Teledermatology is the most advanced clinical specialty in telemedicine. The development of teledermatology in specific countries has not been studied in depth.
MethodsOur objective was to analyze teledermatology models in clinical practice in Spain. We paid special attention to organization, technical aspects, training, and the advantages/disadvantages as seen by teledermatologists. Two surveys were carried out (2009 and 2014).
ResultsTeledermatology was used at 25 centers in 2009 and at 70 in 2014. The extended survey was completed by 21 centers in 2009 and 41 in 2014. Store-and-forward teledermatology was the main technique (83%) in 2014. Only 12% of centers used the real-time method, and 5% used a hybrid modality. Patients lived less than 25km away in 75% of cases (urban teledermatology). Most centers used mid-range bridge cameras; only 12% used mobile phones. Teledermoscopy and tertiary teledermatology were each used in 15% of centers. Teledermatology was restricted to skin cancer in 25% of cases, and 66% of centers used it to train primary care physicians. The main advantages, assessed on a scale of 1 to 10, were prioritization in cancer screening (8.3), rapid emergency care (7.8), training of and communication with primary care physicians (7.6), screening for trivial conditions (7.6), and reduction in the number of face-to-face visits (7.6). The main disadvantages were poor image quality (6.3), fear of error (5.7), difficulty in coordinating with primary care physicians (3.8), and time commitment (3.3). Between 2009 and 2014, the number of centers using teledermatology and the number of teledermatologists increased, as did use of the store-and-forward and urban models. The technology used also improved.
ConclusionTeledermatology is an emerging technology that is becoming well established in Spain. More than 25% of dermatology centers in Spain have implemented a teledermatology model. Store-and-forward in an urban setting is the most widely used modality. Teledermatologists see this technology as an effective option with more advantages than disadvantages. General satisfaction is high, although there is room for significant improvement in some areas.
La teledermatología (TD) es la especialidad clínica más desarrollada de la telemedicina. El desarrollo de la TD en un país completo no se ha estudiado previamente en profundidad.
MétodosEl objetivo fue analizar los modelos de TD en práctica real en España, centrándose en la organización, los aspectos técnicos, la docencia y las ventajas/desventajas percibidas por los teledermatólogos. Se realizaron 2encuestas con teledermatólogos en 2009 y 2014.
ResultadosSe identificaron 25 centros utilizando TD en 2009 y 70 en 2014. La encuesta ampliada fue completada por 21 centros en 2009 y 42 en 2014. Las características generales en 2014 fueron: TD almacenamiento (TDA) fue la técnica predominante (83%), solo el 12% TD en tiempo real y el 5% TD híbrida. El 75% de los pacientes vistos en TD viven a menos de 25 km (TD urbana). La mayoría de los centros utilizan cámaras bridge de gama media y solo el 12% utiliza los teléfonos móviles. El 15% practica teledermoscopia y el 15% TD terciaria. En el 25%, la TD se restringió a la oncología cutánea; el 66% utiliza la TD para formación de médicos de primaria. Las ventajas principales (puntuación 0-10) fueron priorización en oncología (8,3), asistencia rápida de urgencias (7,8), la formación y la comunicación con los médicos de primaria (7,6), el cribado de enfermedad banal (7,6) y la disminución de las visitas presenciales (7,6). Los principales inconvenientes fueron (puntuación 0-10): la baja calidad de imágenes (6,3), el miedo al error (5,7), difícil coordinación con los médicos de primaria (MP) (3,8) y consumo de tiempo (3,3). La evolución 2009-2014 mostró más centros con TD y más teledermatólogos, mejor tecnología y aumento de los modelos TDA y urbano.
ConclusiónLa TD es una tecnología emergente que comienza su fase de consolidación en España. Más del 25% de los centros de dermatología en España han puesto en práctica un sistema de TD. El modelo predominante es TDA en un entorno urbano. Los dermatólogos perciben la TD como una opción efectiva con más ventajas que desventajas. La satisfacción general es alta, sin embargo, todavía hay áreas que necesitan mejoras significativas.
