The minimal erythema dose (MED), an essential measurement in studies of skin photosensitivity, requires establishing MED values for specific populations, given genetic variation. Different ways to assess erythema are also relevant. We aimed to determine MED values in a sample of Colombian patients and correlations between MED and Fitzpatrick skin type. We also studied concordance correlation between MEDs and two alternative ways to assess erythema.
Patients and methodsCross-sectional study of 113 individuals in Bogotá, Colombia. We used a solar simulator to measure UV-A radiation and combined UV-A and UV-B (UVA+UVB) radiation, for MED calculation. Narrowband UV-B (NBUVB) radiation was measured in a phototherapy cabin. Erythema was assessed visually and with a Mexameter MX 18 device.
ResultsThe median MEDs of UVA+UVB radiation were 22mJ/cm2 for Fitzpatrick skin types I and II, and 33 and 43mJ/cm2, respectively, for skin types III and IV. The MEDs of UV-A radiation were 22, 42, 86, and 100J/cm2 for skin types I, II, III, and IV, respectively. The MEDs of NBUVB radiation were 390, 550, 770, and 885mJ/cm2 for the 4 skin types. The correlation between MEDs and skin types ranged from 0.5 to 0.69. Lin's concordance correlation coefficients between visual and Mexameter assessments of erythema were greater than 0.8 in all cases.
ConclusionThis study allowed us to understand MED values for UV-A, UVA+UVB, and NBUVB according to different skin types in the Colombian population. Concordance correlation coefficients between the different methods of erythema assessment were very good. Correlations between MEDs and skin types were moderate to good.
La determinación de la dosis eritematosa mínima (DEM) es necesaria para el estudio de la fotosensibilidad cutánea, debe determinarse en cada población, dadas las diferencias genéticas y las metodologías utilizadas. El objetivo de este estudio fue determinar la DEM en población colombiana, su correlación con los fototipos y la concordancia de dos alternativas de medición.
Pacientes y métodosEstudio de corte trasversal que incluyó 113 personas en Bogotá (Colombia). Se determinó la DEM para UVA+UVB y UVA utilizando un simulador solar y para UVB de banda estrecha (UVBBE) con una cabina de fototerapia. La evaluación se realizó visualmente y por Mexameter MX®-18.
ResultadosLa mediana de la DEM para UVA+UVB fue de 22mJ/cm2 para fototipos I y II y de 33 y 43mJ/cm2 para fototiposIII y IV, respectivamente; para UVA fue de 22, 42, 86 y 100J/cm2 y para UVBBE de 390, 550, 770 y 885mJ/cm2 (fototipos I-IV, respectivamente). La correlación entre los fototipos y la DEM osciló entre 0,5 y 0,69. El nivel de correlación-concordancia de LIN entre el método visual y el Mexameter fue superior a 0,8 en todos los casos.
ConclusionesEste estudio permitió conocer los valores de DEM para UVA+UVB, UVA y UVBBE para los diferentes fototipos en la población colombiana, y evidenció una correlación muy buena entre los métodos de medición evaluados y una correlación moderada a buena entre la DEM y los fototipos.
Evaluation of skin sensitivity to UV radiation is a key component of the assessment of cutaneous photosensitivity, which is essential in the case of photodermatosis, photocarcinogenesis, sun protection, and use of phototherapy.1,2 One of the most commonly used parameters for measuring sensitivity is the determination of the minimal erythema dose (MED), which is defined as the minimum dose of UV radiation capable of inducing perceptible erythema in the skin. It is usually evaluated 24hours after irradiation.3,4
Visual detection of the MED is subjective, and its value can be affected by various factors, such as the light source, the increments used, the area irradiated, previous exposure to UV radiation, the definition of the MED, skin temperature, and intraobserver and interobserver variability.2 Differences in ethnicity also affect variability in the detection of the MED; therefore, measurement must be validated for the specific population.
Potential sensitivity to UV radiation can be evaluated using indirect methods without having to measure the MED. The most widely used is the Fitzpatrick skin type scale,5 although the reliability and validity of this system have been called into question, mainly because it is subjective and prone to recall bias.2,6,7 Nevertheless, Sánchez et al.8 suggest that the scale can prove to be reliable insofar as the evaluation method of this approach can be standardized.
