Pilomatricoma is a benign neoplasm with differentiation into hair follicle matrix cells.1
Although it appears more frequently in individuals younger than 30 years,1 a 2nd incidence peak has been described between 50 and 65 years.2
Since most of the literature describes two peaks of higher incidence, the aim of this study is to conduct a comparative analysis of the characteristics of pilomatricomas based on the age of presentation.
Material and methodsWe conducted a retrospective review on 287 histologically confirmed cases of pilomatricomas from 1992 through 2023 in the South Health Area of Seville (Spain). Subsequently, we performed an analysis of their characteristics comparing three age groups (≤20, 21–59, and ≥60 years).
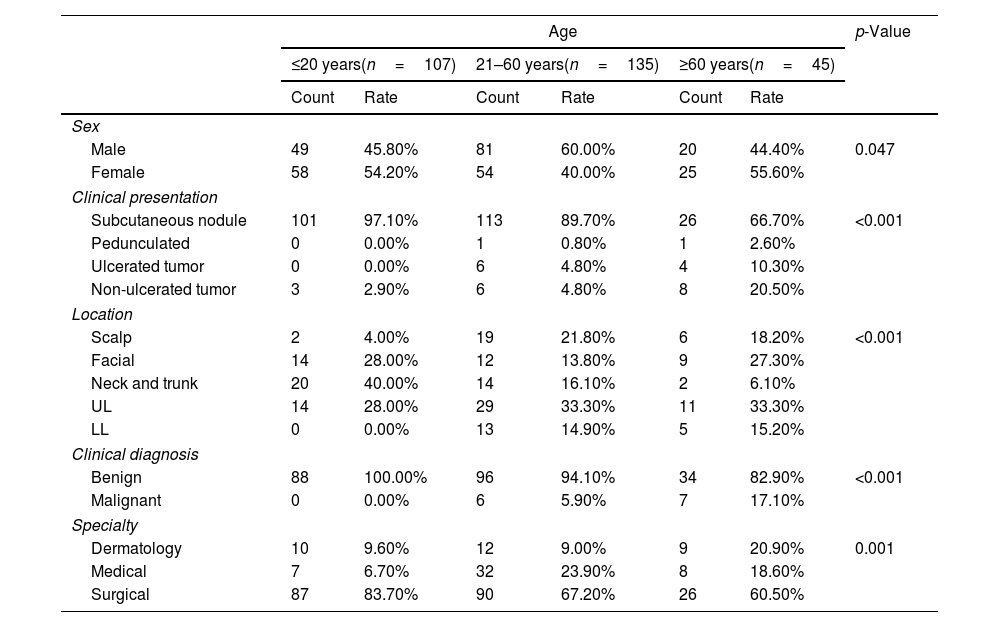
ResultsThe highest proportion of cases was found in individuals under 20 years old (37.3%), followed by those aged 40–64 years (31%). Men accounted for 52% of the cases. There was a predominance of men in the 21–59 age group and women in the other groups.
In all age ranges, the most common presentation of pilomatricoma was as a subcutaneous nodule. However, in individuals over 60 years old, there was a higher proportion of lesions presenting as tumors and ulcerations.
Lesions were most frequently located on the upper limbs, except in individuals under 20 years old, where they primarily appeared on the neck and trunk. In the 21–59 age group, pilomatricomas were more common on the scalp and lower limbs than in the other two groups.
Preoperative diagnosis was correct in only 2.5% of cases. Differential diagnosis included other benign tumors, with cysts being the most common, as well as malignant tumors.
In 100% of the younger patients, pilomatricoma was identified as a benign lesion. In contrast, in individuals over 60 years old, it was mistaken for a malignant tumor in 17.1% of cases.
Most cases were evaluated by general surgery (63.3%) and other surgical specialties. Middle-aged patients were more frequently assessed by medical specialties (primary care and internal medicine) vs the other groups. Only 11% of patients were evaluated by dermatology, with older patients being the most widely referred (Table 1).
