Giant basal cell carcinoma (BCC) is defined as a tumor with a diameter of 5cm or more. Surgery, the treatment of choice for any type of BCC, can cause considerable anatomical damage in large tumors. In 2 patients with giant BCC we therefore provided neoadjuvant treatment with a combination of oral acitretin and topical 5% imiquimod. Acitretin is a systemic retinoid used for primary prevention of nonmelanoma skin cancer. Imiquimod is an immunomodulator whose approved indications include treatment of nonfacial superficial BCC less than 2cm in diameter. Previous studies have demonstrated a synergic anticancer effect of both drugs in vitro and in vivo. This combination produced a marked reduction in tumor mass in our patients. Later we were able to provide definitive treatment, which achieved complete remission of the tumors.
El carcinoma basocelular (CBC) gigante se define como aquel que mide 5cm o más. Aunque la cirugía se considera el tratamiento de elección para cualquier tipo de CBC, en los de gran tamaño, puede ser altamente destructiva. Así, utilizamos la combinación de acitretino oral e imiquimod 5% tópico como tratamiento neoadyuvante en dos pacientes afectos de un CBC gigante. El acitretino es un retinoide sistémico que se utiliza en la prevención primaria del cáncer cutáneo no melanoma. El imiquimod es un inmunomodulador aprobado para el tratamiento, entre otros, de CBC superficiales no faciales menores de 2cm. Estudios previos han demostrado una acción sinérgica anticarcinogénica de ambos fármacos, tanto in vivo como in vitro. Dicha combinación produjo en nuestros pacientes una gran reducción de la masa tumoral, lo que nos permitió aplicar posteriormente un tratamiento definitivo con la remisión completa de los CBC.
Basal cell carcinoma (BCC) is the most common tumor in humans. The incidence of this type of cancer in Spain is calculated to be 253 cases per 100 000 individuals per year.1 The treatment with the highest cure rate is complete excision. However, depending on the size of the lesion and its location, this approach can be disfiguring and thus poorly accepted by the patient. The therapeutic options presented in such cases include electrosurgery, radiotherapy, topical imiquimod, 5-fluorouracil, and photodynamic therapy.2,3 We report on 2 patients with giant BCC who received a combination of oral acitretin and topical imiquimod as neoadjuvant treatment to reduce the size of the tumor.
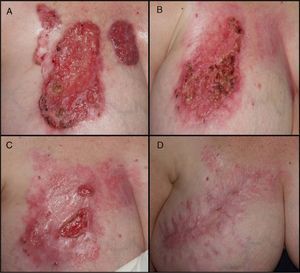
Case DescriptionPatient 1Our first patient was a 68-year-old woman with psoriasis since childhood for which she had received several topical treatments and UV-B phototherapy. She consulted in 2002 for a series of skin lesions that had developed gradually over the previous 10 years and that she felt were associated with her underlying skin condition. Nine of the lesions comprised erythematous desquamative plaques with pearly borders on the lower limbs and trunk. The lesions measured 1 to 4cm in diameter, and some had small dots and globules of gray pigment Two ulcerated lesions were present on her chest; these also had pearly borders with pigmented areas and measured 11 x 18cm and 4 x 8cm (Fig. 1A). Analysis of a punch biopsy specimen confirmed them as micronodular BCC. The patient was initially examined at the breast cancer unit, where she refused surgery owing to the potentially considerable damage arising from complete resection of the tumor. Her case was referred to the skin tumor board of our department, where we suggested reducing the size of the tumor using alternative treatment. We prescribed oral acitretin (25mg/d) combined with daily topical imiquimod 5% cream. Flu-like symptoms appeared 2 months later; the dose of imiquimod was reduced to 3 alternate days per week, and her symptoms resolved. At 4 months, the smaller lesion had completely disappeared, and the larger lesion was reduced in size by 30% at 4 months (Fig. 1B) and 70% at 6 months (Fig. 1C). Of note, analysis of biopsy specimens revealed recurrence of several of the tumors on the lower limbs, which were not treated with topical imiquimod. Even though treatment lasted 9 months, the size of the main tumor remained stable for the last 3 months. At this point, the residual tumor (5 x 7cm) was treated with surgery. No recurrence of giant BCC has been detected after 8 years of follow-up (Fig. 1D).
A, Two eroded giant basal cell carcinomas on the right side of the chest. B, Significant improvement in the lesions after 4 months of treatment with oral acitretin and imiquimod 5% cream. C, Reduction in the size of the tumor (70%) after 6 months. D, No signs of recurrence and acceptable cosmetic outcome 2 years after surgery.
Our second patient was a 63-year-old man who consulted for an ulcerated tumor (10 x 7cm) with pearly borders on the right cheek and temple. Histopathology confirmed the tumor to be infiltrative BCC. Given the size and location of the lesion, the skin tumor board rejected conventional approaches such as surgery and radiotherapy. The favorable outcome reported in the case described above led the board to recommend starting combination therapy with imiquimod 5% cream and oral acitretin (25mg/d). Marked inflammation was evident 1 month later (Fig. 2B). After 15 weeks, the size of the tumor had been reduced to a maximum size of 3 x 4cm. However, after 6 months, the tumor was seen to be progressing, possibly owing to a lack of adherence. As the patient refused surgery, we decided to initiate local radiotherapy (200 cGy administered in 30 doses) (Fig. 2C). No recurrence of giant BCC has been detected after 2 years of follow-up (Fig. 2D).