Teledermatology (TD)—the practice of dermatology by means of communication technologies—is considered to be the most advanced clinical specialty in telemedicine.1,2 Store-and-forward TD, based solely on still photography, is becoming more common at the expense of real-time TD, which involves videoconferencing.3 TD is also the most widely studied telemedicine specialty.4,5 Despite the growing popularity of the practice, it is not clear whether TD should be considered a mature application,6,7 especially with regard to health outcomes in clinical practice. In fact, TD has been widely debated in some countries where the practice has a long tradition, including the United Kingdom8 and Spain.4 The large-scale utility of TD as a diagnostic instrument has been demonstrated in the Netherlands.9 Despite the apparently incremental increase in the use of this approach around the world, there have been very few studies on the implementation and characterization of TD modalities in developed countries. The exception is an interesting study from 2012 on the practice models and real-world challenges associated with TD in California, which provides an in-depth analysis of TD practice in the state.10 The following year saw the publication of a longitudinal study that assessed the development of TD programs in the United States (US) between 2003 and 2011.11
Given the scarcity of research on this subject, it can be difficult for dermatologists to obtain relevant information about practice models and the potential challenges associated with TD. Moreover, we believe it is important to understand the development of this technology outside of the United States, particularly in Spain—hence our motivation for the present study. The main objectives of this study were to analyze the extent of TD implementation in Spain and describe the most important characteristics of the practice, including organization, population served, technology, research, training, advantages, and disadvantages. We present the results of a comparative longitudinal study consisting of 2surveys, carried out in 2009 and 2014 by the Imaging Group of the Spanish Academy of Dermatology and Venereology (AEDV).
MethodsThe study was approved by the research committee at Hospital General Universitario de Ciudad Real. For the first survey, carried out in 2009, all AEDV members were contacted by email with the aim of identifying dermatologists who practiced TD. For the second survey, carried out in 2014 with the collaboration of AbbVie's Spanish sales network, the heads of all dermatology departments in Spain (n=267) were contacted in person and asked about TD use in their departments. The teledermatologists identified by both methods were asked to identify other teledermatologists who may not have been contacted.
Once the centers that used TD had been identified, they were sent a full survey by email in order to obtain an accurate description of each center's functional model. The authors developed the survey questions in collaboration with the Imaging Group's committee members. The questions focused on 5 areas: (a) characteristics and organization of the center; (b) operational considerations; (c) technical data; (d) objectives of TD at the center; and (e) challenges associated with TD use (advantages and disadvantages). The 2014 questionnaire was somewhat longer as it included more items than the 2009 version; as a consequence, certain comparisons were not possible.
ResultsA. Characteristics of centers that used TD: In 2009, after all AEDV members were contacted by email, we identified 25 centers that used TD, 21 of which (84%) completed an exhaustive survey. In 2014, all dermatology departments in Spain (n=267) were contacted in person. Of the 267 centers, 70 (26.2%) used TD (Fig. 1); however, only 42 centers (60%) completed the survey. In 2014, experience with TD ranged from 0.3 to 17 years; mean experience was 4.9 years. Consistent with the findings of the 2009 survey, in 2014 there were 24 centers with less than 4 years of experience and 17 with more than 5 years of experience. Only 5 centers had more than 10 years of experience. All centers that used TD belonged to the Spanish national health system and most were university hospitals (57%). Many teams had 5 or more dermatologists on staff (33% had 5-8 dermatologists; 24% had 9-15 dermatologists). Local hospitals with fewer than 4 dermatologists on staff accounted for 43% of the centers that used TD. On each team, telemedicine consultations were generally handled by a group of just 1 to 3 dermatologists. In 2009, just 15% of the centers spent more than 5hours per week on TD; by 2014, this figure had nearly doubled, to 29%. In 2014, 12 of 41 centers (29%) saw a large volume of patients by TD (more than 100 patients per month), while 8 centers (19%) saw fewer than 20 patients per month.
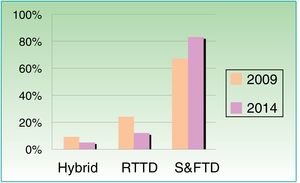
B. Health care organization and TD models: The number of centers with specific hours reserved for TD appointments increased from 8 of 21 centers surveyed (38%) in 2009 to 22 of 41 centers (53%) in 2014. In 2014, 24 of 32 centers (75%) used TD to treat patients who lived less than 25km away, while just 4 of 37 centers (11%) used TD to see patients who lived more than 100km away. The percentage of centers treating patients more than 100km away was nearly 4 times higher in 2009, when 8 of 21 centers (39%) reported this practice. These findings reveal a clear trend towards a more urban use of TD (Table 1). In Spain, 79% of teledermatologists and 75% of primary care physicians who practice TD do so without a nurse or other support staff. Such support is more common in real-time TD models. The store-and-forward TD model was used by 14 of 21 centers in 2009 (67%); this figure increased to 34 of 41 centers (83%) in 2014. In contrast, the use of real-time TD decreased from 24% in 2009 to 12% in 2014, while the use of hybrid systems fell from 9% to 5% over the same period (Fig. 2). In 2014, most centers used mid-range bridge cameras, 15% used teledermoscopy, and only 12% used mobile devices.
