There is debate in the literature regarding the management of basal cell carcinoma following excision with positive surgical margins. While in some cases recurrence is not observed even after many years of follow-up, those in which recurrence does occur are at an increased risk of complications.
Factors may exist that help to choose the best therapeutic approach for basal cell carcinomas on the head in which positive margins are observed following excision.
Material and methodsA total of 46 patients were selected who had been treated by Mohs micrographic surgery as a result of positive surgical margins being present following previous tumor excision. The factors associated with the absence of tumor nests and the occurrence of negative margins following a single Mohs stage were analyzed.
ResultsNo associations were observed with sex, tumor size, affected margin (lateral, deep, or both), time since diagnosis, number of previous treatments, histological type, or tumor site. There was a certain trend towards more frequent identification of tumor remnants when both surgical margins were affected and towards a requirement for a single Mohs stage in tumors less than 1.2cm and in which less than 5 years had elapsed since diagnosis.
ConclusionsConclusive data are unavailable with which to define cases in which re-excision is necessary or those in which conventional excision could be sufficient. The best option for the treatment of these tumors is Mohs micrographic surgery, although conventional excision could be reasonable in small tumors located at low-risk sites and in which long periods have not elapsed since diagnosis.
La actitud ante los carcinomas basocelulares que han sido extirpados con márgenes afectos es controvertida en la literatura. Frente a casos que no recidivan incluso tras muchos años de seguimiento, hay riesgo de complicaciones en aquellos que sí lo hacen.
Podrían existir factores que ayuden a escoger la mejor opción terapéutica para los carcinomas basocelulares localizados en la cabeza y extirpados con márgenes afectos.
Material y métodosSe seleccionaron 46 pacientes tratados mediante cirugía de Mohs por haber sido previamente extirpados con afectación de márgenes. Se valoró qué factores se asociaron a la ausencia de restos tumorales y qué factores estaban asociados a la obtención de márgenes negativos con un único estadio.
ResultadosNo se consiguió ninguna relación significativa con el sexo, el tamaño tumoral, el margen que estaba afecto (lateral, profundo o ambos), el tiempo de evolución, el número de tratamientos previos, el tipo histológico ni la localización. Hubo una cierta tendencia a encontrar más frecuentemente restos tumorales en las áreas perioficiales de tumores con ambos márgenes afectos, y a necesitar un único estadio en los tumores de menos de 1,2cm y con menos de 5 años de evolución.
ConclusionesNo existen datos concluyentes que permitan definir en qué casos puede no ser necesaria la reextirpación ni en cuáles puede ser suficiente una exéresis convencional. La mejor opción para el tratamiento de estos tumores es la cirugía de Mohs, aunque podría ser razonable realizar exéresis convencional en tumores pequeños de poco tiempo de evolución en localizaciones de bajo riesgo.
In daily clinical practice it is not uncommon to see cases of basal cell carcinoma (BCC) with involvement of the margins after excision but that present no recurrence even after many years of follow-up. Studies have shown that between 33% and 90% of incompletely excised BCCs do not recur after excision, independently of their histological type.1–7 The maximum number of tumor recurrences has been detected in series with a predominance of morpheaform BCC, with recurrence rates as high as 100%, although that rate has been reported in studies with few cases.8 We should keep in mind that the risk of further recurrences among tumors that have recurred once is over 50%,9,10 and that the treatment of lesions in certain areas can be difficult. On the other hand, an absence of residual tumor has been observed in the surgical specimens from many BCCs after re-excision due to positive surgical margins. In a series of 52 cases in which this finding was studied, residual tumor was detected in only 11 cases (21%).11 It would appear reasonable to consider that persistence of a tumor could be due to various factors and tumor characteristics, such as time since diagnosis, previous treatments, site of the tumor, and histological type.
Despite the low recurrence rate, the majority of authors defend the need for re-excision because of the potential complications, particularly in high-risk areas.11 Several authors have suggested that the best approach in tumors with positive margins is Mohs micrographic surgery.6,12 However, this mode of surgery is not available at most centers and is more costly than conventional surgery, though it should be remembered that cost-benefit studies have found that the cost is higher in low-risk but not high-risk tumors.13,14 In our experience, the majority of low-risk BCCs require only 1 Mohs stage to achieve tumor-free margins. It would therefore be interesting to determine whether there is a real need to use this technique for re-excision in these cases and, in particular, whether there are cases in which simple excision could represent a more straightforward solution.