Main study results.
| Age | p-Value | ||||||
|---|---|---|---|---|---|---|---|
| ≤20 years(n=107) | 21–60 years(n=135) | ≥60 years(n=45) | |||||
| Count | Rate | Count | Rate | Count | Rate | ||
| Sex | |||||||
| Male | 49 | 45.80% | 81 | 60.00% | 20 | 44.40% | 0.047 |
| Female | 58 | 54.20% | 54 | 40.00% | 25 | 55.60% | |
| Clinical presentation | |||||||
| Subcutaneous nodule | 101 | 97.10% | 113 | 89.70% | 26 | 66.70% | <0.001 |
| Pedunculated | 0 | 0.00% | 1 | 0.80% | 1 | 2.60% | |
| Ulcerated tumor | 0 | 0.00% | 6 | 4.80% | 4 | 10.30% | |
| Non-ulcerated tumor | 3 | 2.90% | 6 | 4.80% | 8 | 20.50% | |
| Location | |||||||
| Scalp | 2 | 4.00% | 19 | 21.80% | 6 | 18.20% | <0.001 |
| Facial | 14 | 28.00% | 12 | 13.80% | 9 | 27.30% | |
| Neck and trunk | 20 | 40.00% | 14 | 16.10% | 2 | 6.10% | |
| UL | 14 | 28.00% | 29 | 33.30% | 11 | 33.30% | |
| LL | 0 | 0.00% | 13 | 14.90% | 5 | 15.20% | |
| Clinical diagnosis | |||||||
| Benign | 88 | 100.00% | 96 | 94.10% | 34 | 82.90% | <0.001 |
| Malignant | 0 | 0.00% | 6 | 5.90% | 7 | 17.10% | |
| Specialty | |||||||
| Dermatology | 10 | 9.60% | 12 | 9.00% | 9 | 20.90% | 0.001 |
| Medical | 7 | 6.70% | 32 | 23.90% | 8 | 18.60% | |
| Surgical | 87 | 83.70% | 90 | 67.20% | 26 | 60.50% | |
LL, lower limbs; UL, upper limbs.
No statistically significant differences were found across age groups regarding lesion size (median=1.2cm), the presence of associated lesions (3.5% of cases, with cysts being the most frequent), or the existence of multiple lesions (3.5%).
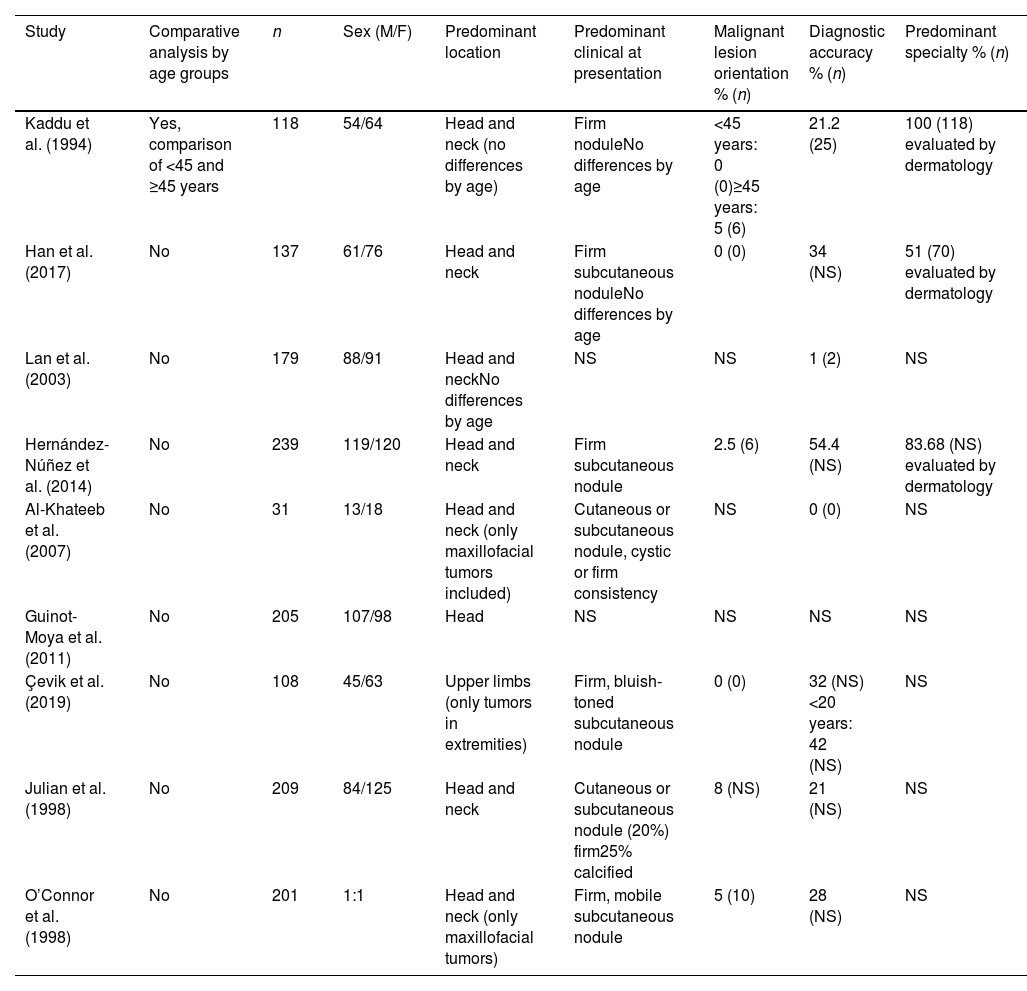
DiscussionOur study population exhibits a bimodal distribution, which is consistent with observations made by other researchers.1,3,4
There is a predominance of men, which is also similar to the findings made in the studies conducted by Lan et al.3 and Guinot-Moya et al.5
Based on our data, age influences the clinical appearance of the lesion, in contrast to the analysis by Kaddu et al.,1 which revealed no differences.