Comparison of 2009 and 2014 Survey Findings.
| Overall Comparison | 2009 | 2014 | Variation | |
|---|---|---|---|---|
| Centers using TD | 25 | 70 | Increase | |
| Departments that completed the survey | 21 | 42 | Increase | |
| Experience with TD (mean and range in years) | 3.1 (0.2-14) | 4.9 (0.5-17) | Increase | |
| TD modality | Store-and-forward | 67% (14/21) | 83% (35/42) | Increase |
| Real-time | 23% (5/21) | 12% (5/42) | Decrease | |
| Hybrid | 9% (2/21) | 4.5% (2/42) | Decrease | |
| Skin diseases assessed by TD | All types | 62% (13/21) | 81% (34/42) | Increase |
| Cancer only | 33% (7/21) | 16,6% (7/42) | Decrease | |
| Other | 4.7% (1/21) | 2.4% (1/42) | Similar | |
| Hours per week spent on TD (mean and range) | 3 (1-12) | 4.67 (0.5-18) | Increase | |
| Number of dermatologists practicing TD in each department (mean and range) | 2.3 (1-6) | 2.8 (1-7) | Increase | |
| Greatest distance between center and TD patient | Less than 50 km | 28% (6/21) | 46% (17/37) | Increase |
| Between 50 and 100 km | 38% (8/21) | 43% (16/37) | Increase | |
| More than 100 km | 33% (7/21) | 11% (4/37) | Decrease | |
| TD software integrated into hospital information system | 33% (7/21) | 66% (28/42) | Increase | |
| Training objectives for primary care physicians (e-learning) | 61% (13/21) | 66% (28/42) | Similar | |
C. Technical aspects: Regarding software, at 60% of centers the dermatologists participated in the development of the software and data collection system. Obligatory elements were included in 70% of the information systems used for TD. At 66% of the centers, it was possible to export data for use outside the system. In contrast to the level of development observed in the data-management software used in TD, just 33% of centers used diagnostic coding in 2014. Only 19% of centers had integrated their TD system with the hospital information system and appointment system in 2009, but by 2014 this figure had risen to 64%. This large increase reflects the notable development of electronic health records in recent years. In 2014, the mean satisfaction with the computer system reported by dermatologists was 7.15 on a scale of 0 to 10.
D. Objectives of TD: In 2014, a majority of the centers (62%) used TD in the treatment of all types of skin conditions, while 25% used it only for skin cancer (down from 38% in 2009). In 2014, 40% of the centers were able to schedule surgical appointments directly, with no need for a presurgical clinical appointment. (The survey did not ask about this option in 2009.) Two thirds of the centers used TD in the training of primary care physicians. Training took place by teleconsultation at 33% of centers, in seminars and meetings in 17% of centers, and by both methods in 31% of centers. Sixty-six percent of the centers used TD for teaching in 2014 and a similar percentage was reported in 2009. In contrast, just 20% of the centers carried out patient satisfaction surveys.
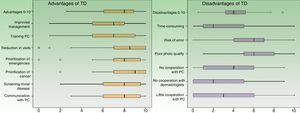
E. Advantages and disadvantages (Fig. 3): On a scale of 0 to 10, mean overall satisfaction with TD increased from 6.3 points in 2009 to 6.9 points in 2014. The main advantages and disadvantages of TD perceived by dermatologists were similar in 2009 and 2014. Among the main advantages were patient prioritization and communication with family doctors; in both surveys, poor photo quality was the main disadvantage reported. Internet connection speed was a problem for some centers in 2009, but not in 2014. The dermatologists assessed the various advantages and disadvantages on a scale of 0 to 10 in 2014; the results are shown in Fig. 3.
Advantages and disadvantages of using a TD system in 2014 (dermatologist's perspective on a scale of 0 to 10). The main advantages are scored on a scale of 0 (strongly disagree) to 10 (fully agree). The main disadvantages or problems are scored on a scale of 0 (nonexistent problem) to 10 (the problem is very serious and difficult to solve) (n = 42; ranges and medians). TD indicates teledermatology; PC, primary care.