Based on the above data, we hypothesized that BCCs with positive margins after excision could present features that would indicate the most appropriate therapeutic approach to be used: monitoring, conventional surgery, or Mohs micrographic surgery.
Our study had 2 objectives. The first was to identify factors that could predict which cases of BCC on the face or scalp—the areas with the highest risk of complications in the event of recurrence—re-excised using Mohs micrographic surgery because of positive margins would not present residual tumor in the surgical specimens. The second objective was to find characteristics associated with free margins with a single stage of Mohs surgery that could be used to select a subgroup of patients in which re-excision could be performed using conventional surgery.
Patients and MethodsWe selected 46 patients with BCC in which histological involvement of the surgical margins had been detected after simple excision and whose definitive treatment was performed in the dermatology department of the Instituto Valenciano de Oncología in Valencia, Spain, using Mohs micrographic surgery, between January 1996 and May 2009.
The response variable was defined as the presence or absence of residual deposits of BCC in the histology study of the material excised during Mohs surgery. Using the standard procedure for Mohs surgery, 100% of the margins of the surgical specimen were studied on the fresh sample. This was followed by histological study of the remaining material, that is, the skin present between the margins evaluated in the fresh specimen and the scar of the previous excision, after embedding in paraffin. The paraffin-embedded specimen underwent conventional processing, which would suggest that only 5% to 10% of the sample was examined. Residual tumor was considered to be absent when only 1 stage of Mohs surgery was required to achieve negative margins, associated with an absence of tumor deposits in the subsequent study of the surgical specimen after embedding in paraffin. The response was also defined according to the number of stages of Mohs surgery necessary to achieve free margins, and this was dichotomized into 2 categories: 1 stage and more than 1 stage.
The explanatory variables included the following characteristics: demographic characteristics (sex of the patient and age at the time of definitive surgery); and data recorded on the excised tumor after a review of the medical history and the pathology report, including histological type (nodular, micronodular, infiltrative, morpheaform, basosquamous, or not specified), determination of the presence or absence of perineural invasion, the margins affected in the previous surgery (lateral, deep, or both), site of the tumor, and diameter in centimeters of the lesion prior to the previous surgery. The medical history was also used to determine the time since diagnosis of the lesion (considered from the date the tumor was first diagnosed), and the number and type of previous treatments (conventional surgery, cryotherapy, electrocoagulation, radiation therapy, immunotherapy, and photodynamic therapy).
For the analysis, all quantitative variables were categorized and the differences in the distribution of each variable according to the response variable were evaluated using the X2 and Fisher tests. The odds ratios and their corresponding 95% confidence intervals (CIs) were calculated using logistic regression. A P value less than .05 was considered statistically significant.
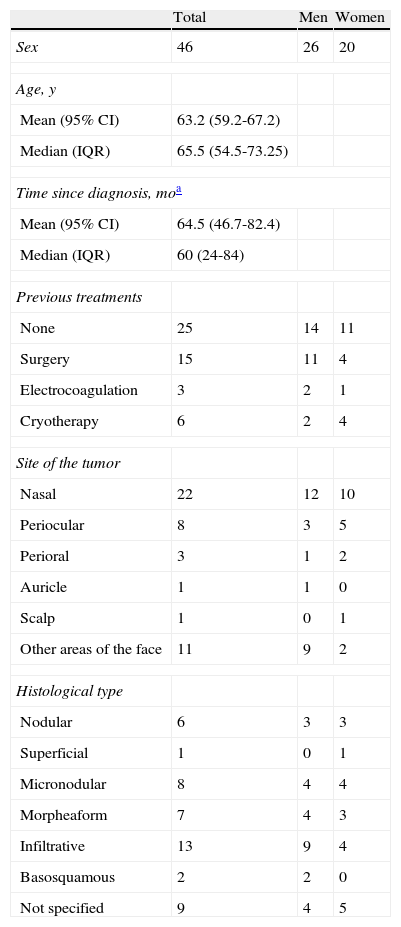
ResultsThe study group was formed of 20 women (43.5%) and 26 men (56.5%), with a median age of 65.50 years (interquartile range [IQR], 54.50-73.25 years) and a mean age of 63.2 years (95% CI, 59.2-67.2). The characteristics of the study group are detailed in Table 1. The time since diagnosis of the tumors varied between 6 and 240 months, with a median of 60 months (IQR, 24-84 months) and a mean of 64.5 months (95% CI, 46.7-82.4). The median largest diameter of the lesions was 1.5cm (IQR, 1-2cm), with a mean of 1.59cm (95% CI, 1.26-1.93), and they had been treated a median of 0 times (IQR, 0-1) and a mean of 0.85 times (95% CI, 0.47-1.22).
