Lichen striatus (LS) is an uncommon asymptomatic acquired dermatosis that mainly affects children.
The diagnosis is usually clinical, as the histologic findings are variable and depend on the phase of the disease. It presents with flat-topped, desquamating erythematous papules with a linear distribution along the Blaschko lines (Fig. 1).
A possible association with atopic dermatitis has been suggested.1–5 We designed this retrospective study in order to describe the characteristics of children with this disease and to determine whether a higher prevalence of atopic dermatitis existed in our population.
We present a case series of children diagnosed with LS at our centre in Valencia, Spain, from January 2008 to the present time, including all patients under 18 years old with compatible clinical manifestations.
Socio-demographic, clinical, histological, and therapeutic variables were analyzed, as well any relationship with possible triggering factors, including in particular atopic dermatitis, diagnosed in accordance with the Hanifin and Rajka criteria.
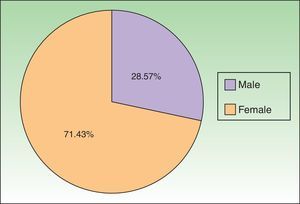
A total of 35 patients were included in the study. The mean age was 5 years and there was a predominance of female (Fig. 2).
Only 3 diagnostic biopsies were required in cases with atypical clinical manifestations. In the other patients, the characteristics of the lesions were consistent with LS and there was no need to perform an invasive procedure for confirmation.
The lesions were mostly asymptomatic (85.7%). When symptomatic, the most common complaint was pruritus (14.3%).
The site most frequently affected was the lower limbs (57.2%). None of the children presented associated onychodystrophy.
The majority of the lesions were managed with emollients and photoprotection (73.5%). Topical corticosteroids were used in the remaining patients.
Sixteen patients were lost to follow-up. None of those children were subsequently referred back to our department by their pediatrician or primary care physician for further follow-up. A complete response was achieved in all the other children except one who presented a partial improvement.
With regard to possible related factors, the medical histories of 2 patients revealed that the lesions appeared after a previous diagnosis of infection.
Nine patients presented a previous diagnosis of atopic dermatitis made by a specialist. In 5 patients, manifestations of atopy were found in the medical history (most frequently pityriasis alba) and in 1 patient a family history was found in first-degree relatives.
With respect to other related diseases, 9 children presented bronchial hyperreactivity (25.7%) and 3 patients had been diagnosed with some form of allergy.
Lichen striatus is an uncommon, asymptomatic acquired dermatosis that mainly affects children, with a predominance in female.1,2,6
The lesions do not usually produce symptoms, but when they are present, the most common is pruritus.6
This disease tends to resolve spontaneously in 6 to 24 months. In some cases a transitory residual hypopigmentation can remain. It is therefore useful to explain to patients and their parents that this is a benign condition, and to individualize therapeutic management.
Several authors have proposed seasonal changes as possible triggering stimuli, though there is no general agreement. Some of them report an increase in incidence of LS in summer,3,7 while others report the increase in autumn and winter.1 This observation has given rise to the association with infectious diseases as a triggering factor,8 nevertheless no relationship was found in our patients. In the series of 115 patients with LS studied by Patrizi et al.,1 only 3 children presented prodromal symptoms suggestive of viral infection. Because of that, this theory cannot be confirmed despite studying a larger number of patients.
Retrospective studies have highlighted the relationship between atopic dermatitis and LS,1–5 considering that the immune changes present in atopic dermatitis could be a predisposing factors for the induction of LS. Other authors, such as Happle,9 suggest that this disease should be included in the list of acquired disorders with a nevoid distribution/pattern and postulate that it could represent a mosaic form of atopic dermatitis.
Our series supports the findings of previous studies with a larger number of patients, in which atopic dermatitis could be considered to be a predisposing factors for LS.1
However, the results reported in the literature are based on retrospective studies, and prospective studies with a larger number of patients are needed to investigate the association of LS with triggering factors and concomitant diseases.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Briz MI, Santos-Alarcón S, Fuertes-Prosper MD, Mateu-Puchades A. Liquen estriado en la infancia. ¿Una entidad relacionada con la dermatitis atópica? Actas Dermosifiliogr. 2017;108:882–884.