Argyria is a rare disease caused by silver deposition in the body. Most reports of occupational argyria in the literature describe the generalized form.1 We report on 2 patients who developed localized argyria after more than 30 years of contact with silver. The clinical appearance of these lesions requires us to make a differential diagnosis including deep melanocytic lesions, especially melanoma metastases.
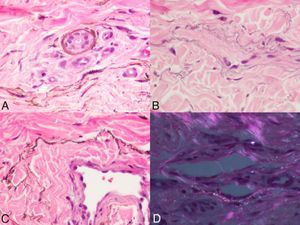
The first patient was a 75-year-old man with no previous history of interest who presented with asymptomatic blue macules that had begun to appear 5-10 years previously on the dorsum of the fourth finger of the right hand and on the palmar surface of the fifth finger of the right hand (Fig. 1, A and B). Dermoscopy revealed lesions with a homogeneous blue pattern (Fig. 1C). The second patient was a 70-year-old man who also presented with blue-gray macules on the dorsum of both hands that had begun to appear 5 years previously (Fig. 1D). Biopsy disclosed multiple dark brown strands and granules with a periadnexal distribution around the secretory coils of the sweat glands and an interstitial distribution with deposits along the elastic fibers of the dermis (Fig. 2, A, B, and C). Staining for melanocytes was negative. Dark-field microscopy revealed characteristic brilliant specks (Fig. 2D). After more exhaustive questioning, both patients stated that they had worked as jewelers for more than 30 years and habitually handled silver. They were diagnosed with localized cutaneous argyria and, after opting not to receive treatment, remain under follow-up. Two years after diagnosis, no changes have been detected in the lesions.
A and B, The first patient presented several blue-gray macules on the dorsum of the fourth finger of the right hand and on the palmar surface of the fifth finger of the right hand. C, Dermoscopy revealed a homogeneous blue-gray pattern. D, The second patient presented similar lesions on the dorsum of both hands.
Histology revealed the presence of dark brown strands and granules with a periadnexal distribution (A) and along the elastic fibers to create an image resembling chains of streptococci (B and C) (hematoxylin-eosin, original magnification ×200). Dark-field microscopy shows the characteristic “starry sky” image (D).
Argyria is an uncommon condition today, especially since silver-containing systemic medication, which was once used to treat a variety of conditions (including syphilis), is no longer prescribed.2 Nevertheless, a series of mechanisms has been described in recent years by which silver can unintentionally enter the body through the skin, including the use of earrings, body piercing, dental amalgam, topical silver salts, or acupuncture needles.2–9 Prolonged occupational exposure to silver occurs in individuals working in the manufacturing industry and photographic processing, as well as silversmiths and goldsmiths.10,11
Clinically, argyria is classed as generalized or localized. Generalized argyria is produced by the ingestion or inhalation of silver compounds that subsequently reach internal organs and the skin, where they cause permanent diffuse blue-gray coloration in photoexposed areas.
Localized argyria is caused by direct external contact with silver; the most commonly affected areas are the hands, eyes, and the mucosas. The mechanism of penetration is unknown, although it is thought to be via the eccrine sweat ducts, since the metal is most concentrated around the secretory portion of the gland.1 The fact that accumulation of silver does not respond to chelators, as well as the relatively low frequency of systemic argyria in patients with intact skin who come into contact with silver, suggests that silver is deposited in the dermis in a chemically stable and apparently inert form.1,4 Physical examination reveals multiple asymptomatic blue-gray macules with a nonspecific homogeneous blue pattern on dermoscopy. Histology reveals apparently normal skin. However, increased magnification reveals multiple brown-gray strands and granules distributed between collagen fibers, within histocytes, in the basement membrane of the eccrine sweat glands, and along the elastic fibers of the dermis in a pattern that resembles chains of streptococci. Under polarized light microscopy, the metallic granules are brilliantly refractile and produce the characteristic “starry sky” image.1 In chrysiasis (gold deposits in tissue), the granules are typically larger and present red-orange birefringence. Bismuth deposits are positive on Christeller-Komaya staining. The definitive diagnosis is made using electron microscopy, x-ray microanalysis, or other more complex histochemical methods that make it possible to identify the chemical composition of the granules.1
In conclusion, we present 2 cases of localized occupational argyria occurring after years of exposure to silver products. The clinical appearance and dermoscopy findings required other blue-colored lesions, particularly melanoma metastases, to be ruled out. Argyria is probably underdiagnosed, and some authors report that up to 40% of exposed individuals can eventually develop the condition.1 A detailed history will help to orientate the diagnosis.
We are grateful to Dr Victor Alegre de Miquel for his valuable contribution to the description of the histopathology findings.
Please cite this article as: Garcias-Ladaria J, et al. Argiria cutánea localizada. A propósito de 2 casos. Actas Dermosifiliogr. 2013;104:253–4.