Patient Characteristics.
| Total | Men | Women | |
| Sex | 46 | 26 | 20 |
| Age, y | |||
| Mean (95% CI) | 63.2 (59.2-67.2) | ||
| Median (IQR) | 65.5 (54.5-73.25) | ||
| Time since diagnosis, moa | |||
| Mean (95% CI) | 64.5 (46.7-82.4) | ||
| Median (IQR) | 60 (24-84) | ||
| Previous treatments | |||
| None | 25 | 14 | 11 |
| Surgery | 15 | 11 | 4 |
| Electrocoagulation | 3 | 2 | 1 |
| Cryotherapy | 6 | 2 | 4 |
| Site of the tumor | |||
| Nasal | 22 | 12 | 10 |
| Periocular | 8 | 3 | 5 |
| Perioral | 3 | 1 | 2 |
| Auricle | 1 | 1 | 0 |
| Scalp | 1 | 0 | 1 |
| Other areas of the face | 11 | 9 | 2 |
| Histological type | |||
| Nodular | 6 | 3 | 3 |
| Superficial | 1 | 0 | 1 |
| Micronodular | 8 | 4 | 4 |
| Morpheaform | 7 | 4 | 3 |
| Infiltrative | 13 | 9 | 4 |
| Basosquamous | 2 | 2 | 0 |
| Not specified | 9 | 4 | 5 |
Abbreviations: CI, confidence interval; IQR, interquartile range.
Previous treatments included conventional surgery (with or without subsequent reconstruction), electrocoagulation, and cryotherapy. The operation that gave rise to the indication for Mohs surgery due to the presence of positive margins was not included in the classification of patients according to previous treatment. Treatments prior to the operation that gave rise to the indication for Mohs surgery included other surgical approaches in 15 cases (32.6%), electrocoagulation in 3 (6.5%), and cryotherapy in 5 (10.9%) (some patients had been treated on more than 1 occasion).
The tumors were of the following histological types: nodular (n=6, 13.0%), superficial (n=1, 2.2%), micronodular (n=8, 17.4%), infiltrative (n=13, 28.3%), morpheaform (n=7, 15.2%), basosquamous (n=2, 4.3%), and not specified (n=9, 19.6%). Perineural invasion was observed in only 2 cases (4.3%).
Prior to Mohs surgery, only the lateral margins were affected in 9 patients (19.6%), only the deep margins in 12 patients (26.1%), and both lateral and deep margins in 22 patients (47.8%). The affected margins were not specified in the pathology reports of 3 of the patients.
The tumors were located in the periocular region in 8 patients (17.4%), on the scalp in 1 patient (2.2%), on the nose in 22 (47.8%), in the perioral region in 3 (6.5%), on the ear in 1 (2.2%), and on other areas of the face in 11 (23.9%).