In several countries, the MED has been determined taking into account the skin type, and some studies have shown that there is no favorable correlation between these variables.6,9–12 In Colombia, the only published study was performed in schoolchildren and did not find a correlation between MED for UV-B and phototype.12
Cutaneous erythema has been assessed more objectively using various instruments, including the tristimulus colorimeter (chromameter) and the narrowband simple reflectance spectrophotometer (Mexameter MX 18), which correlate well with the visual evaluation.13,14
The objective of the present study was to determine the MED for UV-A+UV-B, UV-A, and narrowband UV-B in a group of Columbian individuals with different skin types, the degree of correlation between MED and the skin types, and the degree of concordance and correlation between the 2 assessment methods (visual assessment and Mexameter MX 18).
MethodsDesign, Population, and SampleWe performed a cross-sectional study to evaluate the sensitivity of the skin to UV radiation in terms of the MED value in a sample of Colombian patients and determined the concordance and correlation for 2 methods of measuring MED, namely, visual assessment and Mexameter MX 18 (Courage Khazaka Electronic). The Mexameter MX 18 device is a spectrophotometer that measures absorption of light on 2 wavelengths, 568nm for hemoglobin and 660nm for melanin, yielding an erythema index and a melanin index. We used a sequential convenience sample of healthy individuals aged >18 years who were seen at Hospital Universitario Centro Dermatológico Federico Lleras Acosta, Bogotá, Colombia and gave their consent to participate in the study. We excluded patients who had taken systemic photosensitizing medication during the 2 months before initiation of the study, topical corticosteroids during the previous 8 days, and those who had taken oral antihistamines during the previous 2 days. We also excluded patients with a personal or family history of photosensitivity, those whose backs had been exposed to natural or artificial solar radiation during the 6 weeks before the study, and foreigners and children of foreign parents.
The sample size was calculated using the formula proposed for estimation of concordance and correlation in cross-sectional studies, which is based on ordinal and continuous data,15 taking into account an alfa of .05, an expected accuracy of 10%, and a correlation coefficient of 0.8 (according to a pilot study developed by the researchers). Based on the above, we calculated a sample size of 75 persons for determination of the MED for UV-A, UV-A+UV-B, and narrowband UV-B and for evaluation of the 2 techniques for measuring MED. All study procedures were approved by our institutional review board and were consistent with the recommendations of the Declaration of Helsinki.
Procedure for Evaluating MEDEach participant was evaluated using the Fitzpatrick skin type scale.5 The skin on the back was then irradiated with 20% increases in the dose of UV-A+UV-B (skin types I–II, 15–43mJ/cm2; and skin types III–IV, 30–72mJ/cm2), UV-A (skin types I–II, 20–50J/cm2; and skin types III–IV, 42–100J/cm2), and narrowband UV-B (skin types I–II, 50–550mJ/cm2; and skin types III–IV, 100–970mJ/cm2). UV-A+UV-B and UV-A were administered using a 300-mw solar simulator (Model 601 Multiport, Solar Light), which has 6 liquid light guides measuring 9mm each. Narrowband UV-B was administered using a phototherapy cabin (Daavlin, 305/350), with a potency of 4.3mW/cm2 at a distance of 15cm after placing a 4-layer white plastic mold with 8 fields, each measuring 1cm2, on the skin of the back. The rest of the body surface and the face were covered with a thick material that did not allow UV radiation to penetrate, and the participant wore photoprotective eyewear. The radiation doses were measured using a PMA-2100 dosimeter and its respective detectors (SUV PMA2103 and UVA PMA2113) in the case of the solar simulator (calibrated by Solar Light) and with an IL-1700 radiometer and its detector for narrowband UV-B (International Light) in the case of the phototherapy cabin.
MED was read at 24hours after irradiation, taking into account the lowest dose of radiation with which minimum perceptible erythema was achieved. The readings (visual and Mexameter MX 18) were taken by 2 trained observers. In the case of Mexameter MX 18, a total of 3 readings were taken by pressing the handheld unit against the nonradiated skin, and 3 readings were taken for each irradiated field; an average was then calculated. If erythema was not achieved, the procedure was repeated with geometrically increasing doses. The MED value taken using the Mexameter MX 18 was determined by a physicist and corresponded to the dose with which the maximum slope on the dose-response curve was obtained for each individual, based on a previously published method.16 The maximum UV-A dose administered with the solar simulator was 100J/cm2; for purposes of the analysis, persons for whom no erythema was achieved with this dose were arbitrarily assigned an MED value of 120mJ/cm2.
