safety.
Spain's Ministry of Health plays an active role in the WAPS programs. The Ministry of Health, Social Services and Equality recently contacted the AEDV, which in turn asked me, to collaborate on the preparation of a strategy paper on Patient Safety in the National Health Service for the period 2015 to 2020. The resulting document has been approved by the Patient Safety Strategy Institutional Committee on which numerous scientific associations are represented. Several experts, including Dr. Aranaz, were consulted.
Concluding this second section, we might reflect that patient safety could become an area of action similar to those of health promotion, risk management, and disease prevention.
Competitive Risks and Homeostasis of RiskIn reality, safety and risk are not 2 different concepts, but rather points on a continuum moving from a lesser to a greater degree of risk to the patient. Risk and safety are held in a dynamic balance by the sinuous line that joins and separates them: when one increases, the other diminishes.
Patient safety is the result of the balance arising from the continuous interaction between 2 sets of factors: first, a series of latent conditions that includes the quantity and quality of available resources, the culture of safety, and the characteristics of the institutional setting; and, second, the teams and professionals working in the healthcare system. Although the central focus of patient safety is the prevention of adverse events caused by healthcare rather than the complications or consequences of the unfavorable evolution of the patient's disease owing to its natural course, certain population characteristics—such as aging, difficult social and economic conditions, low educational level, and a lack of family support—do constitute a threat to patient safety because they increase the vulnerability of the individual.
One of the paradigms used to explain patient safety is the “Swiss cheese” model in which the barriers or safeguards intended to reduce the risks or dangers associated with healthcare and to protect the patient from adverse effects are represented as a series of slices of cheese in which the holes represent the imperfections in the system. When the holes in a series of barriers line up, an adverse event occurs.
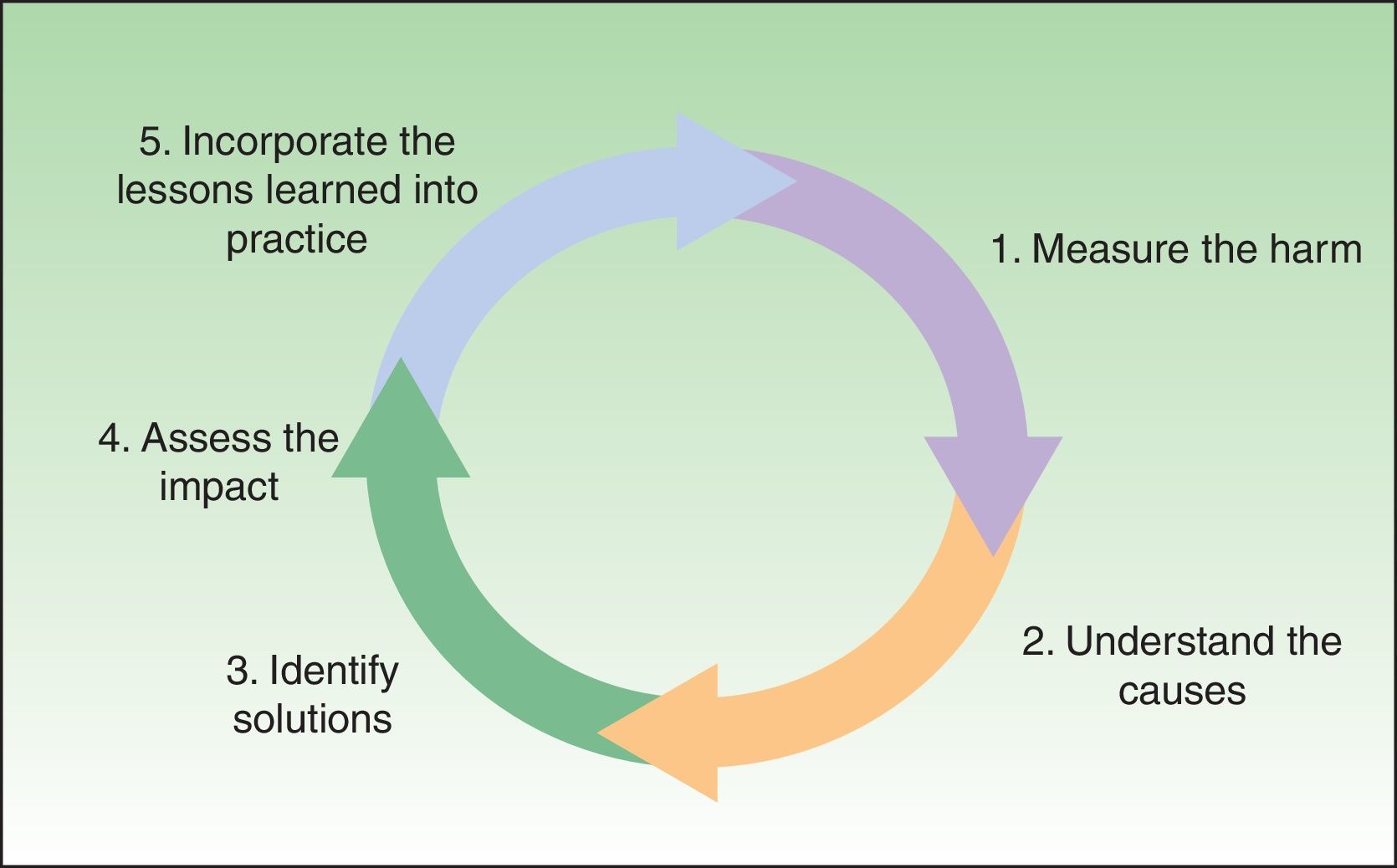
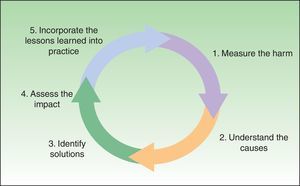