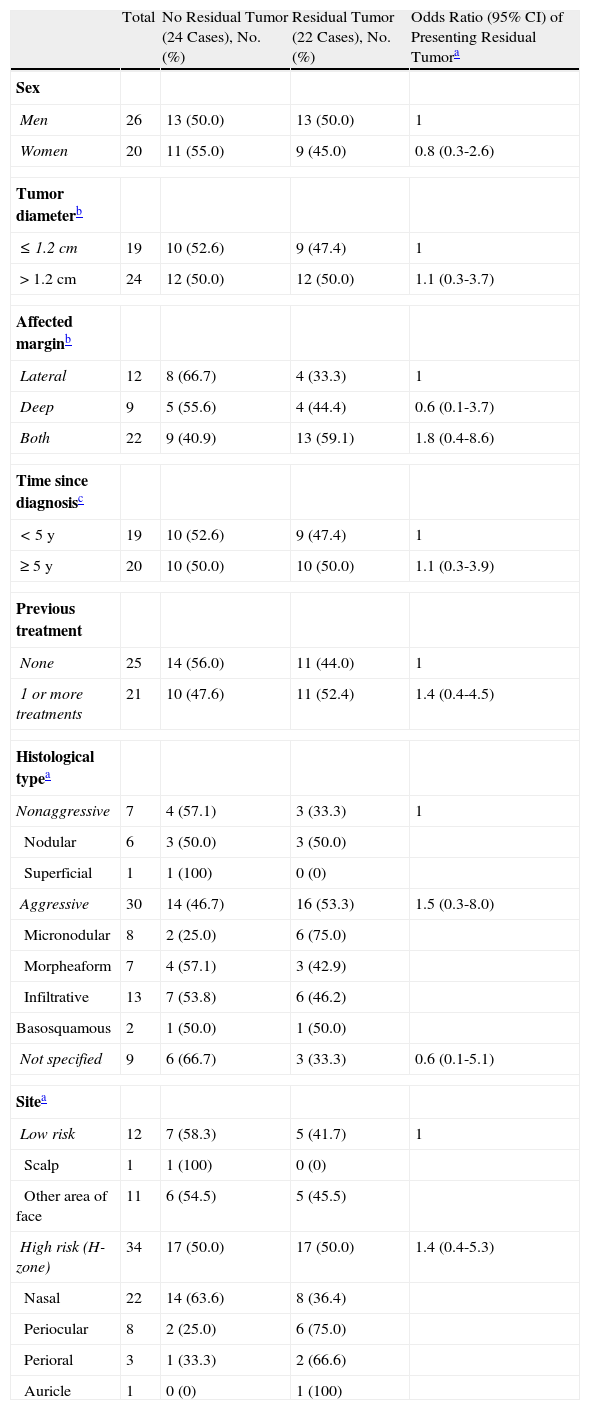
First we analyzed the differences between 2 groups defined according to the presence or absence of residual tumor in the histology study during Mohs surgery. The results of this analysis are presented in Table 2. No statistically significant differences were found in the distribution of the variables studied in the 2 groups, though interesting trends were observed. With regard to the type of BCC, it was observed that micronodular lesions presented a higher frequency of residual tumor. Six of the 8 micronodular BCCs (75%) presented residual tumor after Mohs surgery. The indication for Mohs surgery was involvement of the lateral and deep borders in 75% of the tumors of this histological type, and involvement only of the deep border in 25%. No marked differences were observed in the frequency of residual tumor in the nodular, infiltrative, morpheaform, or basosquamous types. It is interesting to note that both lateral and deep surgical margins were affected in 70% of the cases of morpheaform BCC, which is a histological type in which the borders of the lesion are less clear.
Analysis of the Relationship Between the Clinical-Pathological Characteristics of the Tumor and the Histological Presence of Residual Tumor in the Surgical Specimen.
