A 59-year-old homeless male patient presented to the emergency department with a 3-month history of a rapidly enlarging, painful perianal mass associated with rectal bleeding. He also reported nocturnal sweats, fever, weight loss, and a chronic productive cough. The patient had no past medical history of note and was not on any medication, but he was a smoker and consumed marihuana on a daily basis. He stated that he had unprotected sex with occasional women, but denied anal sex.
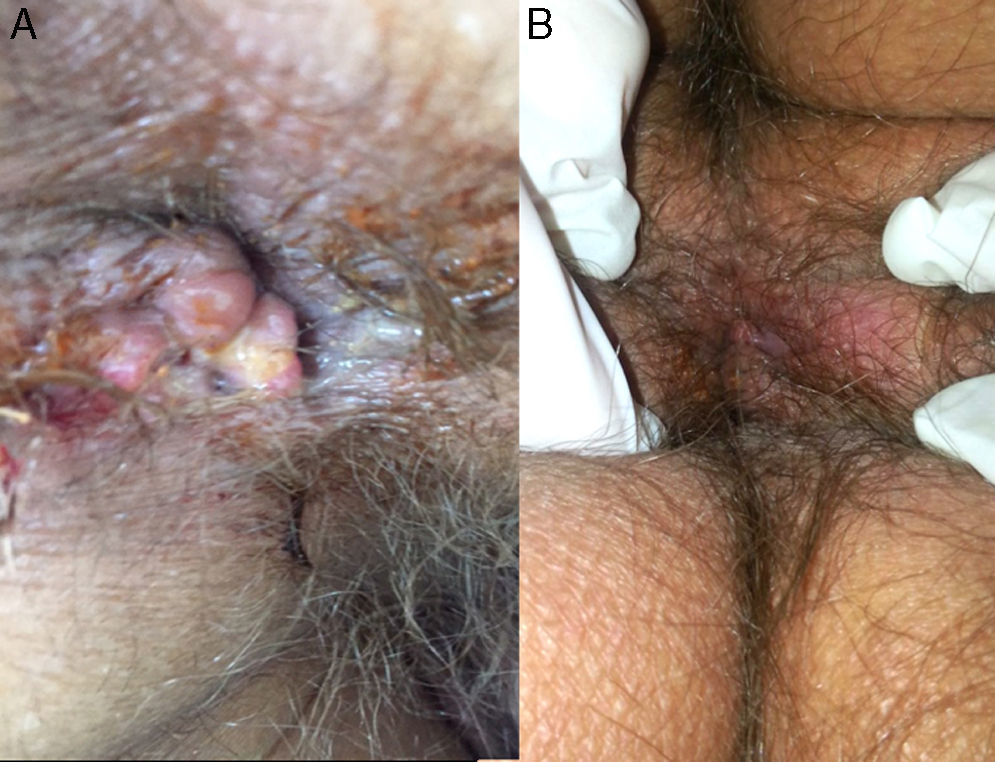
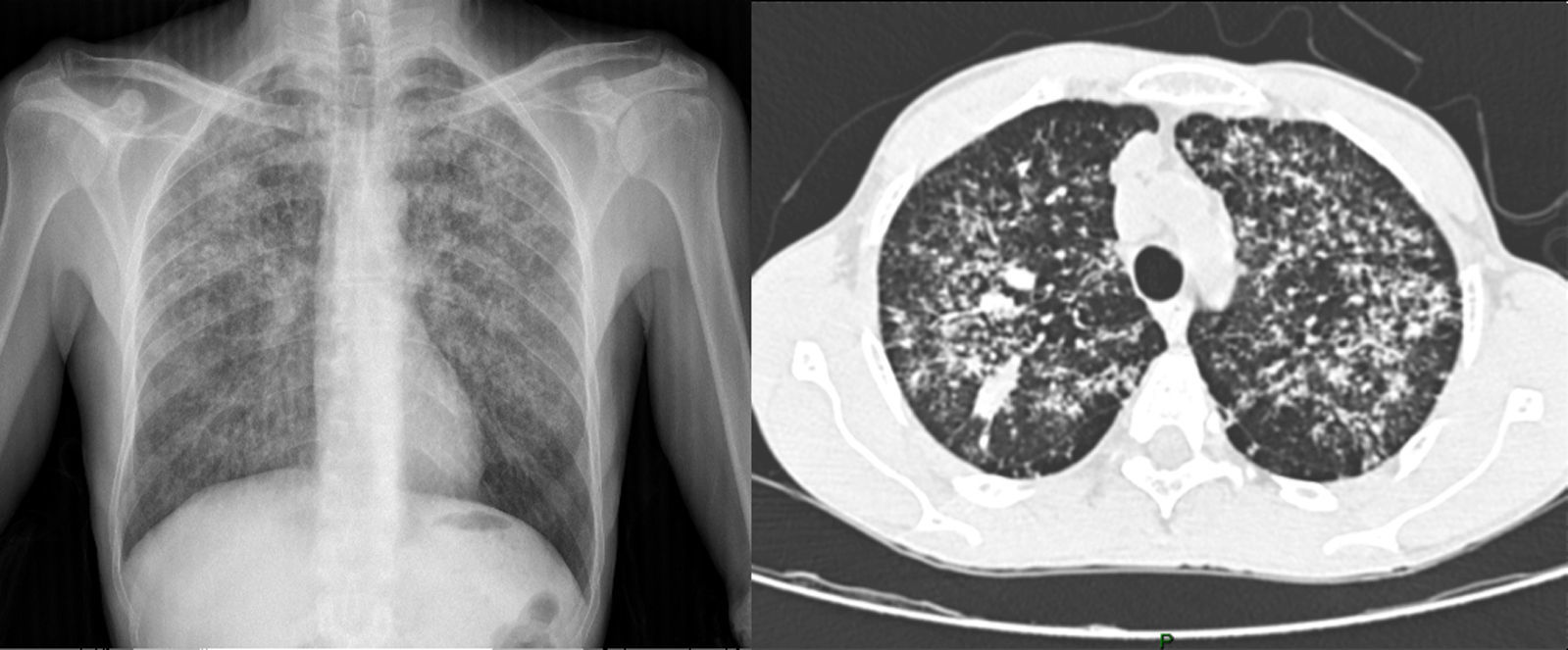
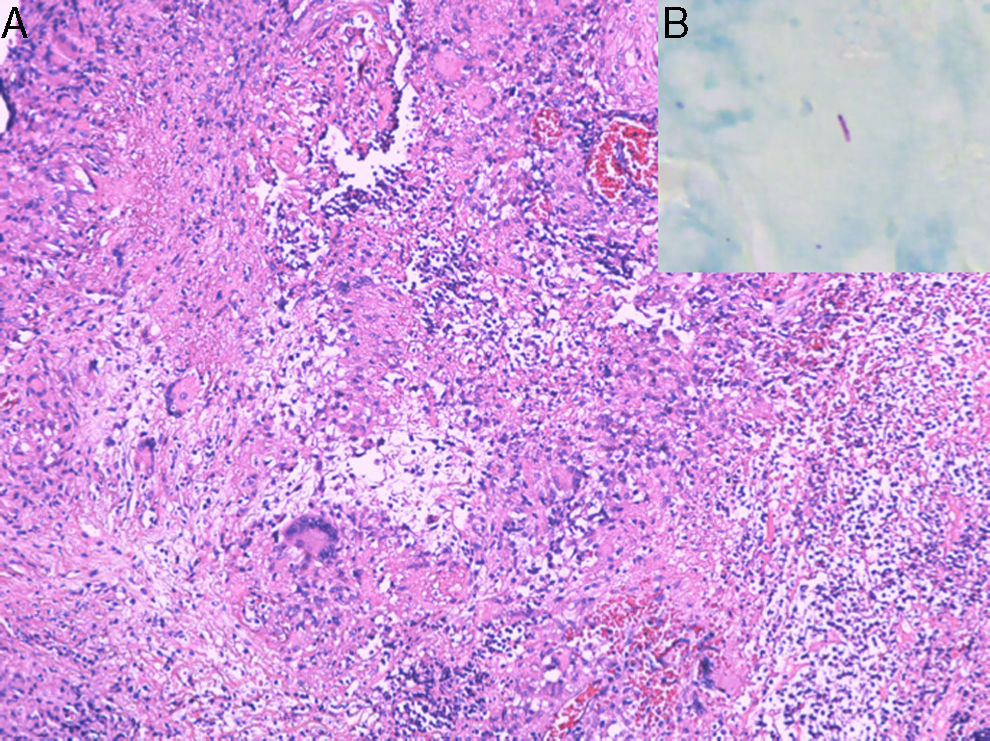
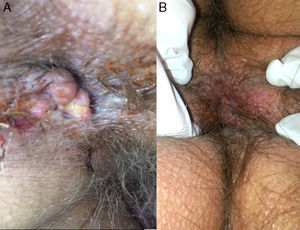
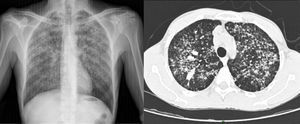
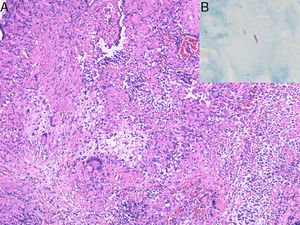
On inspection, the patient was cachectic, with a weight of 45kg. Physical examination revealed numerous enlarged cervical lymph nodes, some measuring over a centimeter in diameter, and chest auscultation was abnormal. In the perianal area, multiple skin-colored nodules had coalesced into a larger mass associated with a well-defined, indurated, painful, hemorrhagic perianal ulcer (Fig. 1). Serology for HIV and hepatitis was negative, and kidney and liver function was normal. Chest X-ray and high-resolution computed tomography revealed widespread reticulonodular opacities in both lung fields (Fig. 2). Sputum bacilloscopy was positive for acid-alcohol-fast bacilli, confirming the diagnosis of active pulmonary tuberculosis. The GeneXpert MTB/RIF test on material from a biopsy of a cervical lymph node was positive for Mycobacterium tuberculosis DNA. On colonoscopy an isolated ulcer with positive bacilloscopy for acid-alcohol-fast bacilli was discovered in the cecum. Biopsy of the perianal lesion reveled caseous necrosis and a granulomatous inflammatory process with positive bacilloscopy for acid-alcohol-fast bacilli and a GeneXpert MTB/RIF test that was positive for M. tuberculosis DNA, with a negative rifampicin resistance test (Fig. 3). Based on this information we made a diagnosis of disseminated tuberculosis (TB) with pulmonary, lymph node, intestinal, and perianal involvement. The patient started treatment with rifampicin, isoniazid, pyrazinamide, and ethambutol daily for 2 months, followed by rifampicin and isoniazid 3 times a week for 7 months (total treatment duration, 9 months). A good response was achieved after completing the first phase, with a decrease in the size of the perianal lesion (Fig. 1) and resolution of the systemic symptoms.
