A 39-year-old Moroccan man with no relevant past history consulted for assessment of diffuse, painful swelling of the right foot, accompanied by redness and small ulcers with secretion. The symptoms had first appeared 1 year earlier. The patient reported no trauma to the area and presented no other symptoms.
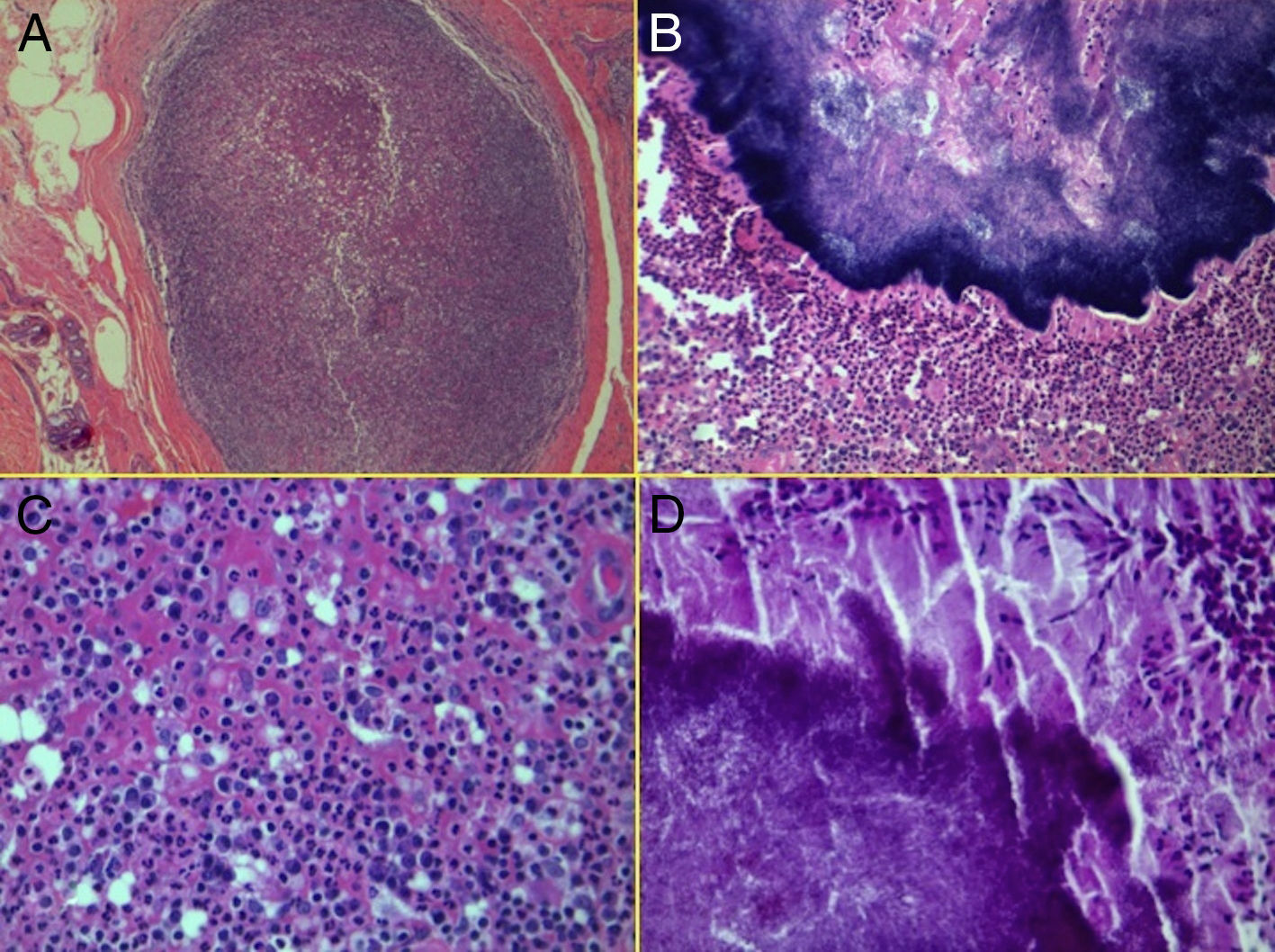
Physical ExaminationPhysical examination of the right foot revealed indurated, poorly defined nodules with purulent secretion (Fig. 1).
Additional TestsMagnetic resonance imaging revealed soft tissue involvement, fungoid masses, nodular lesions, and a lytic lesion in the first metatarsal.
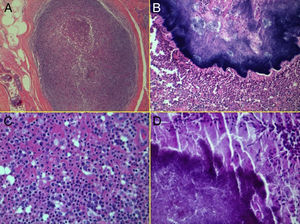
HistopathologyHistologic examination with hematoxylin-eosin staining revealed dermal abscesses surrounded by fibrous tissue (Fig. 2A). At higher magnification, structures formed by basophilic granulations surrounded by an eosinophilic hyaline material were observed inside the abscesses (Fig. 2B). Abundant polymorphonuclear neutrophils, plasma cells, histiocytes, and necrotic material were observed in the periphery (Fig. 2C). These structures were stained with the periodic acid–Schiff (PAS) technique.
What Is Your Diagnosis?
DiagnosisActinomycetoma of the foot.
Clinical Course and TreatmentFilamentous gram-positive bacteria consistent with Actinomyces species were observed in culture (Fig. 2).
The patient received 3 cycles of treatment, each administered 2 months apart, with intramuscular amikacin at a dose of 500mg/d for 21 days and treatment with trimethoprim/sulfamethoxazole at a dose of 2g/d for 6 months.
The symptoms recurred 6 months and 1 year later, and the patient received treatment with amikacin at the same dose as before. Clinical and microbiologic cure was achieved 1 year after treatment ended.
CommentMycetoma is a chronic suppurative infection caused by Actinomyces bacteria or eumycetes. Actinomycosis of the foot is caused by inoculation following trauma; it is most common in men between the ages of 30 and 50 years in barefoot-walking populations, agricultural workers, immunodeficient patients, and homeless persons.1
The prevalence of the disease has increased in Europe and the United States as a result of immigration and travel from endemic areas.2 Clinically, it is characterized by swelling, abscesses, fistulization, and secretion of discharge containing colored granules. The color of these granules can be the key to diagnosis. The techniques used to diagnose the disease also include imaging, cytology, histology, immunodiagnosis, and, most importantly, culture. DNA sequencing is useful in cases in which the culture is negative.3
The incubation period ranges from weeks to months. Initially asymptomatic, the disease progresses by infecting deep tissues, forming abscesses, fistulas, and pseudotumors.
The disease is usually diagnosed at advanced stages of progression. Actinomycetoma can progress rapidly and lead to risk of amputation, and it can even lead to death by means of systemic dissemination. However, actinomycetoma responds better to antibiotic treatment than eumycetoma does. Local complications can lead to extensive, disfiguring scars.4 Diagnosis requires a detailed medical history and physical examination. The color of the granules should raise the suspicion of actinomycetoma or eumycetoma.5
The differential diagnosis should include other local infectious processes such as botryomycosis as well as various tumors.6
Treatment is based on expert opinion—no evidence-based studies have been carried out—and lasts between 3 and 18 months. Surgery is necessary in many cases of eumycetoma.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr. Josep Arimany for allowing us to study and treat his patient.
Please cite this article as: Giavedoni P, Barreiro-Capurro A, Ferrando J. Tumoración mal delimitada de larga evolución en el pie de un inmigrante. Actas Dermosifiliogr. 2014;105:191–192.