| Total | No Residual Tumor (24 Cases), No. (%) | Residual Tumor (22 Cases), No. (%) | Odds Ratio (95% CI) of Presenting Residual Tumora | |
| Sex | ||||
| Men | 26 | 13 (50.0) | 13 (50.0) | 1 |
| Women | 20 | 11 (55.0) | 9 (45.0) | 0.8 (0.3-2.6) |
| Tumor diameterb | ||||
| ≤ 1.2cm | 19 | 10 (52.6) | 9 (47.4) | 1 |
| > 1.2cm | 24 | 12 (50.0) | 12 (50.0) | 1.1 (0.3-3.7) |
| Affected marginb | ||||
| Lateral | 12 | 8 (66.7) | 4 (33.3) | 1 |
| Deep | 9 | 5 (55.6) | 4 (44.4) | 0.6 (0.1-3.7) |
| Both | 22 | 9 (40.9) | 13 (59.1) | 1.8 (0.4-8.6) |
| Time since diagnosisc | ||||
| < 5 y | 19 | 10 (52.6) | 9 (47.4) | 1 |
| ≥ 5 y | 20 | 10 (50.0) | 10 (50.0) | 1.1 (0.3-3.9) |
| Previous treatment | ||||
| None | 25 | 14 (56.0) | 11 (44.0) | 1 |
| 1 or more treatments | 21 | 10 (47.6) | 11 (52.4) | 1.4 (0.4-4.5) |
| Histological typea | ||||
| Nonaggressive | 7 | 4 (57.1) | 3 (33.3) | 1 |
| Nodular | 6 | 3 (50.0) | 3 (50.0) | |
| Superficial | 1 | 1 (100) | 0 (0) | |
| Aggressive | 30 | 14 (46.7) | 16 (53.3) | 1.5 (0.3-8.0) |
| Micronodular | 8 | 2 (25.0) | 6 (75.0) | |
| Morpheaform | 7 | 4 (57.1) | 3 (42.9) | |
| Infiltrative | 13 | 7 (53.8) | 6 (46.2) | |
| Basosquamous | 2 | 1 (50.0) | 1 (50.0) | |
| Not specified | 9 | 6 (66.7) | 3 (33.3) | 0.6 (0.1-5.1) |
| Sitea | ||||
| Low risk | 12 | 7 (58.3) | 5 (41.7) | 1 |
| Scalp | 1 | 1 (100) | 0 (0) | |
| Other area of face | 11 | 6 (54.5) | 5 (45.5) | |
| High risk (H-zone) | 34 | 17 (50.0) | 17 (50.0) | 1.4 (0.4-5.3) |
| Nasal | 22 | 14 (63.6) | 8 (36.4) | |
| Periocular | 8 | 2 (25.0) | 6 (75.0) | |
| Perioral | 3 | 1 (33.3) | 2 (66.6) | |
| Auricle | 1 | 0 (0) | 1 (100) | |
On grouping the BCCs into high-risk (infiltrative, micronodular, morpheaform, and basosquamous) and low-risk (nodular and superficial) histological types, we found that 41.7% of the low-risk tumors presented residual tumor compared to 50% of the high-risk tumors; this difference was not statistically significant.
Although perineural invasion was detected in only 2 of the 46 cases, it should be noted that both cases presented residual tumor in the Mohs surgery specimen.
With regard to previous treatments, it was found that all 3 patients who had been treated using electrocoagulation presented residual tumor in the surgical specimen.
There were also variations in the frequency of residual tumor according to the site of the BCC, although once again the differences were not statistically significant. Residual tumor was detected in 75% of periocular tumors and 66.7% of perioral tumors, compared to frequencies around 40% in lesions on other areas of the face.
With regard to the margins affected, we found residual tumor in 33.3% of cases in which only the lateral margins were affected, compared to 44.4% of cases in which only the deep margins were affected. Residual tumor was detected in 59.1% of cases in which both the lateral and the deep margins were affected.
There were also no significant differences in the presence of residual tumor according to the time since diagnosis of the lesion, although the figure was slightly higher in the tumors present for a longer time (50% in the case of tumors diagnosed more than 5 years earlier compared to 47.4% in those diagnosed less than 5 years earlier).
Residual tumor was observed in 52.4% of cases when the tumor with affected margins was a recurrent tumor, and had therefore received at least 1 previous treatment before the intervention that led to the indication for Mohs surgery, compared to 44% in cases of primary tumors.
