Amyloidoses are a heterogeneous group of diseases characterized by abnormal extracellular deposits of amyloid in tissues, which are derived from the degradation of various proteins and has multiple origins. There are 2 variants in which amyloid derives from the light chains of immunoglobulins: primary systemic amyloidosis and primary cutaneous nodular amyloidosis (PCNA). Both are manifestations of a plasma cell dyscrasia. In the latter, this dyscrasia is localized, with a low risk of progression to systemic disease. Among cutaneous amyloidoses, PCNA is very rare.1,2
Two cases of cutaneous nodular amyloidosis are described below.
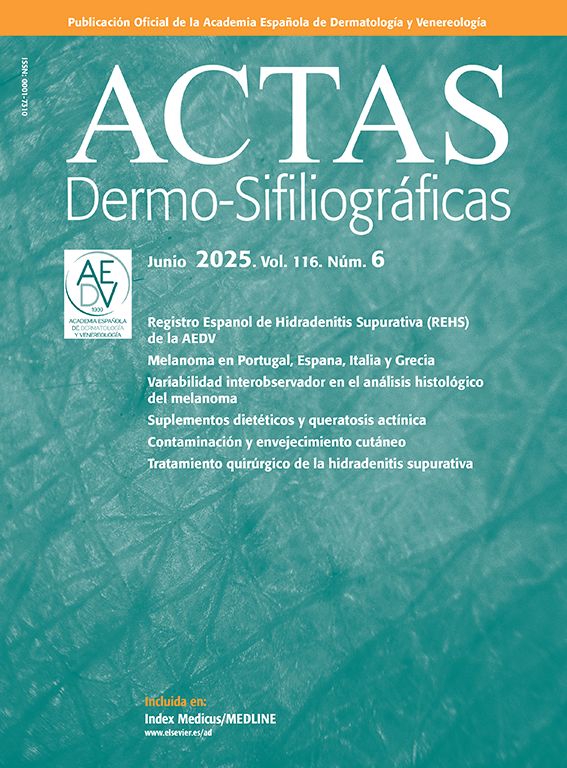
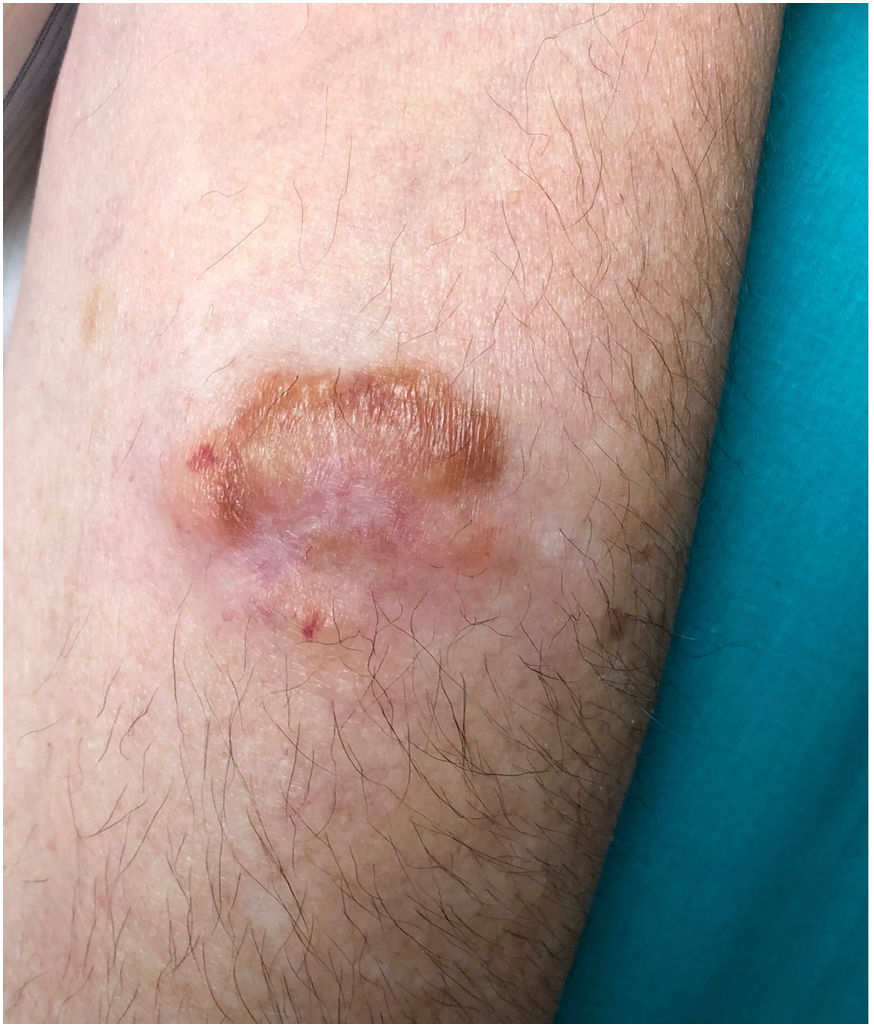
Case #1: A 62-year-old woman, with no relevant past medical history, presented with a several-year history of a yellowish, infiltrated, alopecic plaque on the scalp—approximately 4cm2 in diameter—(Fig. 1). A similar 1cm lesion was found in the right parietal area. The lesion was biopsied, and hematoxylin-eosin (HE) revealed the presence of an amorphous eosinophilic material occupying the entire dermis. This material stained red-orange with Congo red and showed apple-green birefringence under polarized light. The only analytical change reported was elevated levels of lambda light chains (2.19mg/dL2). Systemic involvement was ruled out, and a diagnosis of PCNA was established, which was treated with a triamcinolone acetonide infiltration resulting in a flattening of the lesion. The patient did not show systemic progression or develop new lesions over the next 10 years. Persistent elevation of lambda light chains was noted in the lab test results.