Statistical AnalysisA descriptive analysis was performed for each of the variables using the most appropriate summary statistics. Categorical variables were presented as frequency tables with absolute and relative values (sex and skin type). Given that the data were nonnormally distributed for MED (UV-A+UV-B, UV-A, and narrowband UV-B, visual and Mexameter MX 18 measurements), the variables were expressed as median (interquartile range [IQR]). The correlation between the skin type and the MED value, in all its different modalities, was evaluated using the Spearman correlation coefficient, with its respective 95% CI and P value. Furthermore, in order to evaluate the degree of concordance and correlation between the different MED values, we used the Lin concordance correlation coefficient, which was reported with its 95% CI and P value. The analysis was performed using Stata 14.
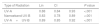
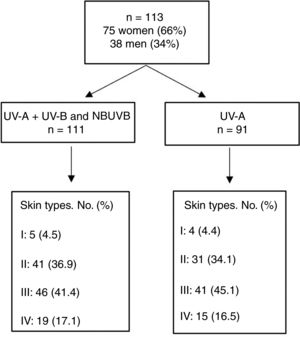
ResultsThe study population comprised 113 participants with a median age of 27 (18–56) years; of these, 66% were women. No participants had skin types V or VI. Fig. 1 shows the total number of individuals and their distribution by skin type. MED was evaluated for UV-A+UV-B and narrowband UV-B in 111 participants and for UV-A alone in 91 owing to difficulties in remaining for the time necessary to undergo the test. Erythema was not observed at the maximum dose of UV-A administered (100J/cm2) in 21 of the 91 cases (3 were skin type II, 7 skin type III, and 11 skin type IV), and in 14 participants, Mexameter MX 18 did not detect erythema (1 was skin type II, 7 skin type III, and 6 skin type IV). Table 1 and Fig. 2A–C show the median (IQR) MED by skin type and assessment method.
Skin Types and MED (UV-A+UV-B, UV-A, and Narrowband UV-B) Assessed Visually and by Mexameter.
| Type of Radiation | Skin Type I | Skin Type II | Skin Type III | Skin Type IV | ||||
|---|---|---|---|---|---|---|---|---|
| MedianVIS/MEX | IQRVIS/MEX | MedianVIS/MEX | IQRVIS/MEX | MedianVIS/MEX | IQRVIS/MEX | MedianVIS/MEX | IQRVIS/MEX | |
| UV-A+UV-B | 22/27 | 15/12 | 22/22 | 12/12 | 33/30 | 13/6 | 43/43 | 26/26 |
| UV-A | 22/24 | 6.5/8.5 | 42/42 | 21/18 | 86/60 | 70/36 | 100/100 | 48/48 |
| Narrowband UV-B | 390/390 | 160/0 | 550/550 | 380/160 | 770/590 | 420/220 | 885/770 | 330/470 |
Abbreviations: IQR, interquartile range; MEX, Mexameter MX 18; VIS, visual.
A–C, Box and whisker plots for UV-A+UV-B (MEDTOT), UV-A, and narrowband UV-B (NBUVB) for the MED values measured visually and using Mexameter MX 18 for skin types 1 to 4. Note the progressive increase in the median value, especially from skin type 2 to skin type 4. D–F, Diagrams showing the concordance-correlation coefficient between the visual measurement and measurement by Mexameter MX 18. Note the good correlation for the different wavelengths. MED indicates minimum erythema dose; NBUVB, narrowband UV-B.
In order to compare our findings with the literature on this subject, we calculated the mean MED assessed visually, even though the sample was not normally distributed (Table 2).