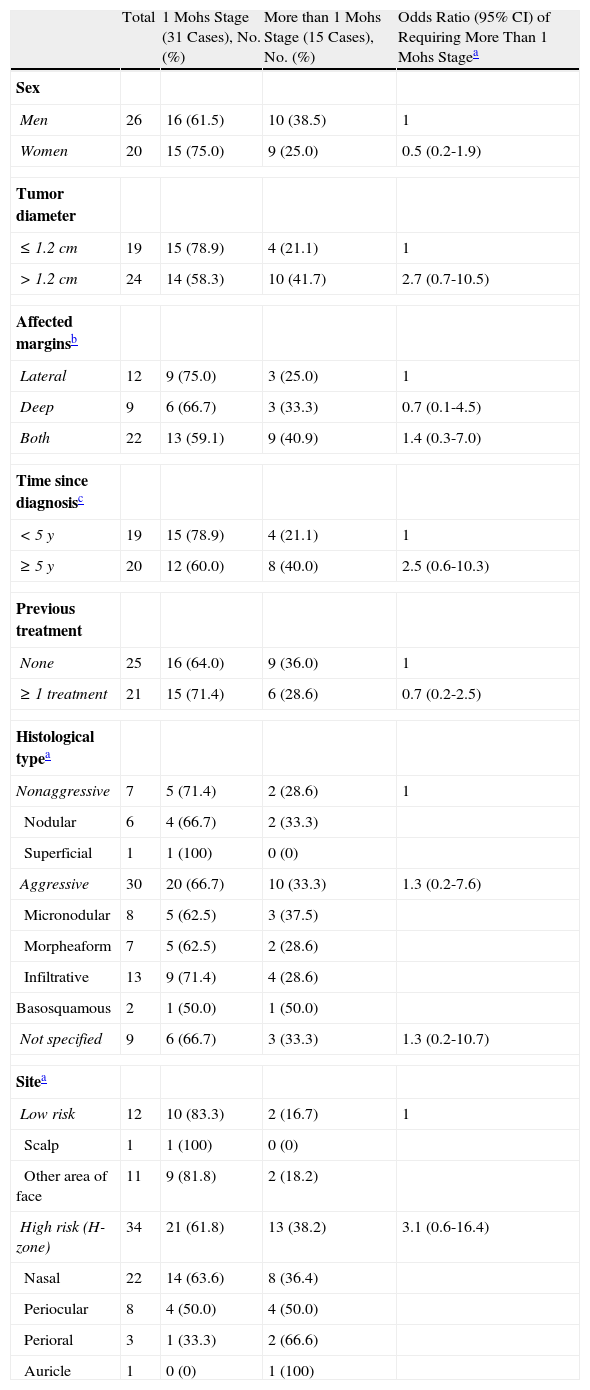
The second analysis was performed to determine if there were any variables that could establish the need for only a single stage of Mohs surgery to achieve tumor-free margins. The results of this analysis are presented in Table 3. Of the 46 patients in the study, 31 (67.4%) required a single stage of Mohs surgery to achieve tumor-free surgical margins. Of this group, only 7 presented residual tumor in the paraffin-embedded samples. Once again, there were no statistically significant differences for any of the variables studied.
Analysis of the Relationship Between the Clinical-Pathological Features and the Number of Mohs Stages Necessary to Achieve Free Margins.
| Total | 1 Mohs Stage (31 Cases), No. (%) | More than 1 Mohs Stage (15 Cases), No. (%) | Odds Ratio (95% CI) of Requiring More Than 1 Mohs Stagea | |
| Sex | ||||
| Men | 26 | 16 (61.5) | 10 (38.5) | 1 |
| Women | 20 | 15 (75.0) | 9 (25.0) | 0.5 (0.2-1.9) |
| Tumor diameter | ||||
| ≤ 1.2cm | 19 | 15 (78.9) | 4 (21.1) | 1 |
| > 1.2cm | 24 | 14 (58.3) | 10 (41.7) | 2.7 (0.7-10.5) |
| Affected marginsb | ||||
| Lateral | 12 | 9 (75.0) | 3 (25.0) | 1 |
| Deep | 9 | 6 (66.7) | 3 (33.3) | 0.7 (0.1-4.5) |
| Both | 22 | 13 (59.1) | 9 (40.9) | 1.4 (0.3-7.0) |
| Time since diagnosisc | ||||
| < 5 y | 19 | 15 (78.9) | 4 (21.1) | 1 |
| ≥ 5 y | 20 | 12 (60.0) | 8 (40.0) | 2.5 (0.6-10.3) |
| Previous treatment | ||||
| None | 25 | 16 (64.0) | 9 (36.0) | 1 |
| ≥ 1 treatment | 21 | 15 (71.4) | 6 (28.6) | 0.7 (0.2-2.5) |
| Histological typea | ||||
| Nonaggressive | 7 | 5 (71.4) | 2 (28.6) | 1 |
| Nodular | 6 | 4 (66.7) | 2 (33.3) | |
| Superficial | 1 | 1 (100) | 0 (0) | |
| Aggressive | 30 | 20 (66.7) | 10 (33.3) | 1.3 (0.2-7.6) |
| Micronodular | 8 | 5 (62.5) | 3 (37.5) | |
| Morpheaform | 7 | 5 (62.5) | 2 (28.6) | |
| Infiltrative | 13 | 9 (71.4) | 4 (28.6) | |
| Basosquamous | 2 | 1 (50.0) | 1 (50.0) | |
| Not specified | 9 | 6 (66.7) | 3 (33.3) | 1.3 (0.2-10.7) |
| Sitea | ||||
| Low risk | 12 | 10 (83.3) | 2 (16.7) | 1 |
| Scalp | 1 | 1 (100) | 0 (0) | |
| Other area of face | 11 | 9 (81.8) | 2 (18.2) | |
| High risk (H-zone) | 34 | 21 (61.8) | 13 (38.2) | 3.1 (0.6-16.4) |
| Nasal | 22 | 14 (63.6) | 8 (36.4) | |
| Periocular | 8 | 4 (50.0) | 4 (50.0) | |
| Perioral | 3 | 1 (33.3) | 2 (66.6) | |
| Auricle | 1 | 0 (0) | 1 (100) | |
Tumors of 1.2cm diameter or less required only 1 Mohs stage in 78.9% of cases, compared to 41.7% of cases in which the tumor was greater than 1.2cm. Similarly, the need for only 1 Mohs stage was much more common (78.9%) in tumors diagnosed less than 5 years earlier. Of the tumors situated in the area of the nose, 63.6% required only 1 stage of Mohs surgery, compared to 50% of the lesions in the periocular area. The most marked difference was observed between tumors in the H-zone of the face (periocular, perioral, nasal, or periauricular) and those in other areas of the face. Of the tumors in these other areas, 83.3% presented tumor-free margins after 1 Mohs stage compared to 61.8% of tumors in the H-zone.
