Malignant umbilical skin lesions, although infrequent, usually require treatment that includes partial or total omphalectomy.1 Given the esthetic importance of the umbilicus in the abdominal wall, its reconstruction must be considered when planning surgical treatment.
Neoumbilicoplasty with an island pedicle flap can be performed in parallel with the omphalectomy, and provides adequate esthetic results. Although well described in dermatology for the reconstruction of central facial defects, the use of this technique in this anatomical location has been described on only a few occasions.2–4
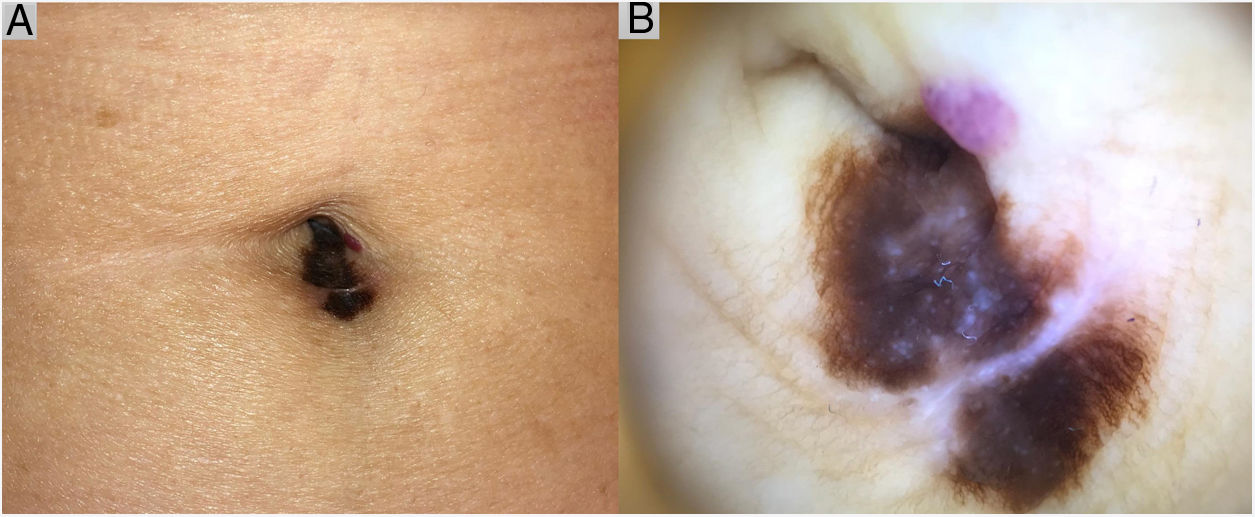
Case DescriptionAn 82-year-old patient was evaluated for the growth of an asymmetric, melanocytic umbilical lesion (12 × 6 mm) with irregular borders and heterochromia, and, on dermoscopy, an atypical pigment network, grayish-blue dots, and whitish areas (Fig. 1). A partial biopsy was performed given the patient’s initial refusal to undergo surgery. Histology revealed a predominantly in situ, superficial spreading melanoma, with extensive underlying regression and an invasive component of 1.25 mm thick, without ulceration or mitotic activity. Wide excision with 2-cm margins was scheduled. A tumor extension study, including inguinal ultrasound and computerized axial tomography, revealed no findings of relevance. The patient refused to undergo a sentinel node biopsy.
