Atopic dermatitis is a chronic inflammatory skin disease that is very common in childhood. Among adults it is an increasingly common reason for consultation and is diagnosed with increasing frequency. Dupilumab is a monoclonal antibody that blocks the interleukin 4 (IL-4) receptor subunit α, decreasing activation of cells that express this receptor (mainly Th2 lymphocytes). The decreased polarization of naïve Th to Th2 lymphocytes results in a decrease in the secretion and function of the cytokines IL-4, IL-13, and IL-5. Naive Th lymphocytes are instead polarized to Th1 and Th17 lymphocytes, increasing the secretion of the corresponding cytokines.
Therapeutic blockade of certain cytokines or their receptors causes certain immunological modifications. Beneficial effects have been described for several such therapies, mainly in patients with psoriasis, although paradoxical reactions occur in some patients.
The persistence or de novo appearance of head and neck dermatitis, which is observed in up to 10% of the cases in clinical practice,1 was not reported in the phase 3 clinical trial of dupilumab. Zhu et al.2 reported the appearance or persistence of facial dermatitis in 14 patients treated with dupilumab. In their study of 1000 patients with atopic dermatitis who were treated with dupilumab, Soria et al.3 found that this biological treatment resulted in the appearance of de novo head and neck dermatitis in 10 patients, and aggravation of the same presentation in 32, requiring discontinuation of dupilumab treatment in some cases.
Given these findings, it is important to consider the possibility of dermatosis of the head and neck in dupilumab-treated patients. This requires knowledge of the peculiarities of the corresponding lesions in affected patients.
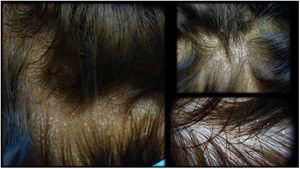
Malassezia hypersensitivity4 is proposed as the main reason for the de novo appearance or exacerbation of facial dermatitis. Pityriasiform lesions on the scalp (Fig. 1), whether associated or not with localized facial lesions in seborrheic areas, are indicative of seborrheic dermatitis. Detection of specific immunoglobulin (Ig) E against Malassezia species and a culture positive for this fungus can help orient the diagnosis. The underlying etiology is not well defined. Studies, including that of Adalsteinsson et al.,5 have proposed that Th2 lymphocytes are the main adaptive immune system cells responsible for regulating interactions with this commensal fungus. An adequate therapeutic response to oral or topical antifungals has been described in these cases.
Rosacea is another dermatosis that appears to play a key role in head and neck dermatitis in dupilumab-treated patients. Of 94 patients treated with dupilumab, 6.4% showed histologically confirmed inflammatory rosacea with an increase in colonization by the parasite Demodex.6 The proliferation of Demodex after polarization to Th1 and Th17 is proposed as trigger for rosacea. Although flushing episodes were observed in these patients, the main clinical manifestation appears to be basal erythema with inflammatory papules located mainly in the malar area. Histology reveals the abundant presence of Demodex folliculorum, although an adhesive tape test can demonstrate the presence of this parasite less invasively. It is important to remember the utility of the dermoscopy for the detection of Demodex species.7 Topical ivermectin or oral tetracyclines are the treatments of choice in these cases.
The persistence or de novo appearance of eyelid dermatitis may pose the greatest diagnostic and therapeutic challenge in clinical practice. In such cases, it will be necessary to rule out the presence of allergic contact dermatitis (ACD). The main culprits are fragrances and preservatives, although others, such as surfactants (e.g. cocamidopropyl betaine, derived from coconut), are common components of hair cosmetics. Both Raffi et al.8 and Zhu et al.9 reported no interference of continuous dupilumab treatment with patch testing. Another potential cause is ACD resulting from contact between the hands and face. In such cases, acrylates are one of the main allergens responsible, especially in women.
Sensitization to pneumoallergens is another potential cause in patients who show a seasonal worsening of head and neck dermatitis. Detection of specific IgE and collaboration with an allergologist is essential to confirm this etiology. Despite antihistamine treatment, skin lesions in these patients do not usually improve, necessitating specific recommendations on environmental exposure and the use of topical calcineurin inhibitors for the period during which the individual is exposed to pneumoallergens.
Obviously, there will be complex cases in which the cause of head and neck dermatitis in a given patient will not be clear. A growing body of evidence on this topic will help further our knowledge. However, the persistence or de novo appearance of head and neck dermatitis in patients taking dupilumab should not be a reason for treatment discontinuation. Clinical peculiarities may aid the dermatologist in selecting the most appropriate adjuvant treatment for each patient. Table 1 shows the clinical characteristics, corresponding additional tests, and recommended treatments in dupilumab-treated patients with head and neck dermatitis.
Possible etiologies of head and neck dermatitis in dupilumab-treated patients.
| Bacterial | Clinical manifestations | Complementary test | Treatment |
|---|---|---|---|
| Seborrheic dermatitis | Pityriasiform lesions (dry whitish scales) over orange erythema in seborrheic areas and on the scalp | Microbiological cultureMalassezia IgEMalassezia spp. prick testSkin biopsy | Oral antifungalsFluconazole 150mg/wk, 2 dosesItraconazole 50–100mg/d, 7–14 daysTopical antifungalsClotrimazoleFenticonazoleKetoconazole |
| Rosacea | Flushing (less frequent)Malar erythemaErythematous papulesPustules | Punch biopsyIn vivo study with adhesive test | Topical ivermectin 1%Oral doxycyclineOral isotretinoin |
| Allergic contact dermatitis | Localized eczema on the eyelids and hairline | Patch testsStandard seriesFragrance seriesCosmetic seriesOwn cosmetics | Avoid allergenHigh-potency topical corticosteroidsTopical calcineurin inhibitors |
| Airborne dermatitis | Facial eczema with involvement of skinfolds such as the eyelids and the retroauricular area | Specific IgE against pneumoallergensSpecific prick tests | Oral antihistaminesHigh-potency topical corticosteroidsTopical calcineurin inhibitors |