No differences in the number of stages necessary to achieve tumor-free margins were detected on comparing the number of previous treatments or the type of treatment performed.
When only the lateral margin was affected, 75% of cases required a single Mohs stage, compared to 66.7% when only the deep margin was affected and 59.1% when both margins were involved.
Comparison of the histological types of BCC revealed no marked differences, although the histological type that most frequently required more than 1 stage was micronodular BCC (37.5%). When the histological types of BCC were grouped into high grade and low grade, it was found that 33.3% of the high-grade tumors required more than 1 Mohs stage compared to 28.6% of low-grade tumors; this difference was not statistically significant.
DiscussionBCC is a skin tumor that usually requires surgical excision to achieve complete cure. It is not rare to see cases of incompletely excised BCC; incomplete excision can occur in lesions located in complicated sites or with histological types that make it difficult to accurately evaluate the true extension of the tumor.4 Involvement of the margins is most common in tumors of the morpheaform type situated on the face, particularly in the nasal and perioral areas.4 Depending on the study, recurrence occurs in 10% to 67% of BCCs at these sites, independently of the histological type.1–3,5–8,11 In view of the above, dermatologists considered that it could be reasonable to perform follow-up of some cases seen in normal daily practice, without subjecting the patient to further surgery. The absence of recurrence has been attributed, at least in part, to the postoperative healing process, which could destroy small tumor foci in the surrounding tissue. Despite this, the high recurrence rate (over 50%) among reoperated recurrent tumors on sites such as the face suggests a need for additional treatment.9,10
We found no factors likely to predict a subgroup of BCCs in which simple excision or even just clinical follow-up would be certain to be sufficient, at least in the area of the face and scalp. This study has an obvious selection bias as the patients referred to our center as candidates for Mohs surgery have 1 or more risk factors that indicate the use of this technique. It is likely that, in a series of unselected patients, it would be possible to define a low-risk subgroup (for example, patients with nodular or superficial tumors on the back) in which a conservative approach or conventional surgery could be used, as has been suggested by other authors.11 In addition, our sample size was small, reducing the likelihood of finding statistically significant differences.
