Onychopapilloma is a benign tumor of the nail bed and distal matrix of unknown etiology. Classically, it has been described as a localized band of longitudinal erythronychia. However, recently, more clinical signs have been reported. This broad clinical spectrum could be a potential mimicker of other disorders, such as viral warts, melanoma, squamous cell carcinoma, or connective tissue tumors, among others.1,2
Despite being considered a rare tumor, with nearly 205 reported cases found in medical literature,1 onychopapilloma represents the main cause of localized longitudinal erythronychia.3 Some authors consider this entity could even be more common, but remains underreported.4
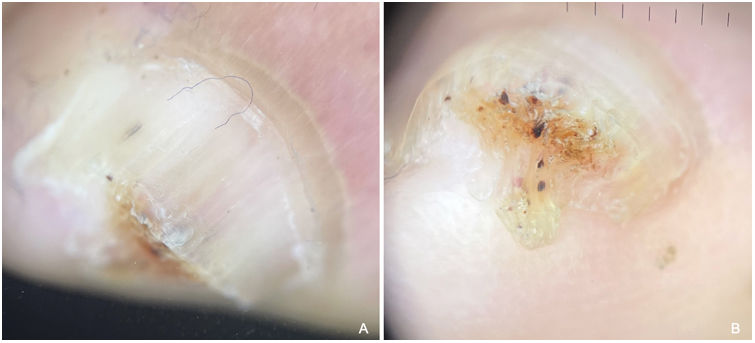
A 56-year-old man (case #1), with Fitzpatrick skin phototype IV, and a past medical history of metabolic syndrome, coronary artery disease and sleep apnea presented to our dermatology clinic with a lesion on his left 3rd toenail. He reported a history of trauma while cutting the mentioned nail 4 years prior, with occasional bleeding and pain. The physical examination revealed the presence of a big hyperkeratotic tumor that shifted laterally toward a portion of the nail plate with a healthy appearance. The 10mm×15mm lesion was very hard on palpation and elicited pain. On dermoscopy, these findings where enhanced. This technique allowed us to identify black dots and lines consistent with splinter hemorrhages (Fig. 1). A nail biopsy was performed with the clinical impression of an onychocytic tumor vs connective tissue tumor.
A 72-year-old man (case #2), with Fitzpatrick skin phototype IV, and a past medical history of metabolic syndrome presented for evaluation of a longitudinal yellow streak on his left 4th toenail, which had been treated as a wart at a different dermatology clinic. On physical examination, subungual hyperkeratosis, splinter hemorrhages, and yellow chromonychia were seen. Findings were limited to the distal half of the nail plate, with no changes in the lunule or proximal fold. On dermoscopy of the free edge, thickening of the central nail plate was noticed, where overlying black-reddish dots and lines were found over an orange background. The inferior portion of the tumor seemed to extend toward the fingertip, resembling a ventral pterygium (Fig. 2). A biopsy was performed with a diagnostic impression of Squamous-cell-carcinoma vs viral wart.
Case #2. Dermoscopy. (A) Yellow chromonychia and splinter hemorrhages on the left 4th toenail. (B) Onychoscopy of the free edge showing thickening of the central nail plate, black-reddish dots, and lines over an orange background. The ventral portion of the tumor resembles a ventral pterygium.
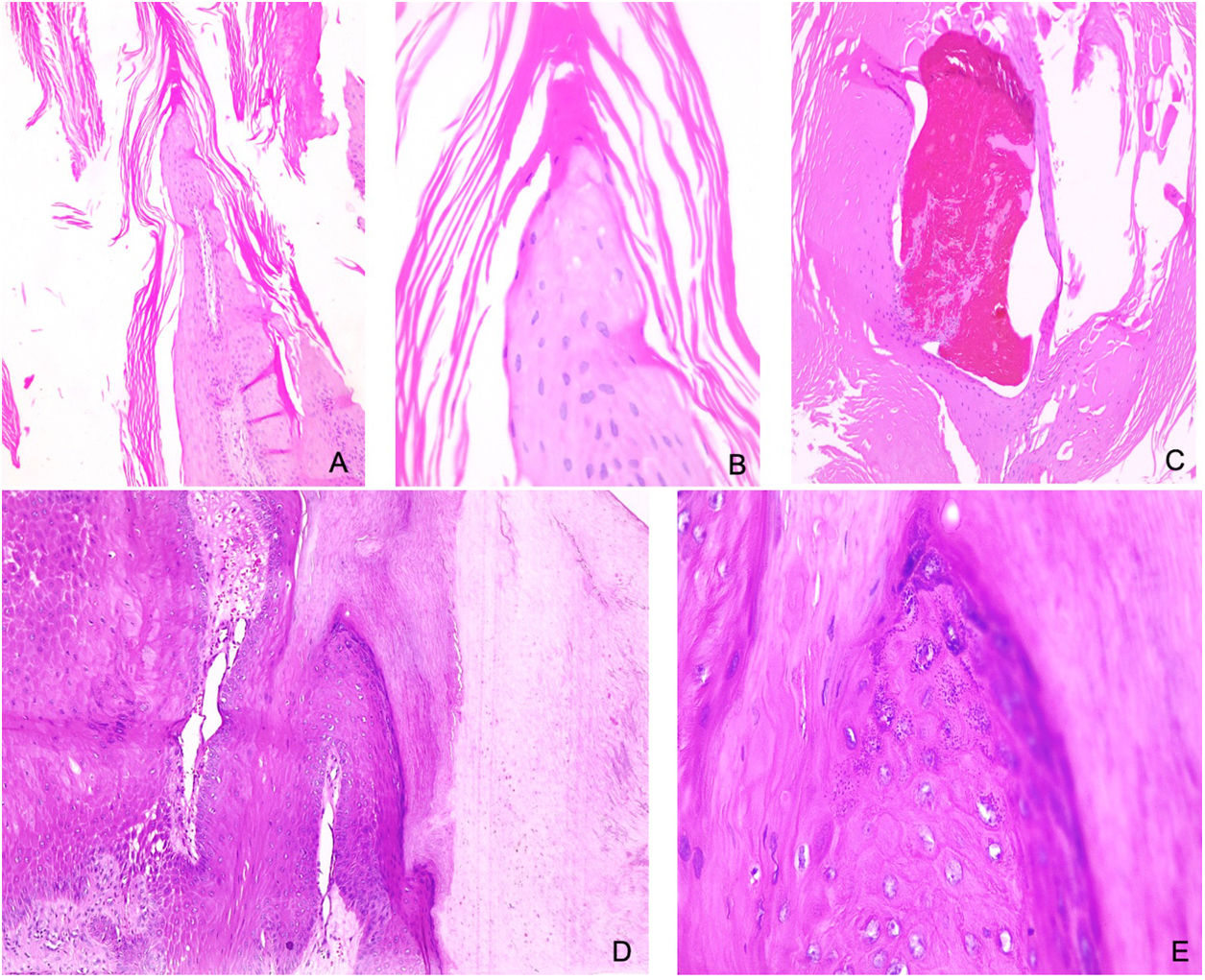