There is agreement between our series and other studies regarding lesion size and the proportion of patients with multiple tumors.3,5–8
In most of the literature, the head and neck are the most common locations,2–6,9 whereas in our series, the upper limb was the most frequent site. However, this is not directly comparable since we separated the head into “facial” and “scalp” regions and categorized cervical tumors together with those on the trunk.
Although it is rare to report the presence of associated lesions, in both the series by Hernández-Núñez et al.9 and ours, cysts were the most common findings (72.7%).
The accuracy of preoperative diagnostic is low,3,4,7 with only 6 cases being (2.5%) correctly identified. This low proportion contrasts with the figures presented by Hernández-Núñez et al. and Han et al. (54.4%9 and 34.5%,2 respectively). This discrepancy is likely due to the fact that most patients in those series were evaluated by dermatologists. We agree with Julian et al. that correct diagnoses are primarily made by dermatologists (5 cases),4 highlighting a lack of familiarity with this tumor among other professionals.
Cysts represent the primary differential diagnosis in both the literature reviewed2–4,6,9,10 and our study. In 5.6% of cases, the lesion was preoperatively considered malignant, a slightly lower rate than that reported by Julian et al.4 Similar to Kaddu et al., we observed that as age increases, the proportion of clinically diagnosed malignant lesions also rises (Table 2).1
Former studies on pilomatricoma and relevant findings for the present study.
| Study | Comparative analysis by age groups | n | Sex (M/F) | Predominant location | Predominant clinical at presentation | Malignant lesion orientation % (n) | Diagnostic accuracy % (n) | Predominant specialty % (n) |
|---|---|---|---|---|---|---|---|---|
| Kaddu et al. (1994) | Yes, comparison of <45 and ≥45 years | 118 | 54/64 | Head and neck (no differences by age) | Firm noduleNo differences by age | <45 years: 0 (0)≥45 years: 5 (6) | 21.2 (25) | 100 (118) evaluated by dermatology |
| Han et al. (2017) | No | 137 | 61/76 | Head and neck | Firm subcutaneous noduleNo differences by age | 0 (0) | 34 (NS) | 51 (70) evaluated by dermatology |
| Lan et al. (2003) | No | 179 | 88/91 | Head and neckNo differences by age | NS | NS | 1 (2) | NS |
| Hernández-Núñez et al. (2014) | No | 239 | 119/120 | Head and neck | Firm subcutaneous nodule | 2.5 (6) | 54.4 (NS) | 83.68 (NS) evaluated by dermatology |
| Al-Khateeb et al. (2007) | No | 31 | 13/18 | Head and neck (only maxillofacial tumors included) | Cutaneous or subcutaneous nodule, cystic or firm consistency | NS | 0 (0) | NS |
| Guinot-Moya et al. (2011) | No | 205 | 107/98 | Head | NS | NS | NS | NS |
| Çevik et al. (2019) | No | 108 | 45/63 | Upper limbs (only tumors in extremities) | Firm, bluish-toned subcutaneous nodule | 0 (0) | 32 (NS) <20 years: 42 (NS) | NS |
| Julian et al. (1998) | No | 209 | 84/125 | Head and neck | Cutaneous or subcutaneous nodule (20%) firm25% calcified | 8 (NS) | 21 (NS) | NS |
| O’Connor et al. (1998) | No | 201 | 1:1 | Head and neck (only maxillofacial tumors) | Firm, mobile subcutaneous nodule | 5 (10) | 28 (NS) | NS |
NS, not specified.
The present study includes one of the largest series to date and provides a more comprehensive comparative analysis based on age.
The limitations of this study include its retrospective design, leading to inconsistencies in data collection, and the categorization of lesion locations, which differs from previous studies, making comparisons difficult.
ConclusionsThe diagnosis of pilomatricoma is challenging for physicians, even for dermatology specialists. The age of presentation influences sex distribution, lesion location, clinical presentation, and diagnostic approach.
FundingNone declared.
Conflicts of interestNone declared.