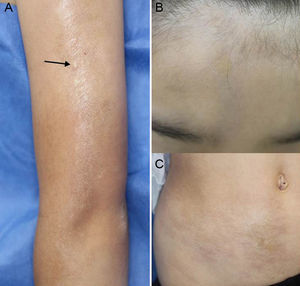
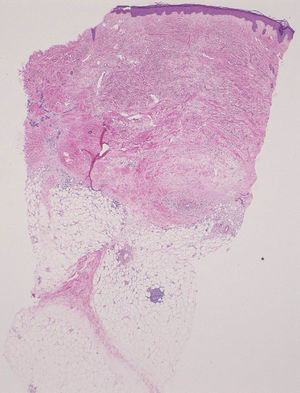
An 8-year-old girl was referred to our department with a linear sclerotic lesion on the upper left arm that had appeared several months earlier. The lesion had developed on the upper lateral aspect of the left arm, at the site of a Bacille Calmette-Guerin (BCG) vaccine, given more than 7 years earlier. It had gradually spread in a linear pattern and new sclerotic plaques appeared in increasing numbers over the subsequent months. Physical examination revealed a linear, slightly sclerotic plaque on the forehead (scleroderma en coup de sabre), linear pigmented, shiny plaques on the upper left arm, and sclerotic plaques on the right abdomen, left axilla, and back (Fig. 1A–C). The girl also complained of muscle weakness in the upper left arm and occasional headaches. A biopsy specimen taken from the BCG vaccination site revealed thickened collagen bundles throughout the dermis (Fig. 2). Patchy lymphocytic infiltrates and fibrosis of septal connective tissues were seen in the subcutaneous tissue. Laboratory tests revealed positive antinuclear antibodies (1:320, speckled and nucleolar) and values within the normal range for rheumatoid factor and anti-DNA, anti-centromere, and anti-U1RNP antibodies. Liver and kidney function, serum complement levels, creatine phosphokinase, aldolase, and myoglobin were also all within normal ranges. Three-dimensional computed tomography of the scalp did not reveal any abnormal findings. The patient was initially treated with oral prednisolone (15mg/d), followed by the addition of methotrexate (6mg/wk), which led to satisfactory results.
Morphea is sometimes triggered by local stimuli, such as minor trauma, irradiation, vaccination, implantation of silicon prostheses, needle biopsy, laparoscopy, and drug injections; it can also arise at the site of surgical and herpes zoster scars.1–7 The Koebner phenomenon is seen in various disorders, including morphea. The pathogenesis of this phenomenon has not yet been fully elucidated. Upon epidermal injury, several proinflammatory cytokines, such as interleukin 1, tumor necrosis factor α, and granulocyte macrophage-colony stimulating factor (GM-CSF), are released, possibly inducing further inflammation. Ueki8 proposed a 2-step theory to explain the pathophysiology of the Koebner phenomenon. The first step, referred to as a nonspecific inflammatory step, would involve multiple environmentally induced factors such as cytokines, stress proteins, adhesion molecules, and autoantigens translocated from intracellular areas, while the second, disease-specific, step would involve disease-specific reactions mediated by T cells, B cells, autoantibodies, and immune complex deposition under the restriction of susceptible backgrounds.
Dermatological complications of BCG vaccination generally include induration and severe ulceration, but cases of granuloma annulare, abscesses, papular tuberculids, lupus vulgaris, and benign and malignant tumors have also been reported. Keloid formation at the BCG vaccination site is well known, but few cases of morphea have been reported to date.9,10 In one of the cases, the lesions appeared on the shoulder a year after BCG vaccination, which was proposed as a possible trigger for the skin changes.9 Another case was reported in a series of 7 cases of sclerodermatous conditions after bone marrow transplantation, but a detailed description was not provided.10 Our patient developed linear scleroderma that started at the site of a BCG scar, without prior keloid scarring. Previous trauma may be associated with persistent inflammation and the release of various mediators such as cytokines and growth factors, or neurotransmitters from degenerative peripheral nerves.