Although the results obtained do not allow us to confirm our initial hypothesis, they do show interesting trends that could help to identify characteristics of excised tumors with positive margins that might indicate more conservative therapeutic approaches at other sites. First, the histological type of tumor that most frequently presented residual tumor was the micronodular BCC, whereas the other types (morpheaform and infiltrative) showed similar frequencies in terms of the presence and absence of residual tumor. This may appear paradoxical, as the infiltrative and morpheaform types tend to extend beyond what is clinically visible, and in other studies the morpheaform type has been most frequently associated with affected margins after excision.4 However, the initial treatment of the infiltrating and morpheaform tumors in our study sample was probably more aggressive, with wider surgical margins from the outset, and residual tumor may therefore have been minimal and easily destroyed during the healing process. There is also the possibility that different specialists were involved in the treatment of the tumor, a factor we were unable to evaluate as this information was not included in the Mohs surgery database of the department. The opposite may be true in the micronodular type, in which a less aggressive initial treatment could have led to the higher index of residual tumor than in other tumor types. However, it should not be forgotten that the presence of an aggressive histological type (morpheaform, micronodular, infiltrative, or basosquamous) is the most important predictive factor of recurrence in patients with recurrent BCC treated using Mohs surgery.14
With regard to the site of the tumor, we observed that tumors situated in the perioral and periocular areas had a higher frequency of residual disease than tumors on other areas of the face. This is probably because the perioral and periocular areas are surgically more complicated, and the cosmetic and functional results are very important, leading to the excision of a smaller amount of tissue in order to save healthy tissue and leave a smaller surgical defect. This aspect is particularly relevant because the periocular area, especially around the medial canthus of the eye, is one in which recurrence can be very problematic.15 This underlines the need in oncologic surgery to prioritize elimination of the whole tumor and to achieve tumor-free margins before looking to achieve a cosmetically acceptable functional result. However, none of the factors studied enabled us to define which subgroup of tumors could be treated using conventional surgery.
The second study objective was to predict which tumors should undergo re-excision using Mohs surgery and in which tumors simple re-excision with narrow margins might be sufficient. As with the previous objective, the results obtained only enable us to report trends, though again we consider it interesting to discuss these trends despite the absence of firm conclusions. The first point that stands out is the large number of cases that required only 1 Mohs stage to achieve negative surgical margins. Thirty-five patients (76%) would not have required Mohs surgery as simple excision with a narrow margin would have been sufficient.
Negative surgical margins were more likely to be achieved after a single Mohs stage in tumors with a diameter of less than 1.2cm and a time since diagnosis of less than 5 years, and tumors situated away from the high-risk areas of the face (nasal, periocular, and perioral regions and the scalp and ear).
Our initial hypothesis was that there would be factors that could help to choose the best therapeutic approach in BCCs on the head with positive surgical margins after a previous excision. A further aim was to determine which tumors of those requiring surgery would benefit from Mohs surgery and which could be treated by simple excision. Despite the small sample size, the fact that none of the characteristics was associated with a percentage of close to 100%, for either the absence of residual tumor or the achievement of negative margins with a single Mohs stage, would suggest that there is no single characteristic that defines a subgroup of cases in which conventional surgery could guarantee complete cure in the majority of the cases.
In conclusion, the trends observed, together with a critical and in-depth analysis of the literature, reviewed in detail in an article published in Actas Dermosifiliográficas by Dr. Ríos-Buceta,11 enable us to establish rational approaches to previously excised BCC with positive margins. By extrapolating the results to other, clinically less important sites, such as the back, certain criteria can be put forward to help decide which tumors might be adequately re-excised by conventional surgery or simply be closely monitored. The characteristics associated with a lower risk are tumor diameter less than 1.2cm and a time since diagnosis of less than 5 years. Conventional surgery may also be a reasonable option for BCCs on the head but away from the high-risk areas. In contrast, Mohs surgery would appear to be the treatment of choice in previously excised BCC with positive margins in the high-risk areas of the face, independently of the pathological or temporal characteristics of the tumor.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Angulo J, et al. Re-exéresis mediante cirugía de Mohs de carcinomas basocelulares de la cabeza previamente extirpados con afectación de márgenes. Actas Dermosifiliogr.2011;102:797-804.