Chronic hepatitis caused by the hepatitis C virus (HCV) is associated with skin diseases including lichen planus, mixed cryoglobulinemia, porphyria cutanea tarda, pruritus, and necrolytic acral erythema. Cutaneous adverse effects are also common in patients treated with interferon (IFN), particularly when combined with ribavirin. These include injection-site reactions, alopecia, xerosis, pruritus, nummular eczema, lichen planus, and psoriasis flares.1
Sarcoidosis is a chronic systemic granulomatous disease of possible autoimmune etiology that primarily affects the lungs and lymph nodes. Induction of sarcoidosis, especially pulmonary and cutaneous forms, has been described in HCV patients treated with IFN alfa and ribavirin. It is thought that IFN alfa favors the differentiation of CD4 T cells, promoting a Th1-type immune response with subsequent granuloma formation. This mechanism may be intensified by ribavirin.2
We present the case of an adult woman with chronic hepatitis due to HCV who was treated with telaprevir, IFN alfa, and ribavirin and who developed papular sarcoidosis of the knees.
The patient was a 51-year-old woman with Child class A liver cirrhosis due to HCV genotype 1A, for which she had begun antiviral therapy 6 months earlier with telaprevir, IFN alfa, and ribavirin. She was seen for asymptomatic lesions on the knees that had appeared several months earlier.
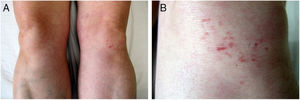
Physical examination revealed multiple brownish erythematous papules (2–5 mm in diameter), some of which were oriented linearly, on both knees (Fig. 1). Dermoscopy revealed an area of homogeneous yellow-orange coloration in which linear vessels were evident (Fig. 2).
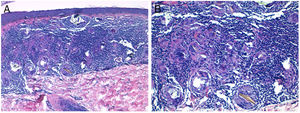
Histology of one of the lesions on the left knee revealed a non-necrotizing granulomatous infiltrate in the superficial dermis consisting of epithelioid histiocytes and multinucleated giant cells that phagocytosed birefringent crystalline material under polarized light microscopy (Fig. 3). A diagnosis of papular sarcoidosis of the knees induced by antiviral therapy was established.
Histological images. A, Non-necrotizing granulomatous infiltrate in the superficial dermis (hematoxylin-eosin, original magnification ×10). B, Epithelioid histiocytes and birefringent crystalline material phagocytosed by multinucleated giant cells (hematoxylin-eosin, original magnification ×20).
Additional tests (laboratory tests with complete blood count, biochemistry, serum levels of angiotensin-converting enzyme, calcium levels in urine collected over 24 h, tuberculin test, and chest x-ray) revealed no findings of note. Thoracic computed tomography (CT) revealed minimal involvement of the parenchyma of the peribronchovascular interstitium in the patient’s sarcoidosis. The skin lesions on the knees improved a few months after discontinuing antiviral therapy, without the need for treatment.
The prevalence of sarcoidosis is higher in HCV patients (0.12%) than in the general population (1–40 per 100000). Moreover, skin lesions are more common in sarcoidosis patients with HCV (56%) than in those without (22%).3 In many patients with chronic HCV hepatitis sarcoidosis is triggered by antiviral treatment (IFN alfa administered alone or in combination with ribavirin). The resulting sarcoidosis is usually pulmonary or cutaneous, and has a favorable prognosis. In fact, with adequate follow-up most patients can complete antiviral treatment. Once treatment is discontinued or completed the sarcoidosis lesions tend to resolve spontaneously,4,5 as observed for the cutaneous and pulmonary lesions in our patient.
Papular sarcoidosis of the knees is considered an intermediate clinical form of sarcoidosis, sharing features of scar and papular sarcoidosis.6 It is usually the initial manifestation of systemic sarcoidosis and has a good prognosis. It is characterized by the presence of reddish-brown papular lesions on both knees, in some cases with a lichenoid appearance and linear orientation.7,8 In approximately half of all cases papular sarcoidosis is associated with erythema nodosum (Löfgren syndrome). For many authors, the presence of these lesions on the knees is key for confirmation of sarcoidosis as the underlying cause of erythema nodosum.9,10 Papular sarcoidosis lesions on the knees usually resolve spontaneously. Even in the context of systemic sarcoidosis oral corticosteroid treatment is rarely necessary.10
Foreign-body particles are present in the lesions in 60% of cases of papular sarcoidosis. The linear distribution of some lesions is suggestive of an exogenous cause. However, patients tend not to report the presence of previous scars in the same location and histology reveals no scar tissue.10 It is possible that microtrauma results in the inclusion of foreign bodies, and that lesions develop years later in predisposed individuals or in response to treatments such as IFN alfa.5
The main differential diagnosis is scar sarcoidosis, a rare clinical form characterized by swelling and reddening of pre-existing scars of many types, including those caused by trauma, tattoos, venipuncture, surgery, hyaluronic acid injection, and burns.5
In conclusion, we describe a case of papular sarcoidosis of the knees in a HCV patient treated with telaprevir, IFN alfa, and ribavirin. Sarcoidosis should be suspected in patients with erythematous, occasionally linear papules located on both knees, especially in patients with erythema nodosum or HCV treated with IFN.
Please cite this article as: Monteagudo B, Grueiro MC, Vilas-Sueiro A, Campo-Cerecedo F. Sarcoidosis papulosa de las rodillas tras tratamiento con interferón alfa y ribavirina en paciente con hepatitis C. Actas Dermosifiliogr. 2019;110:871–873.