As for overall trends, between 2009 and 2014 there was an increase in the number of centers using TD, the number of teledermatologists per center, the time spent on TD, the quality of technology and organization, the number of centers using store-and-forward TD systems, and the use of TD in urban settings (Table 1).
DiscussionThis study attempted to characterize the Spanish health care facilities that used TD in 2014 and to analyze changes and trends since 2009. Our findings show that TD is an emerging technology in Spain (Table 1). Between 2009 and 2014, the number of centers using TD in Spain practically tripled. Moreover, each center had more teledermatologists on staff, spent more time on TD, was better organized, and had better technology in 2014 than in 2009. There was also an incremental increase in the use of store-and-forward TD at the expense of real-time TD systems, as well as a trend towards more urban use of TD (in order words, the use of TD with patients who live closer the hospital).
Our study had some methodological limitations. The use of online surveys as a study method limited the response rate and left open the possibility of inaccurate responses. The initial methods of contacting the dermatologists were different in 2009 and 2014, so it is possible that undetected differences might exist. Some departments that actively use TD did not respond to the survey; this could be considered selection bias. Exhaustivity of access was the main advantage of our study, especially in 2014, when in-person access to 267 centers was achieved. Other strengths were the wealth and variety of the topics studied, as well as the high response rate among centers that use TD, both in 2009 and in 2014. These strengths suggest that the data obtained are representative and reliable.
Two longitudinal studies have analyzed the evolution of TD use in the United States.11,12 These studies found similar trends to those identified in Spain: an increase in TD use overall and in the use of store-and-forward models in particular. Although the number of TD programs in the United States fell from 62 in 2003 to 37 in 2011, the annual volume of consultations per center increased significantly, nearly doubling.11 Thus, one of the largest TD programs in the United States—that of the Veterans Health Administration (VHA)12—showed rapid growth in the number of TD consultations in recent years. As in Spain, TD in the United States has been shifting away from real-time methods (videoconference technology) since 2007, in favor of modalities involving the storage of still photographs.11,12 Nowadays, store-and-forward is the predominant TD technology, probably because of its low cost, higher image quality, and the fact that an asynchronous approach allows for better organization and greater efficiency.
Only 1 transversal study has offered a comprehensive, in-depth analysis of TD models over a large geographical area. In this study, Armstrong et al.10 studied TD in California—the most populous US state, with 38 million inhabitants—between 2007 and 2011. The authors identified just 17 teledermatologists working actively in 2011—a figure that stands in stark contrast to the 105 teledermatologists identified in 2014 in Spain, which has a population (46 million inhabitants) similar to that of California. The number of teledermatologists per million inhabitants was clearly lower in California (.44) than in Spain (2.28). In California, as in our study, the predominant TD model was store-and-forward (70%); however, hybrid systems were used by a larger percentage of teledermatologists in California (18%). As in Spain, the percentage of teledermatologists using only real-time TD was very low (6%). Mean experience with TD was similar in California and Spain (3.85 and 4.9 years, respectively). However, the objectives of TD use were different in Spain and California. In California, 75% of patients seen by TD had a low socioeconomic status and lived in remote rural areas. In contrast, most centers that used TD in Spain were concentrated in large cities (Seville, Madrid, and Barcelona) and this technology was used to see all types of patients. In their discussion section, Armstrong et al. describe TD as a rapidly evolving field but note that this technique should logically always serve as a complement to face-to-face options. The authors predict that future TD use will not be limited to rural communities or citizens at risk of exclusion. We agree with this view and our results support this theory; in Spain, the urban focus of TD is already a reality,13 as is the rapid development of TD in heavily populated areas of Europe such as the Netherlands and the United Kingdom. It is possible that the use of TD in the United States will begin to catch up with the European model. In fact, in the VHA program, patients seen by TD in urban areas have outnumbered patients in rural areas since 2012.12
The advantages described by Californian teledermatologists are similar to those reported by Spanish teledermatologists: greater efficiency, access, speed of care, and patient satisfaction. The main disadvantages were somewhat different; Californian dermatologists reported problems with reimbursement for teleconsultations as well as costly and inefficient software. In other areas, however, Californian and Spanish dermatologists voiced similar concerns. In both places, image quality and complex skin conditions were the main factors that limited the ability of TD to prevent face-to-face consultations. Moreover, on both sides of the Atlantic, dermatologists agreed that store-and-forward TD should not replace face-to-face consultations entirely. The option of face-to-face consultations should always exist, and for some conditions—for example, a patient with multiple pigmented lesions—face-to-face consultation is the only option and assessment by TD is contraindicated.3,8,13 Technological and legal considerations are also important barriers but can probably be overcome in the near future. According to the sample surveyed in our study, this trend towards future technological improvements appears to be evident. Potential improvements in the area of legal issues were not measured in the survey.
