A 72-year-old man with a history of alcohol use and stable chronic lymphocytic leukemia (CLL) not requiring treatment presented to dermatology with a 3-year history of lesions located on the nasal dorsum for evaluation. The patient had previously been diagnosed with rosacea and rhinophyma and had received topical and oral antibiotic therapy without improvement.
Physical examinationPhysical examination revealed evident swelling along with erythema and soft-tissue enlargement throughout the nasal dorsum, with marked induration on palpation (Fig. 1).
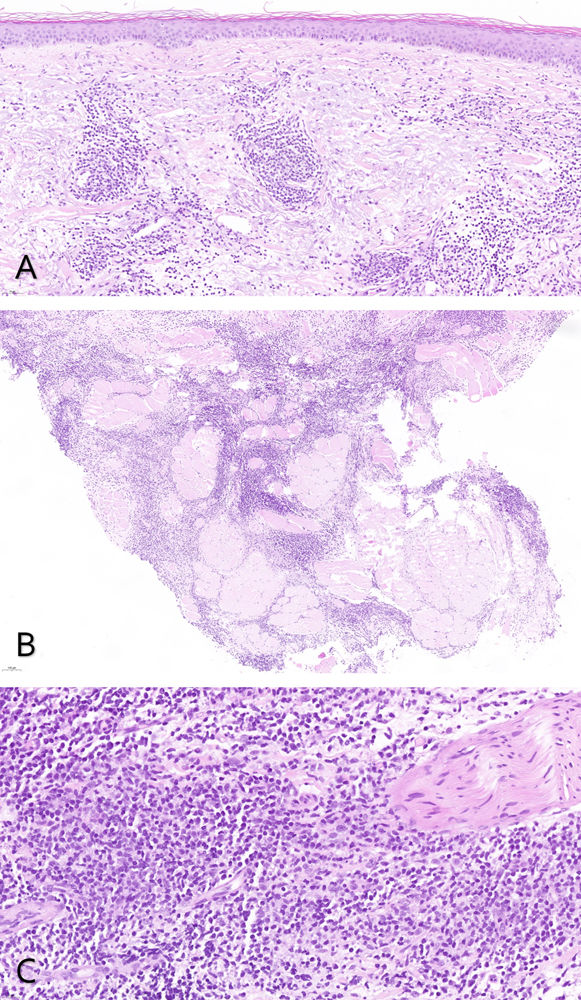
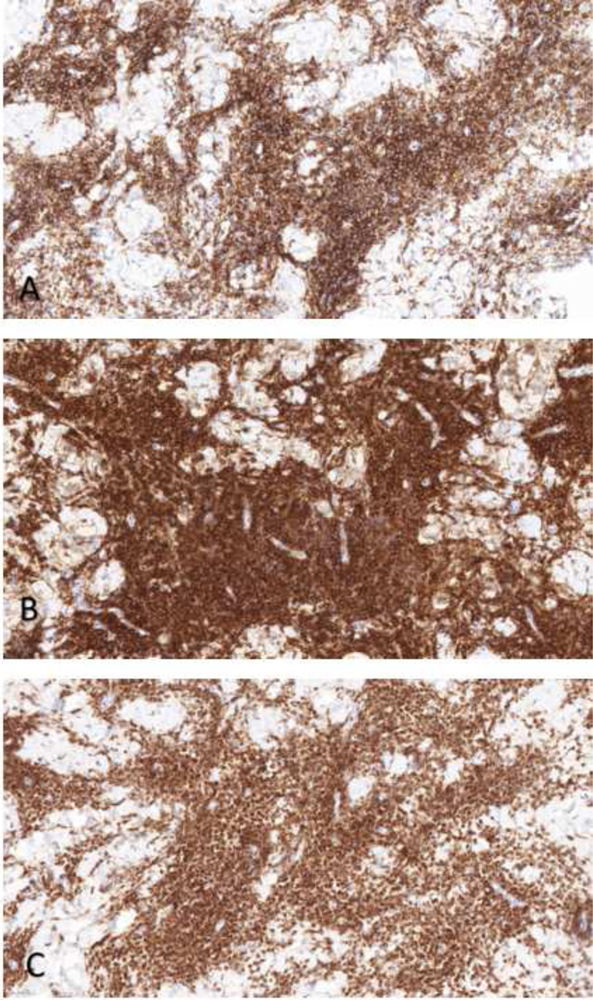
HistopathologyBiopsy showed an unremarkable epidermis and a lymphocytic infiltrate in the dermis composed of small lymphocytes with hyperchromatic nuclei and scant cytoplasm (Fig. 2). Immunohistochemistry demonstrated positivity for CD20, CD23, and BCL-2 (Fig. 3A–C).
What is your diagnosis?
DiagnosisCLL-induced cutaneous infiltration.
Course of the disease and treatmentGiven progression of the CLL, with progressive enlargement of cervical, axillary, and inguinal lymph nodes, the Hematology unit started ibrutinib therapy. The patient showed a good hematologic response, along with notable parallel improvement of the cutaneous lesions, with a marked reduction in nasal induration and erythema 1 month into therapy.
CommentCLL is the most common type of leukemia in adults and is characterized by the accumulation of monoclonal B lymphocytes in the blood, bone marrow, spleen, and lymph nodes. Cutaneous involvement can be observed in approximately 25% of cases, mainly as nonspecific signs, such as infectious complications, exaggerated reactions to insect bites, or vasculitis, among others.1 In addition, specific lesions due to cutaneous infiltration by tumor cells may occur, a condition known as leukemia cutis (LC).1
The leukemia subtype most frequently associated with LC is acute myeloid leukemia, especially monocytic and myelomonocytic variants. Clinically, LC typically presents as solitary or grouped papules, plaques, or nodules, often arising in areas of skin previously affected by herpetic lesions.1
Cases have been reported in the literature of LC presenting as rosacea-like eruptions.2–5 It has been proposed that the development of LC in the same location as prior rosacea lesions may represent a form of Wolf's isotopic response, similar to what occurs after prior varicella-zoster or herpes simplex infection.2 Chronic stimulation by Demodex folliculorum of skin-associated lymphoid tissue has also been suggested as a potential pathway leading to lymphoma development, analogous to the relationship between Helicobacter pylori and gastric MALT lymphoma.2,3
In our patient, the striking swelling confined exclusively to the nasal area and the absence of the sebaceous skin quality characteristic of rosacea prompted us to reconsider the diagnosis and perform a biopsy. Histology revealed the presence of a superficial and deep perivascular dermal lymphocytic infiltrate that may resemble the perivascular cuffing seen in tumid lupus.6 However, the absence of interstitial mucin deposition, the patient's hematologic history, and immunohistochemistry findings allowed us to reach the diagnosis of CLL-induced LC.
This case illustrates a very unusual clinical presentation of LC and underscores the importance of including this entity in the differential diagnosis of atypical rosacea-like lesions that are refractory to standard treatments.
Conflict of interestThe authors declare no conflict of interest.