Periorificial cutaneous tuberculosis, or tuberculosis cutis orificialis, accounts for approximately 2% of cases of tuberculosis of the skin.1 It results from the auto-inoculation of Mycobacterium tuberculosis into the periorificial oropharyngeal, anal, or genital skin or mucosa from a pulmonary, intestinal, or genitourinary focus, respectively.2,3 The definitive diagnosis is made by the isolation of M tuberculosis from the ulcer and detection of the focus of mycobacterial infection responsible for the disease.
The patient was a 78-year-old woman who was referred to our outpatient clinic for mild vulvar bleeding and a long-standing painful ulcer of the labia minora of the vulva. The patient had no other symptoms. Of note in her past medical history was a cadaveric orthotopic kidney transplant in 2005 for chronic kidney failure of unknown etiology. Since that time she had been on immunosuppressive treatment with oral corticosteroids, tacrolimus, and mycophenolate mofetil.
Physical examination revealed a very painful, irregular ulcer of 4×1.5cm on the left labium minus. The base of the ulcer was soft and erythematous and was covered with areas of adherent whitish pseudomembrane (Fig. 1). There were no palpable regional lymph nodes.
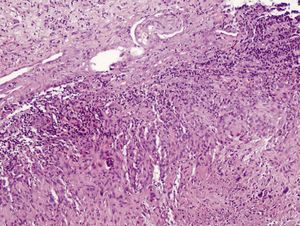
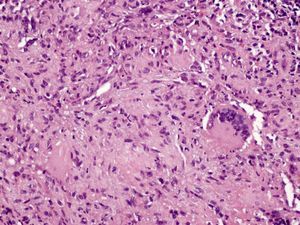
Skin biopsy showed a superficial material formed of fibrin and white blood cells and deeper in the tissue there were numerous granulomas (Fig. 2), some with a necrotic center of caseous appearance, epithelioid cells, and Langhans-type multinucleated giant cells (Fig. 3). No acid-alcohol-fast bacilli were observed with Ziehl-Neelsen stain. These findings were compatible with a diagnosis of ulceration with tuberculoid granulomas.
Given the presence of tuberculoid granulomas and ulceration, a request was made for screening for mycobacteria in the exudate from the ulcer and in the urine obtained by catheterization. Study of the exudate from the ulcer by polymerase chain reaction (PCR) was weakly positive. Ziehl-Neelsen stain of the sample taken from the skin was negative, but it was positive on the urine. Cultures of samples from both sites in Middlebrook 7H9 liquid medium were positive after an adequate incubation time. The microorganism isolated was identified as M tuberculosis using DNA hybridization probes.
The study was completed by hysteroscopy, chest x-ray, abdominal ultrasound, and abdominal computed tomography; there were no signs of active or residual tuberculosis. The tuberculin skin test was negative. Based on these results, a diagnosis was made of vulvar tuberculosis cutis orificialis secondary to auto-inoculation from a urinary focus.
The patient was immediately started on treatment with isoniazid at a dosage of 250mg/d, rifampicin, 600mg/d, pyrazinamide, 1500mg/d, and ethambutol, 800mg/d, which were continued for 2 months; she was subsequently treated for a further 4 months with only isoniazid and rifampicin. The clinical course was favorable with the treatment administered.
There is a high prevalence of tuberculosis in Spain (16.96 cases/100 000 population in 2009 according to the Spanish Network for Epidemiological Monitoring, and 30/100 000 population in 2007 according to the World Health Organization).4 The most common variant of cutaneous tuberculosis is lupus vulgaris.5 Tuberculosis cutis orificialis is a rare variant and accounts for only 2% of cases of cutaneous tuberculosis. It occurs mainly in immunosuppressed individuals,1 and the majority of patients are middle-aged men.6
This clinical form affects the oral, perianal, or genital mucosas and the periorificial skin after auto-inoculation of the bacillus, which is derived from a pulmonary, intestinal, or genitourinary focus by direct spread. The lesions mainly occur in traumatized areas. Lymphocytic or hematogenous dissemination and the involvement of adjacent organs is rare.2,3 The disease is defined clinically by yellowish papules or nodules that rapidly ulcerate, giving rise to very painful, punched-out ulcers with a granular base covered by a whitish pseudomembranous material. Histology of the lesions will show tuberculoid granulomas. Culture and the tuberculin skin test are usually positive.7
Untreated, the disease can be fatal within a few months, due to miliary dissemination of the bacillus.3
The diagnosis of tuberculosis cutis orificialis requires the correlation of clinical, histopathological, and microbiological findings. Conventional mycobacterial culture continues to be the most reliable method for confirming the presence of mycobacteria and their antibiotic sensitivity, as well as for monitoring treatment; however, it has the disadvantage of a long delay until the results are available.8 PCR testing is a powerful tool for the diagnosis of cutaneous tuberculosis, as it is rapid, reliable, and very sensitive.9
The differential diagnosis of ulcerated genitourinary lesions similar to those presented includes Lipschütz ulcer, herpes simplex, tumors, pyoderma gangrenosum, sarcoidosis, chancroid, syphilis, lymphogranuloma venereum, tuberculosis, leishmaniasis, and the deep mycoses.3,10
Cutaneous tuberculosis, including the periorificial form, is treated using the standard treatment regimens for pulmonary tuberculosis.7,8
We would like to thank Dr José Luis Parra Martínez for his accurate initial diagnosis made at his private pathology laboratory, and for supplying us with the fixed histological specimen to complete the study.
Please cite this article as: Jiménez-Gallo D, et al. Tuberculosis cutánea periorificial vulvar. Actas Dermosifiliogr. 2012;103;929–30.