Despite these and other challenges in telemedicine, the development of TD appears to be unstoppable. In 2010, 38% of countries had some sort of TD program and 30% had governmental agencies dedicated to this practice.1 Multiple studies have provided evidence to support the reliability (agreement between diagnosis and management) and accuracy (validity compared to a gold standard) of TD.14 Store-and-forward TD has been shown to be effective in reducing the number of face-to-face consultations in hospitals.15 Face-to-face consultations and store-and-forward TD have shown similar results in terms of clinical improvement and time to intervention in patients with skin cancer.3,16 In recent years, there has been a considerable increase in the number of successful TD programs for managing skin cancer13 and for providing a rapid response in large urban areas.9 Patients have reported high satisfaction and a willingness to pay out of pocket to access TD services.17 TD has been shown to be cost-effective when used as a triage mechanism to reduce appointments and travel18 and to reduce the time to the initial intervention. TD is currently seen as a solution for many deficiencies in health systems.19–21 The technique can be used to increase accessibility for patients who live in remote areas or in geriatric facilities, prioritize cancer diagnosis, prevent referrals for trivial disease, and accelerate care in cases of emergency, among other benefits. The opinions of the Spanish dermatologists (n=42) who use and understand TD support these views (Fig. 3). Assessed on a scale of 0 to 10, the median score for advantages such as improved communication with primary care physicians, screening for trivial conditions, reduction in the number of face-to-face visits, and prioritization of conditions requiring urgent care and cancers was higher than 8. The main problems or disadvantages, also assessed on a scale of 0 to 10 (Fig. 3), received clearly lower scores (median score=4), with the exception of risk of error and poor photo quality (median score=6). Indeed, the reliability of TD is the parameter that has been most widely studied.14 The reliability of TD has been shown to be comparable to that of face-to-face consultation for diagnosis and management, although logically the photographs must be of sufficient quality in order for TD to achieve this reliability in diagnosis and management.
In our view, the main achievement of TD in Spain has been to improve the quality of health care processes, and this fact explains the considerable development of TD that has taken place in Spain.4 TD use has also increased in other developed countries, such as the United States and European countries.22–25 In the United States, TD use increased from 7% to 11% between 2012 and 2014.24 In the Netherlands, TD is fully reimbursed and integrated in the national health system.22 The use of TD is also on the rise in the United Kingdom, where resistance to this technique among dermatologists is decreasing.25 Developing countries, meanwhile, are probably just beginning to apply this technique. A recent study in South Africa found no evidence of the scaling of TD services or of the integration of TD into routine health care.26
Our study showed that the development of TD in Spain is considerable but that there is still much room for improvement, and that it is important not only to increase the number of TD programs but also to improve their quality. Health care providers must give dermatologists sufficient time for teleconsultations and adequate resources (software integrated with diagnostic coding, quality cameras and dermoscopes).
In conclusion, TD is an emerging technology that is becoming well established in Spain. In 2014, more than 25% of public dermatology centers in Spain had introduced a TD system. The levels of development and implementation of TD appear to be higher in Spain than in countries on the cutting edge of telemedicine such as the United States. The predominant model in Spain—store-and-forward TD in urban settings—is similar to that of the Netherlands, and the United States appears to be adopting this trend. In line with findings in other countries, Spanish dermatologists perceive TD as an effective option with more advantages than disadvantages. Dermatologists are generally highly satisfied with TD, although there are still areas in need of significant improvement.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We are grateful to the AbbVie sales network for collaborating on the distribution and collection of the surveys in 2014.
Please cite this article as: Romero G, de Argila D, Ferrandiz L, Sánchez MP, Vañó S, Taberner R, et al. Modelos de práctica de la teledermatología en España. Estudio longitudinal 2009-2014. Actas Dermosifiliogr. 2018;109:624–630.