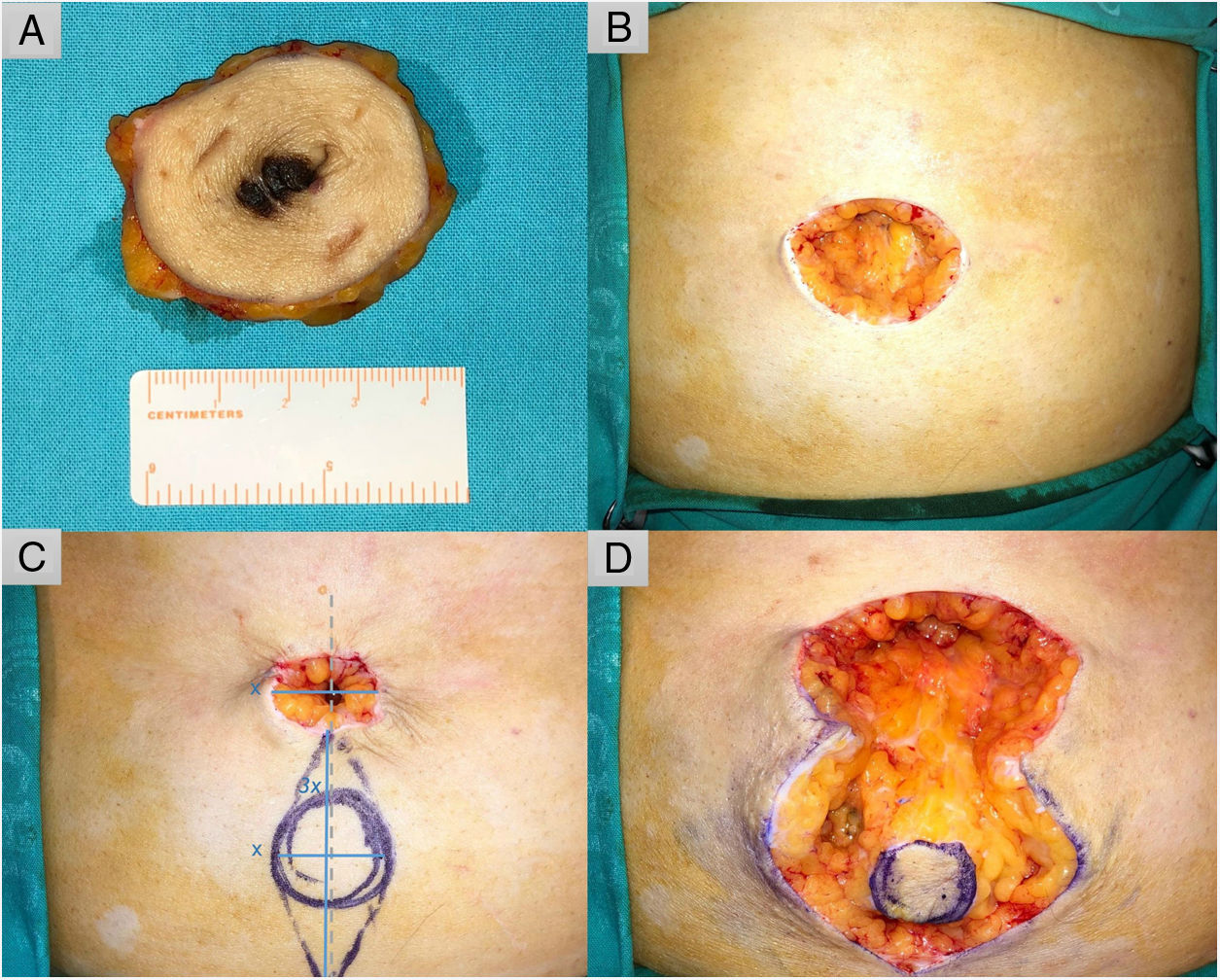
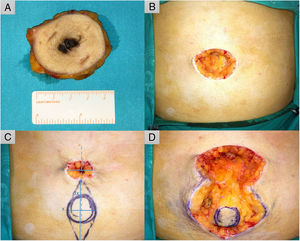
TechniqueUnder local anesthesia, circular excision of the lesion is performed first (Fig. 2A). Next, the size of the defect is reduced (Fig. 2B) using a transient subcutaneous purse-string suture to calculate the size of the plasty (x) (Fig. 2C). A spindle-shaped incision is designed with the major axis coinciding with the central point of the defect. The length of the major axis is 3 times that of the defect (3x), while that of the minor axis corresponds to the length of the defect (x) (Fig. 2C).5 A tobacco pouch is created to facilitate subsequent resection of the lateral triangles and dissection of the island, providing a subcutaneous pedicle long enough for transfer to the site of the defect (Fig. 2D). The pedicle is fixed to the anterior rectus abdominis sheath using a transfixing U-stitch with a 3−0 polydioxanone suture, lending the plasty the conical shape of the umbilicus. The perimeter of the neo-umbilicus is sutured to the surrounding skin using loose stitches and the rest of the incision using a continuous running 4−0 suture (polyamide 6) (Fig. 3A).
A, Wide excision of the lesion with 2-cm margins. B, Surgical defect (40 × 30 mm). C, Planning of reconstruction using an island pedicle flap. The minor axis of the spindle-shaped incision is calculated to ensure a transitory tobacco-pouch closure (x). The major axis is 3 times the length of the minor axis (3x) and runs along the midline of the defect (gray dashed line). D, The tobacco pouch is released, and the lateral triangles are removed, leaving a circular skin island that is dissected together with an adipose pedicle that enables its movement to the desired position.
