The patient was a 64-year-old man with chronic lymphocytic leukemia, which required treatment with chemotherapy and allogeneic umbilical cord blood transplantation. He was also on multiple drugs, in particular systemic prednisone and tacrolimus. Ten months after the transplantation, the patient developed a slow-growing pruriginous lesion on the right leg.
Physical ExaminationPhysical examination revealed a well-defined and painless tumor-like lesion on the right leg measuring 4cm, with secretion of a hemoserous discharge through several holes (Fig. 1). No granules were observed in the discharge.
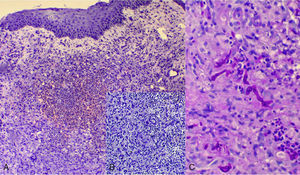
HistopathologyHistological study revealed an intense mixed inflammatory and granulomatous infiltrate in the dermis, several abscesses, and multinucleated Langerhans giant cells and foreign body giant cells (Figs. 2A and 2B). PAS staining highlighted thick-walled septate structures and others with a rounded morphology (Fig. 2C).
Additional TestsLaboratory test findings showed mild anemia and neutropenia (1100 neutrophils/mm3). Exudate and biopsy tissue specimens were cultured on Sabouraud agar.
What Is Your Diagnosis?
DiagnosisEumycetoma caused by Cylindrocarpon sp.
Clinical CourseWhite and downy colonies with a ragged appearance were isolated in Sabouraud agar. Microscopic examination showed elongated, septate, hyaline hyphae together with smooth-walled, septate, hyaline spores characterized by rounded apical cells and a tendency to cluster (Fig. 3). Based on the microscopic findings, we identified a filamentous fungus belonging to the genus Cylindrocarpon.
After treatment with oral voriconazole did not yield any response, the patient required intravenous liposomal amphotericin B and subsequent excision of the lesion.
CommentMycetoma is a chronic granulomatous infectious disease endemic in tropical and subtropical countries. There are two distinct types: actinomycetoma (caused by Nocardia and Actinomycetes species), and eumycetoma (caused by true fungi). Of the two, eumycetoma is more common.1–3
In the present case, we identified a fungus of the genus Cylindrocarpon. This saprophytic fungus is only slightly pathogenic in that it mainly only affects immunocompromised patients with hematologic malignancies.4–7
Mycetoma is more common in young men, agricultural workers, and travelers. Risk factors include a lack of protective footwear, wounds in unprotected areas, malnutrition, and immunosuppression. The disease is caused by direct inoculation of the infectious agent following trauma with a contaminated object. The lower limbs, especially the feet (80%), are the most common site. The incubation period ranges from a few weeks to several months.1,3
Eumycetoma develops as a painless, slow-growing lesion, while actinomycetoma grows more quickly and is characterized by localized tissue destruction and inflammation. A common characteristic is the formation of sinus tracts that discharge a purulent or serosanguinous exudate containing the characteristic grains or granules, which are the fungal colonies.1,3,8
The morphological characteristics of the isolated fungi are essential for diagnosis. Species of the genus Cylindrocarpon spp. are very similar to those of the genus Fusarium spp., which complicates the diagnosis. The presence of thin-walled hyaline conidia with rounded apical cells, and the absence of the basal, foot-shaped cells typical of the genus Fusarium spp. are findings that indicate the genus Cylindrocarpon. The characteristics of the granules also help to identify the etiologic agent. Species of the genus Cylindrocarpon spp. usually produce white grains.4,5,7
The differential diagnosis should include lipoma, sarcoma, chronic osteomyelitis, Kaposi sarcoma, tuberculosis, sporotrichosis, and chromoblastomycosis.1–3
Treatment depends on the causative organism. Eumycetoma is treated with oral or intravenous antifungal agents (ketoconazole, itraconazole, or liposomal amphotericin B) combined with broad surgical resection. Care must be taken not to rupture the capsule during surgery to avoid spread to surrounding tissues. Actinomycetoma is treated with antibiotics, such as trimethoprim-sulfamethoxazole, amikacin, or minocycline. The therapeutic response is better in actinomycetoma than eumycetoma. Without proper treatment, mycetoma can cause severe deformities and lead to amputation of the affected limb and even death.1,3,9
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Vázquez-Osorio I, Pereiro M, Toribio J. Lesión tumoral de reciente aparición en paciente inmunodeprimido. Actas Dermosifiliogr. 2016;107:243–244.