Skin Types and Mean MED (UV-A+UV-B, UV-A, and Narrowband UV-B) Assessed Visually.
| Type of Radiation | Skin Type I | Skin Type II | Skin Type III | Skin Type IV | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| UV-A+UV-B | 22 | 7.5 | 24 | 11.4 | 36 | 10.5 | 48 | 14.9 |
| UV-A | 21 | 4.3 | 44 | 27.3 | 81 | 31.4 | 95 | 26.9 |
| Narrowband UV-B | 498 | 167.1 | 593 | 225.5 | 765 | 205.6 | 946 | 275.7 |
We evaluated the correlation between skin types and each of the MED values (UV-A+UV-B, UV-A, narrowband UV-B), both visually and with the Mexameter MX 18. The correlation observed ranged from 0.5 to 0.69. The lowest correlations were recorded for narrowband UV-B, both visually and with Mexameter MX 18 (0.5 and 0.53, respectively). Table 3 shows the correlation coefficient obtained for each value with its P value.
Correlation Between Skin Type and MED.
| Spearman | P value | |
|---|---|---|
| MED UV-A VIS | 0.64 | <.001 |
| MED UV-A MEX | 0.69 | <.001 |
| MED narrowband UV-B VIS | 0.50 | <.001 |
| MED narrowband UV-B MEX | 0.53 | <.001 |
| MED UV-A+UV-B VIS | 0.66 | <.001 |
| MED UV-A+UV-B MEX | 0.64 | <.001 |
Abbreviations: MED, minimum erythemal dose; MEX, Mexameter MX 18; VIS, visual assessment.
The degree of concordance and correlation for each MED value was calculated according to whether it was assessed visually or using Mexameter MX 18. The Lin concordance correlation coefficient was greater than 0.8 in all cases (Table 4 and Fig. 2D–F).
DiscussionIn this study, we determined the MED for UV-A, narrowband UV-B, and UV-A+UV-B in a sample of the Colombian population. Investigations based on a solar simulator revealed that the mean MED of UV-A+UV-B for the different skin types varies; however, the values for skin types I to IV in this study population were similar to those reported by Pérez-Ferriols et al.17 in Spain, probably owing to the fact that our population comprises people of Spanish descent as a result of genetic admixture.18 In a study carried out in India, the mean MED value for skin type IV was similar to the results for this skin type in Spain and in the present study.19 For skin type III, the mean MED was similar in Australian Asians,20 Spaniards,17 and Colombians. In China, the mean MED values by skin type are much higher,21 probably because the study was based on buttock skin, which is less sensitive than that of the back,9,22 and to genetic differences (Table 5).
Mean MED Values (UV-A+UV-B) in Studies Performed With a Solar Simulator.
| Country | Skin Type | No. | MED UV-A+UV-B | Irradiated Skin | |
|---|---|---|---|---|---|
| mJ/cm2 | SD | ||||
| India20 | IV | 41 | 51.2 | 5.88 | Back |
| China21 | II | NR | 64 | 22.2 | Buttocks |
| III | 66.3 | 17.1 | |||
| IV | 77.4 | 17.4 | |||
| Australian Asians20 | II | 2 | 39 | NR | Back |
| III | 17 | 37.6 | |||
| IV | 11 | 61 | |||
| Spain17 | I | 4 | 23 | 8 | Back or buttocks |
| II | 89 | 28 | 4 | ||
| III | 108 | 35 | 4 | ||
| IV | 31 | 51 | 6 | ||
| Colombia (present study) | I | 5 | 22 | 7.5 | Back |
| II | 41 | 24 | 11.4 | ||
| III | 48 | 36 | 10.5 | ||
| IV | 19 | 49 | 14.9 | ||
The mean MED value for skin types I–IV in studies carried out with other sources of UV-B (fluorescent UV-B lamps) in Brazil,11 in the USA,23 and for some skin types in the UK9 is similar to that of our population for UV-A+UV-B. In contrast, mean MED values in Korea,6 and more particularly, Singapore,24 are much higher for the same skin types (Table 6). These differences could be explained by genetic variability and because the skin irradiated in Singapore was on the buttocks.