On microscopic examination of both cases, a hyperkeratotic and parakeratotic stratum corneum, associated with Malpighi stratum papillomatosis and koilocytic changes was seen, leading to a diagnosis of onychopapilloma (Figs. 3). The finding of an excessively cellular chorion in case #1 prompted us to perform additional immunohistochemical studies that tested negative for S100, CD34, CD99, smooth muscle actin, desmin, h-caldesmon, EMA and XIIIA factor. This cellular chorion strongly tested positive for trichrome staining, indicating thick collagen bundles, Ki-67 cell proliferation index <1%. Based on the clinical and histopathological findings, the diagnosis of onychopapilloma was eventually confirmed (Fig. 3).
Case #1. Pathology. 10×, 40× and 40× (A, B, C, respectively). Nail matrix with hyperkeratotic stratum corneum associated with parakeratosis, hemorrhagic foci, and serous exudate. Malpighi stratum displays papillomatosis and subtle koilocytic changes. Case #2. Pathology. 10× and 40× (D, E, respectively). Nail matrix with hyperkeratosis and parakeratosis, Malpighi stratum with papillomatosis, hypergranulosis, and koilocytic changes.
Onychopapilloma was first described in 1995 by Baran and Perrin who reported four cases of longitudinal erythronychia.1 Multiple hypotheses on its origin have been proposed: (1) a neoplastic hyperplasia of nail bed epithelium due to trauma or chronic irritation; (2) a reaction to concurrent nail inflammatory disorders, such as lichen planus.6 However, its etiology remains unknown to this date.2
It often presents with longitudinal chromonychia associated with localized subungual hyperkeratosis, splinter hemorrhages and distal onycholysis, and in some cases, a nail plate fissure.7 It can also present with isolated splinter hemorrhages, which may be unique or multiple, long, or short.8
Onychopapilloma occurs more frequently on the nails of the 1st finger of the hand.5 Starace et al.1 reported 17 cases of histopathologically confirmed onychopapilloma, with involvement of just 1 finger in all the cases, and damage to the fingernails in 15 cases, more often on the left thumb nail.
Dermoscopy has proven useful in the evaluation of the nail apparatus, being practical for the diagnosis and prognosis of multiple disorders,3 and for the assessment of therapeutic outcomes.5 The onychoscopy of onychopapilloma reveals a well-demarcated longitudinal band extending from the lunule toward the free edge, with irregular violaceous-to-black lines consistent with splinter hemorrhages, and associated with the presence of a subungual hyperkeratotic and phylliform mass in the hyponychium, which can be seen on the nail free edge.5,7
Despite being a benign tumor, a case of an onychopapilloma with malignant histopathology has recently been reported associated with symptoms such as pain and bleeding.4 Although onychopapilloma can eventually cause symptoms, when these are present and associated with atypical clinical presentations, they could be warning signs, and pathological examination should be performed to rule out malignancy, such as in case #1.
In conclusion, onychopapilloma may have various atypical clinical presentations, mimicking malignant tumors. Dermoscopy may aid on its evaluation in typical cases, but in the case of bizarre presentations, only histopathological studies can confirm the final diagnosis.
Conflict of interestThe authors declare that they have no conflict of interest.