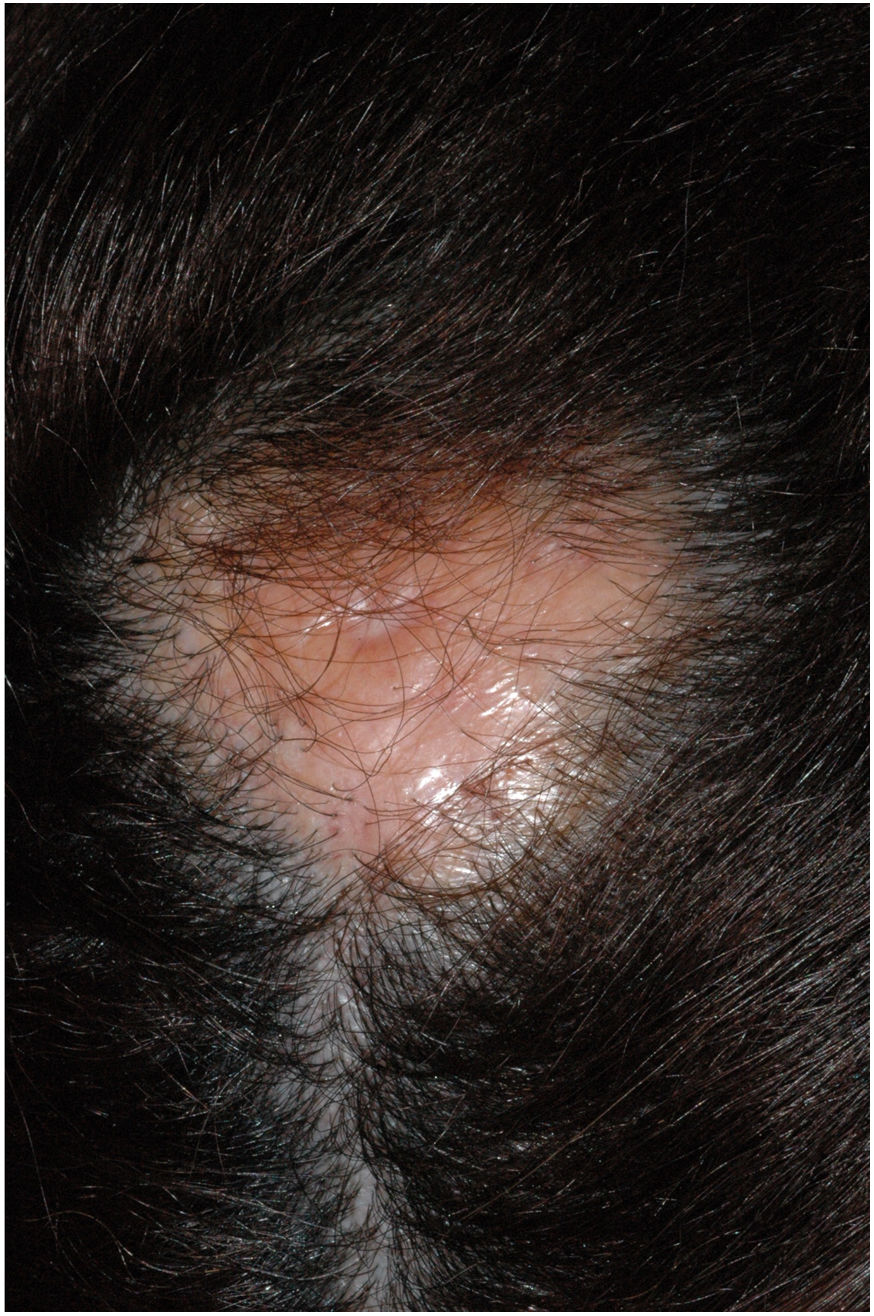
Case #2: A 69-year-old man with hypertension presented with a 1-year history lesion on the left forearm. Physical examination revealed the presence of a lobulated, elastic plaque about 4cm2 in diameter with a blister on its surface (Fig. 2). Ultrasound showed a well-demarcated, hypoechoic, heterogeneous oval nodule involving the dermis and subcutaneous tissue. Histological study with HE revealed a deposit of amorphous eosinophilic material distributed across the dermis, subcutaneous tissue, and perivascularly, associated with a plasma cell infiltrate. The material was Congo red-positive and showed green birefringence under polarized light (Fig. 3). Systemic involvement was excluded. The only observed analytical change was elevated levels of kappa and lambda light chains (4.71mg/dL2 and 3.34mg/dL2, respectively). Diagnosis was PCNA, which was treated with surgical excision. The lesion did not recur, and the patient did not any develop systemic amyloidosis at the 5-year follow-up
PCNA is more common in adults between 50-60 years, without sex predilection.1,3 PCNA has been associated with Sjogren's syndrome in multiple reports.3 Although PCNA shows as often solitary waxy nodules or infiltrated plaques, they can be multiple, skin-colored, or with a pinkish or yellowish hue.1 Lesions are often found on acral areas,3 in order of frequency: lower extremities, head, trunk, upper extremities, and genitals.2
Histology shows a deposit of amorphous eosinophilic material with HE. Porphyria, lipoid proteinosis, Waldenström macroglobulinemia, and primarily, colloid milium, should be considered in the differential histological diagnosis of this disease. Although colloid milium also stains with Congo red, it does not present apple-green birefringence.
In PCNA, the amyloid deposit occupying the entire dermis and subcutaneous tissue2 is composed of light chains of immunoglobulins (kappa and/or lambda). It is often associated with a plasma cell infiltrate located around blood vessels or skin appendages. These findings are indistinguishable from those of primary systemic amyloidosis.2 It is believed that plasma cells produce the amyloid, and genetic rearrangement studies have confirmed the monoclonality of these cells in the lesional skin, without evidence of clonal proliferation of plasma cells in the bone marrow.3 However, since 7% of cases progress to systemic disease,1,2 long-term follow-up is advised.
Multiple options for local treatment have been described.1,2 Nodules can be surgically removed or treated with corticosteroid infiltrations, cryotherapy, laser, among others. However, recurrence is common.1,2
Although rare, PCNA should be included in the differential diagnosis of infiltrated plaques, nodules, or tumors, especially if located on acral areas. It is important to rule out systemic disease and ensure follow-up.
FundingNone declared.