Mean MED Values With Other UV-B Sources.
| Country | Skin Type | No. | MED UV-B | Site Irradiated | |
|---|---|---|---|---|---|
| mJ/cm2 | SD | ||||
| Korea6 | I | 10 | 59 | 17.9 | Back |
| II | 7 | 72.9 | 11.1 | ||
| III | 46 | 72.4 | 31 | ||
| IV | 34 | 69.4 | 30.8 | ||
| Singapore24 | II | 6 | 79 | 27 | Buttocks |
| III | 36 | 108 | 43 | ||
| IV | 32 | 163 | 50 | ||
| United Kingdom9 | I | 7 | 30 | 15 | Back |
| II | 11 | 25 | 10 | ||
| III | 12 | 21 | 7 | ||
| IV | 6 | 49 | 9 | ||
| United States of America23 | I | 39 | 29 | 11.9 | Buttocks |
| II | 163 | 36 | 12.8 | ||
| III | 146 | 43 | 17.6 | ||
| IV | 58 | 58 | 23 | ||
| Brazil11 | I | 30 | 14.8 | 2 | Infraaxillary |
| II | 35 | 26.8 | 5.8 | ||
| III | 35 | 30.8 | 5.1 | ||
| IV | 31 | 41.7 | 8 | ||
| Colombia12 | I | 2 | 35 | 21 | Back |
| II | 23 | 56 | 9 | ||
| III | 51 | 70 | 14 | ||
| IV | 20 | 84 | 10 | ||
If we compare the results of the present study with those reported from Medellin, Colombia,12 we see that in the latter the mean MED value by skin type was higher, probably because the definition of MED used was the minimum dose that led to erythema with well-defined borders.
Our literature review revealed few publications on MED values for UV-A, perhaps because of the difficulty obtaining a UV radiation source that emitted high doses of UV-A over short periods. The median MED values for UV-A in the present study, with the ranges obtained by Fitzpatrick,5 are similar for types I (22 vs 20–35J/cm2) and II (42 vs 30–35J/cm2), although they are higher for types III (86 vs 40–55J/cm2) and IV (100 vs 50–80J/cm2).
As for narrowband UV-B, the mean values for the Spanish population17 (obtained by applying a conversion factor to the MED results for UV-B) are similar to those of the present study for all skin types. In Detroit, USA, Carretero-Mangolis and Lim25 reported that the median MED was 600mJ/cm2 for skin types I-II and 700mJ/cm2 for skin types III-IV; both of these values are similar to those reported in the present study, that is, 550 and 770mJ/cm2, respectively. In 352 patients with psoriasis in the UK, the median MED values by skin type were lower: 200, 280, 390, and 550mJ/cm2 (skin types I–IV, respectively).26
Consistent with reports from other authors,2,11,12,24 we found that MED tended to increase with the skin type. However, the Fitzpatrick skin-type scale is not sufficient to distinguish well between values. In fact, MED values for UV-A+UV-B, UV-A, and narrowband UV-B overlap in different skin types, so that 2 people could have the same MED value but belong to different skin types.2,6,25,27,28
Some authors report no correlation between MED and skin type,6,9,12,29 whereas others do.11,24,30,31 After exploring this association, the present study found a correlation that can be classed as good for UV-A and UV-A+UV-B and moderate for narrowband UV-B.
The concordance correlation coefficient for MED assessed visually and using Mexameter MX 18 was very good for UV-A+UV-B, UV-A, and narrowband UV-B, as shown elsewhere.13,14 Taking these results into account, both forms of measurement are interchangeable; consequently, visual determination continues to be useful in clinical practice.
The limitations of the present study are its small sample size, especially in the case of skin type I, and the fact that the sample is not representative of the whole Colombian population, since we were unable to include individuals with skin types V and VI, who live in other geographic areas of the country. Furthermore, some individuals did not develop erythema at the maximum dose of UV-A administered (100mJ/cm2), sofor the data analysis, we assumed an MED value of 120J/cm2, which may not correspond to the real MED of these subjects.
ConclusionIn this study, where MED was determined for UV-A+UV-B, UVA, and narrowband UV-B in a group of Colombians with skin types I–IV, we found that MED values overlapped for different skin types. We also recorded a moderate to good correlation with the skin types and a good correlation between visual measurements and those obtained using an objective method (i.e., Mexameter MX 18).
FundingThis study was funded by Hospital Universitario Centro Dermatológico Federico Lleras Acosta, Bogotá, Colombia.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Valbuena MC, Nova Villanueva JA, Sánchez Vanegas G. Dosis eritematosa mínima: correlación con el fototipo y método de medición en una muestra de población colombiana. Actas Dermosifiliogr. 2020;111:390–397.