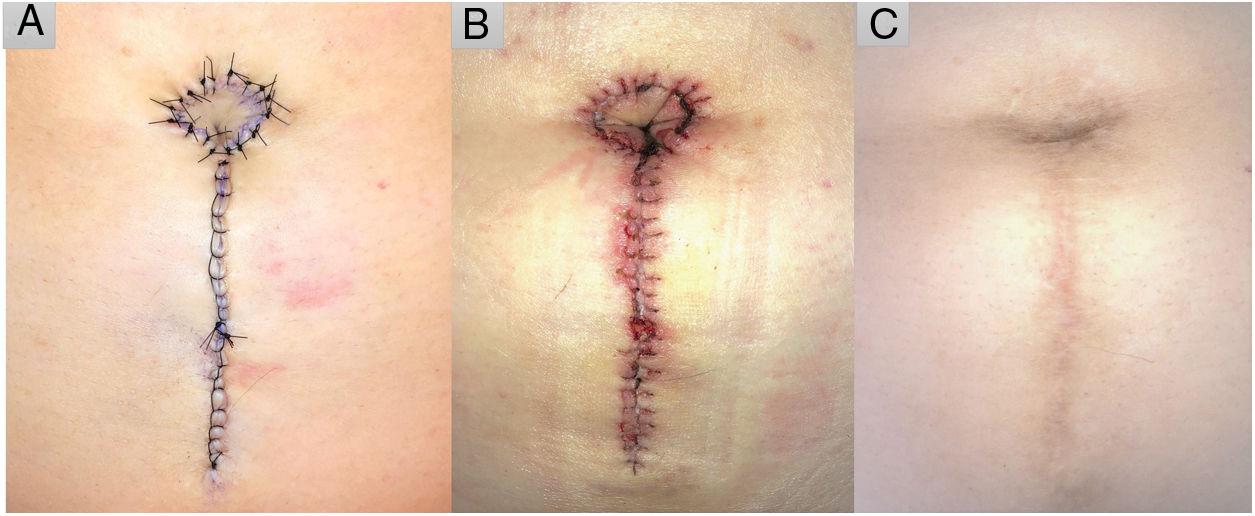
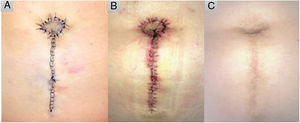
The island is moved to the desired position and fixed to the anterior sheath of the rectus abdominis muscle with a transfixing U-stitch to give it a conical shape. The skin surrounding the neo-umbilicus is sutured with loose stitches and the remainder with a continuous running suture. A, Immediate postoperative result. B, After suture removal, 14 days later. C, Ten months after the surgical intervention.
The patient underwent antibiotic prophylaxis with a single dose of oral cephradine (2 g) 30 min before surgery and a compression bandage was applied for 48 hours, followed by regular wound care. The sutures were removed after 2 weeks (Fig. 3B) and the patient was subsequently followed for 10 months with no complications (Fig. 3C).
DiscussionThe techniques used to create a neo-umbilicus vary in design and technical complexity. The main techniques used are plasties (Borges technique, V plasty, C–V plasty, unfolded cylinder plasty, lunch-box-type plasty, double V–Y plasty), using rotation flaps, triangular flaps, reverse fan-shaped flaps, island flaps, M-shaped or inverted omega-shaped flaps, and, less frequently, grafts.6 Complications of these procedures include necrosis of the plasty, infections, hematoma formation, suture dehiscence, scar hypertrophy, and umbilical flattening.6
Plasty with an island pedicle flap offers a series of advantages including concordance of color, texture, and thickness of the tissues, and avoids the compromise of other anatomical areas.4 Plasty is performed with a generous vascular pedicle, reducing the possibility of necrosis, and involves little tension during closure, therefore reducing the likelihood of dehiscence. Moreover, recovery time is relatively short. Many of the more common techniques, particularly those that leave no visible scars and have excellent esthetic results,7 use healthy abdominal skin, and therefore need not contemplate the removal of a pre-existing umbilicus, periumbilical lesions, small surgical defects, or excess skin resulting from a hernia when constructing the neo-umbilicus. Plasty with an island pedicle flap allows concealment of moderate-sized defects such as that resulting from omphalectomy, and can be performed as part of the same surgical procedure under local anesthesia, ensuring a very adequate esthetic result. For this anatomical location, island plasty has been described using a horizontal orientation, whereby the skin of the island is included in the incision closure and a central transfixing point,3 or a vertical orientation, in which skin is taken from the area adjacent to the lesion and transformed into a conical shape.2 We feel that the vertical orientation promotes better closure with less tension and provides a preferable esthetic result. Moreover, the use of a transfixing U-stitch facilitates the conical transformation.
In conclusion, we propose island plasty with a vertical orientation and a central transfixing stich as a simple, safe, and esthetic technique for umbilical reconstruction after oncological surgery.
FundingThis work did not receive any type of funding.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Vergara de la Campa L, Brinca A, Pinho A, Vieira R. Neoumbilicoplastia mediante plastia en isla vertical. Actas Dermosifiliogr. 2020;111:899–902.