A, Ulcerated giant basal cell carcinoma on the right cheek and temple. B, Impetiginous exudative erythematous tumor plaque after application of topical imiquimod 5% combined with oral acitretin for 1 month. C, Granulation tissue after 2 months of local radiotherapy. D, Permanent resolution of the tumor at 15 months of follow-up.
Radical resection is the most effective treatment for BCC. However, this approach can prove traumatic if the lesions are in functional areas or affect the patient's appearance.4 We found that the combination of oral retinoids and topical imiquimod was effective as neoadjuvant treatment to reduce the size of the tumor in 2 patients with giant BCC.
Retinoids are used in the primary prevention of nonmelanoma skin cancer in high-risk patients, such as transplant recipients, although they are also an option in the treatment of premalignant and malignant skin lesions. These agents regulate the cell cycle by acting on differentiation, inhibiting growth, and inducing apoptosis. In addition, they improve the cellular immune response and antagonize some well-known tumor promoters.5 We were able to find only 1 case of giant BCC (7cm, multifocal) treated with oral retinoids in which the tumor remitted completely.6 However, the follow-up period in that study was very short.
Imiquimod is an immunomodulator that induces production of interferon (IFN) α by monocytes and dendritic cells. INF-α in turn interacts with type 1 helper T cells to induce release of INF-γ and interleukin 2. Thus, it functions as an antiviral agent and favors long-term immunologic memory against tumor cells.7,8 Imiquimod has proven effective in different studies on the treatment of nodular and superficial BCC, with cure rates ranging from 60% to 100%, depending on the regimen. The type and depth of the tumor affect the response to treatment, although the results of one prospective study indicate that the initial tumor area is the main predictor of remission.9 Some cases of superficial giant BCC have resolved with topical imiquimod at different doses.10,11
Retinoids have been considered to have a synergistic effect when combined with imiquimod, IFN-α, or both. These effects are associated with more intense induction of specific genes stimulated by INF-α, including 2’-5’-oligoadenylate synthetase and protein kinase R. A study of pulmonary cancerous MCF-7 cells treated with a combination of retinoids and INF-α revealed overregulation of STAT1, an essential component of the signaling pathways of INF-α/β and INF-γ. Stimulation of this pathway could account for the effects of the combination of both agents on renal cancer cells, melanoma, and respiratory papillomatosis.12 Other studies point to additive antineoplastic activity arising from the synergistic inhibition of angiogenesis.13,14 To our knowledge, 2 patients with multiple BCCs (<2cm) have been treated with this combination.15,16 The first had xeroderma pigmentosum and the second had received Grenz ray therapy on the scalp as a child. Neither of the two was willing to undergo further surgery; therefore, both patients were prescribed oral acitretin and imiquimod 5% cream—the regimen was not described in the report—and the lesions resolved. Our review of the literature revealed no patients with giant BCC treated with this combination.
The combination of topical imiquimod 5% and oral retinoids to treat giant BCC did not completely resolve the tumor in our patients, although it did prove useful as neoadjuvant treatment by reducing the size of the tumor, thus enabling us to subsequently administer definitive treatment of the residual BCC. As the imiquimod regimen we prescribed was longer than recommended in the summary of product characteristics, symptoms and laboratory findings were closely monitored. The combination was adequately tolerated in both cases, and no notable adverse effects were recorded. It is worth noting that application of imiquimod to such a large ulcerated area induced systemic symptoms and resolved tumors at some distance from the treatment area. Furthermore, given that the tumor stabilized in both cases despite treatment, it would be important to establish whether some as yet unknown variable—histologic subtype, tumor area, or development of tolerance to imiquimod—could affect the response to therapy. The absence of a control group comprising patients treated with imiquimod only prevents us from knowing to what extent acitretin improved the results of therapy.
ConclusionWe believe that both of the cases we report illustrate a new therapeutic option in the neoadjuvant treatment of giant BCC, thus facilitating subsequent application of other definitive treatments. However, further studies are necessary to help us understand the synergistic or additive action of both drugs and their therapeutic potential.
Conflicts of InterestThe authors have no conflicts of interest to declare.
We are grateful to Dr Ramón Egido (Histopathology Department, Hospital Arnau de Vilanova, Lleida) for his help with diagnosis and to Drs Moisés Mira (Radiotherapy Department, Hospital Arnau de Vilanova, Lleida) and Elena Aguirre (Oncology Department, Hospital Arnau de Vilanova, Lleida) for their help with treatment.
Please cite this article as: Sanmartín V, et al. Tratamiento neoadyuvante oral e imiquimod tópico en el carcinoma basocelular gigante. Actas Dermosifiliogr. 2012;103:149-152.