M. tuberculosis is an aerobic gram-positive bacillus that is a member of mycobacterium tuberculosis complex. Approximately 2 billion people, a third of the world's population, are infected by M. tuberculosis. Nine million new cases of active TB occur worldwide each year, leading to about 1.8 million deaths annually. The global incidence increased up to the year 2003, since which time there has been a slight fall. The incidence in Colombia is 25–35 cases per 100,000 people, this corresponds to a intermediate incidence in comparison to African countries, where 100–300 cases per 100,000 have been reported.1
Extrapulmonary TB occurs in 15% of cases and can be the result of primary or reactivated TB. The organs the most commonly affected are the lymph nodes (40%), pleura (20%), urinary tract (15%), bone (10%), central nervous system (5%), and heart (3%). Multiple risk factors have been established for primary and disseminated TB, the most important of which are HIV infection (relative risk [RR], 30), hemodialysis (RR, 20), transplant (RR, 20), intravenous drugs abuse (RR, 20), and infection in the previous year (RR, 13).2 A study on mortality in TB patients in Medellin, Colombia, detected social risk factors such as homelessness, drug addiction, or having no fixed address, in 58.1%.3
Gastrointestinal tract and skin involvement are very rare and have been reported in less than 1% of cases of extrapulmonary TB. Gastrointestinal TB can affect any organ of the digestive tract, but peritonitis is the most common presentation. When the intestine is compromised the infection is localized at the ileocecal valve in 85% of cases.4 Anal TB is a very rare condition, occurring in less than 1% of intestinal TB and in less than 0.0015% of all cases of TB. In 2008, Mathew et al.5 described the case of an 80-year-old patient with anal TB and reported that only 3 cases have been published in the United Kingdom. Perianal TB is categorized as periorificial cutaneous tuberculosis or tuberculosis cutis orificialis. It accounts for approximately 2% of cases of cutaneous TB. Tuberculosis cutis orificialis results from self-inoculation of M. tuberculosis into the periorificial oropharyngeal, anal, or genital mucosa from an initial pulmonary, intestinal, or genitourinary infection. Bacilli may reach the perianal area by hematogenous dissemination or by swallowing infected sputum. Numerous forms of anal TB have been described. The most common presentation is as an ulcerated lesion; fissures, verrucous forms, and masses have been reported in fewer cases. In 2009, Antonello et al.6 described the case of a 40-year-old HIV-positive patient with perianal TB that presented as an ulcerating mass, a compound lesion very similar to the finding in our patient. The patient presented by Cheon et al.7 in 2013 was a 46 year-old man diagnosed with Crohn disease 30 years earlier and treated with mesalazine with no improvement of his rectal ulcers. Anal TB was diagnosed and the patient presented a marked improvement after 3 months of treatment. Another case of anal TB was reported in a 42-year-old patient on Adalimumab therapy for psoriatic arthritis.8
The treatment of anal TB is the same as for other forms of extrapulmonary TB. Patients should receive rifampicin, isoniazid, pyrazinamide, and ethambutol daily for 2 months, followed by rifampicin and isoniazid 3 times a week for 7 months (total treatment time, 9 months).9 In order to prevent the appearance of active tuberculosis, the Centers for Disease Control and Prevention advocates targeted screening and treatment of latent tuberculosis infection with 9 months of isoniazid. A newer regimen of weekly combined therapy with isoniazid and rifapentine for 12 weeks was cost-effective in directly observed therapy programs, particularly for populations that would not otherwise complete therapy and are at high risk for conversion to active disease, such as homeless patients.10
Conflict of interestsThe authors declare no conflict of interest.