Patient Safety: Outlook and Research GoalsThe framework suggested by the WHO is very useful for reviewing the many aspects of patient safety. The diagram shows the 5 steps that make up what is called the “patient safety research cycle” (Fig. 2). The cycle is as follows: first, to measure the harm caused; second, to analyze the contributing factors; third to identify solutions; fourth, to evaluate the impact of these solutions; and fifth, to close the cycle and start afresh by making changes (Fig. 2).7
Measuring HarmThe methodology developed on the basis of the IDEA study (http://proyectoidea.com/) and used in the national study on healthcare-related adverse events in Spain (the ENEAS study),8 facilitates the analysis of associations between adverse events identified and the characteristics of both the patients and the medical management, making it possible to propose a hypothesis concerning the risks associated with adverse events, and to contribute strategies and solutions appropriate to the Spanish setting.
Understanding the Causes: Analyzing the Contributing FactorsA review of the studies in the literature on the incidence of adverse events in general hospitals draws attention to the need for a more in-depth understanding of the causes of safety problems. All the studies sought to identify the role played by certain patient characteristics in the origin of adverse events. The ENEAS study highlighted the fact that, in Spain, patient vulnerability is a crucial factor in healthcare-related adverse events. Patients with intrinsic risk factors were 1.6 times more likely to experience adverse events. The risk for people over 65 years of age with extrinsic risk factors was 2.5 times that of patients without such risk factors aged 65 or under.
The 3 most common types of adverse events identified in the ENEAS study were as follows: events associated with medication use (37.4%), healthcare-associated infections (25%), and events related to technical problems during a procedure (25%). Almost half (42.8%) of the adverse events were considered preventable.
The model used to explain the causal cascades leading to an adverse event indicates that system failures play a more important role than human error. Latent failures are like the root causes and can give rise to new cascades of adverse events.9 The studies reviewed indicated that the immediate causes of 70% of adverse events are technical failures, errors in decision-making, failures to take the most appropriate action given the available information, problems with medical history taking, a lack of necessary care, and the use of inappropriate care. Particular consideration was given to the pressure on the healthcare system as a source of adverse effects.
Identifying SolutionsWe can improve clinical safety and reduce the probability of patient safety incidents by eliminating superfluous actions liable to cause adverse events and by taking steps to prevent human errors. We can also monitor the areas of the healthcare system susceptible to failure and take action to prevent possible harm or minimize the consequences of system failures. To do this we can use primary, secondary, tertiary, and even quaternary strategies.
The aim of primary prevention is to strengthen the factors that enhance safety, to reduce the factors associated with risk and latent failures (root causes), and to reduce the incidence of adverse events (repeat occurrence). These goals can be achieved by increasing professional training and patient education on the topic, promoting a proactive culture of safety, implementing safe clinical practices and evidence-based protocols, and broadening the scope of clinical alerts.10
Secondary prevention is the early detection of adverse events or the neutralization of the consequences of an event that was not avoided. The most efficient way of doing this is to put in place epidemiological surveillance systems.
Tertiary prevention involves reducing the negative impact of adverse events (sequelae, disability, pain, suffering) and preventing the recurrence of such events or making it less likely. The tools used to do this are registries and reporting systems, reconciliation committees, and compensation systems.
Quaternary prevention refers to the actions taken to identify patients at risk for overtreatment, to protect them from further medical interventions. It includes suggesting ethically acceptable alternatives. It is the set of health activities undertaken to reduce or neutralize the consequences of unnecessary or excessive medical treatment or interventions based on insufficient evidence.
For more information on specific solutions, we recommend visiting the websites of the international organizations mentioned above and, in particular, careful reading of the 9 solutions proposed by the WHO,11 which is an extraordinarily useful document.
Assessing ImpactTo evaluate the impact of an adverse event, we need to define indicators that can assess percentages of change. For this purpose we can use both process indicators, such as the rate of correct perioperative antibiotic prophylaxis, and outcome indicators, such as the rate of healthcare-related infections, the number of medication errors, or the number of readmissions within 7 days of discharge following surgery.
The study design most often used to assess impact is the quasi-experimental or before-after model. This was the design used to assess the impact of the introduction of the WHO surgical check list.12 That study revealed a 50% reduction in infection rates (6.2% to 3.4%) and mortality rates (1.5% to 0.8%), statistically significance differences in both cases.
Incorporating Solutions into Clinical Practice: Promoting ChangeIf we want to drive change we must first understand the prevailing culture of safety. The US Agency for Healthcare Research and Quality (AHRQ) provides a questionnaire designed to that effect, which identifies areas where action needs to be taken to improve the culture and to move from a reactive to a proactive approach; the same questionnaire also facilitates monitoring of progress and outcomes.13
By Way of ConclusionThe modern era has brought about a different way of articulating the 2 duties of the physician we mentioned earlier: to do good and not to harm. Now the priority will be to balance risks and benefit as a key element in the clinician's decision-making process. Furthermore, effective actions for the patient's good can no longer be undertaken without involving the individual and obtaining his or her consent, out of respect for the principle of autonomy. Thus, the priority today in the third millennium, as underscored by the WHO campaign, is “First, do no harm.”
In the context of an increasingly globalized healthcare framework, we face the challenge of providing a safer healthcare environment, in which effective communication between professionals, and between professionals and patients is a key tool for improvement: we learn from our mistakes. It is not surprising that communication failures between professionals are the main root cause of sentinel events, and failure to communicate effectively with patients favors the occurrence of adverse events and increases the frequency of claims and litigation.
As a final conclusion, it is important to make the point that dermatologists need to become more aware of the importance of patient safety. Although, it might be thought that our specialty does not carry the same risks as others, such as Intensive Care, Infectious Diseases, or General Surgery, in which there have been great efforts to implement safety protocols, our patients will also benefit from the implementation of an appropriate culture of patient safety.
Please cite this article as: de las Heras-Alonso M, Aranaz-Andrés J. Primum non nocere, o como trabajar con seguridad para el paciente. Actas Dermosifiliogr. 2016;107:269–274.